INTRODUCTION
History
Features and epidemiology of OA in Japan
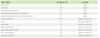
Major causative antigens
Examples of OA in Japan
Konjac asthma
Konjac asthma: Bronchial asthma that seemed to be triggered by Maiko was known among the residents near the konjac milling plant and its employees. The group from the First Department of Internal Medicine at Gunma University performed a detailed field survey at Shimonita in Gunma that identified asthma induced by inhaling Maiko powder, and they named this type of OA as "konjac asthma" and reported it in 1951 [4]. Konjac root is dried and ground into powder in the process of manufacturing the food known as konjac. Maiko is a fine konjac root powder that is blown by air pressure to obtain konjac powder for commercial use. Much of the Maiko powder is dispersed in the air and induces asthma in the plant workers by inhalation. The prevalence of konjac asthma was 16.6% among employees in konjac mills and the age of onset was mostly under 30 years [3].
Antigen: The purified antigen named Ag40D-2 is an acidic protein of about 24,000 daltons. Its ratio of basic to acidic amino acids is 1:3.7 and it induces a strong P-K reaction [7]. The amino acid composition of this antigen has also been determined [3, 8].
Specific IgE antibody: The immediate skin reaction to a purified Maiko powder antigen is positive in 100% of konjac asthma patients, but negative in non-konjac asthma patients. Konjac asthma patients always show a positive inhalation challenge test with Maiko powder, while control subjects are negative in all cases.
Hyposensitization therapy: When this type of asthma was discovered, konjac making was a key industry in the Shimonita area and 40% of the population were involved in producing konjac flour. Specific hyposensitization therapy was developed because of the difficulty in changing jobs. When its efficacy was assessed, it was remarkably effective in 6/35 persons (17.1%) and was effective in 18 (51.4%). The effect of hyposensitization therapy appeared after six months in early cases and after one year in most cases.
Sea squirt asthma
-
Sea squirt asthma is triggered by the inhalation of fluid from protochordate sea squirts that is adherent to cultured oysters [9]. Cultivation of oysters in the Hiroshima region has been done for 400 years and many people are engaged in the task of oyster husking. There were no reports before the second world war, but, employees complained of the onset of asthma associated with their work from around 1960. This asthma was reported at the annual congress of the Japanese Society of Allergology in 1963 by Mitsui et al. In addition, detailed studies revealed that this type of asthma was induced by the inhalation of sea squirt components adherent to oysters. Such OA was named sea squirt asthma in 1966 [9]. The cause of its onset was improved farming methods that allowed farming of oysters in deep water since around 1952, so that sea squirts became attached to the oysters. Because work was often done under rough conditions with poor ventilation, workers inhaled a lot of sea squirt components. The number of patients has recently shown a significant decrease due to improvement of the work environment.
From the investigation done at the time, the prevalence was 29% (443 out of 1,528 people) and it reached 45.8% in some towns. Because the industry mostly has female employees, there is a majority of female patients, but there is no gender difference in the prevalence. Half of the patients develop asthma within five years of starting work. Antigen: Separation and purification of sea squirt antigen was carried out and four antigens (H, Gi-rep, Ei-M, DIIIa) were identified [9]. Gi-rep and Ei-M were effective when used for hyposensitization therapy. The epitope is a five sugar alcohol: as GalNAcα1 → 2Fucα1 → 3 (GalNAcβ1 → 4) GlcNAcβ → 3GalNAc [10].
Specific antibody: The intradermal reaction to sea squirt antigen is positive in 91.3% of sea squirt asthma patients. When an antigen inhalation challenge test was done with sea squirt antigen, 4 out of 9 sea squirt asthma patients were positive.
Hyposensitization therapy: Initially hyposensitization therapy was done with the crude antigen and the efficacy rate was high at about 75%. However, hyposensitization therapy with the crude antigen caused side effects such as induction of asthma or urticaria. In contrast, therapy with the purified antigen has a higher efficacy rate of 91.5% and causes fewer side effects [9].
Characteristics of OA caused by chemicals
Exposure to high concentrations of chemicals may induce tissue damage and can cause bronchopneumonia.
Because of their low molecular weight, chemicals also reach other organs and induce an immune reaction that causes extrapulmonary lesions.
In the case of industrial antigens, unlike those in fields such as agriculture, avoiding exposure by career change is relatively easy. It may be that the estimated number of patients is lower than the actual number.
Identification is difficult because specific IgE cannot be detected.
New occupational antigens
Among high molecular weight antigens, there have been reports of OA due to new types of imported wood. A furniture craftsman developed asthma and the results of inhalation challenge tests showed that the causative antigen of his asthma was the dust of Albiza Falcataria (Falcata wood), which is a broad-leafed tree [11].
Among chemicals, there have been repor ts about occupational allergy induced by ortho-phthalaldehyde, which is used as a disinfectant solution for fiberscopes. Cases of ortho-phthalaldehyde-induced anaphylaxis began to be reported from around 2006. For example, anaphylaxis has been observed immediately after observation by a laryngeal fiberscope. Since various new chemicals will be developed in the future, we always need to pay attention to allergies caused by chemicals.
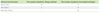
Diagnosis
Treatment
Avoidance of the causative antigen is most important. The incidence of allergic OA is greatly reduced by improving the work environment. Patients with konjac asthma in Gunma and sea squirt asthma in Hiroshima are rarely seen these days due to the development of environmental measures. When avoiding the causative agent is not possible, the physician should educate patients to reduce exposure by the use of protective equipment in the workplace. When workers are removed from their workplace to avoid exposure to antigens without economic support, they become impoverished and are unable to continue the treatment of their asthma. One third of patients with OA lose their jobs within six years of diagnosis in Western countries [13].
Drug therapy is the same as for the treatment of ordinary asthma.
Hyposensitization therapy is effective for patients who cannot change their job or have symptoms even after trying antigen avoidance and drug therapy. Our studies have shown that desensitization therapy with high molecular weight animal or plant antigens is very effective, and efficacy rate was 64.7%, 93.3%, 40.0%, and 91.5% for konjac asthma, sericulture asthma, flour asthma, and sea squirt asthma, respectively. However, desensitization to low molecular weight substances like chemicals and molds is not effective [3, 5].
Prognosis
Prevention
Guidelines for occupational allergic diseases in Japan
Problems related to OA in Japan
The Japanese Society of Allergology holds annual congresses, but symposiums on OA are not so frequent. They were held in Okayama in 1975, Maebashi in 1985, Nagasaki in 1990, Tokyo in 2003, Maebashi in 2004, and Tokyo in 2011. There is a lack of recognition regarding the importance of occupational allergy.
The work environment has improved in large enterprises under the direction of the government, but the smaller companies are not considered to have made enough effort in some cases.
Due to advances in medication, achieving control of symptoms medically tends to be emphasized and the search for causative antigens tends to be neglected. Thus, physicians often do not try to identify the causative antigen.
Action plan
Develop Japanese guidelines for the prevention and control of OA.
Develop a surveillance system to regularly check for OA among workers.
Build a system to share information about OA.
Share information on OA with other countries.
Provide education about OA to workers, employers, health care providers, and government agencies.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download