Abstract
Background
The effect of helminth infections on allergic diseases is still inconclusive. Furthermore, the effect of helminth infections on childhood allergic diseases in a tropical area where prevalence of helminth infections has undergone dramatic changes is not well documented.
Objective
To investigate the relationship between allergic diseases and helminth infection in a cohort of schoolchildren in an area that has undergone dramatic changes in intensity of helminth infections.
Methods
Children attending grade 5 were recruited from 17 schools in Western Province of Sri Lanka. They were assessed for allergic diseases using the International Study of Asthma and Allergies in Childhood questionnaire. Their serum total IgE (tIgE) and allergen-specific IgE (sIgE) for five common aeroallergens were measured by ImmunoCAP® method and stools were examined for the presence of helminth infections.
Results
A total of 640 children (mean age 10 years) were recruited to the study. Of them, 33.7% had evidence of allergic disease and 15.5% had helminth infections. Majority of infections (68.9%) were of low intensity. A significant relationship between allergic disease and helminth infections was not observed, however, a trend toward protective role of helminth infections against allergic diseases was noted. Multivariate analysis showed helminth infections to be an independent predictor of high tIgE levels whereas allergic disease was not. Allergic sensitization (atopy) was a significant risk factor for allergic disease only among non-infected children (odds ratio 3.025, p = 0.022) but not in infected children. The ratio of sIgE to tIgE was higher in non-infected children.
Among the various theories proposed to explain the alarming rise in allergic diseases around the world, the 'hygiene hypothesis' has gained much attraction [1]. This hypothesis attributes the rising incidence in allergic diseases to a reduction in childhood infections. Although it was first proposed almost two decades ago, it still holds merit as a biologically plausible explanation for the observed trend in allergic diseases. Numerous studies have demonstrated an inverse association between bacterial, viral infections and allergic diseases [2-4]. The role of helminth infections, the most common childhood infection in developing countries, is an area extensively investigated in the recent past. Unfortunately, the data are conflicting, interpretations have differed and many of the issues remain unresolved [5-7]. The type of helminth, the intensity and chronicity of the infection are some of the factors thought to affect the outcome in a population. The influence of helminthiasis on allergy has mostly been studied in areas where there is high burden of such infections [8, 9]. Communities in epidemiological transition from high burden of helminthiasis to light/moderate burden, provide a better opportunity to explore the relationship between helminth infection and allergy, especially in children, whose immune system has the greatest potential for modulation.
This study was carried out in Sri Lanka, a developing country in epidemiological transition with changing disease patterns, including allergy and helminthiasis. The objective was to explore the effect of helminth (Trichuris trichiura, Ascaris lumbricoides and hookworm) infections on allergic diseases in a cohort of primary school children.
The study was carried out in the Western Province of Sri Lanka, which has an area of 3,633 km2 and includes 3 districts (Colombo, Gampaha and Kalutara) that lie within the same ecological zone (Low Country Wet Zone). This province is the most highly populated of the nine provinces in the country: 28% of Sri Lanka's population of 19 million are residents of the Western Province. The ethical approval for this study was obtained from the Ethics Committee, Faculty of Medicine, University of Kelaniya, Ragama, Sri Lanka.
Details of the study population and subject selection have been reported elsewhere [10]. In brief, 640 children attending grade 5 (age group 9-11 years) in 17 schools in the Western Province were recruited to the study by stratified random sampling.
Data regarding allergic diseases were collected using the International Study of Asthma and Allergies in Childhood Phase III questionnaire translated into local languages. They were completed by the parent/guardian of selected children. The faecal samples provided by the children were examined on the day of collection using the modified Kato-Katz method [11], with kits obtained from Vestergaard Frandsen (India). According to the manufacturer's instructions, the egg count recorded in each positive sample was multiplied by a factor of 24 to obtain the number of eggs per gram faeces. Intensity of infection was categorized using the cut-off values recommended by the WHO [11]. When there was more than one helminth species, categorization was based on the higher intensity of infection.
Venous blood (5 mL) samples were collected from a sub-sample of children: from all the helminth-positive children who gave consent for the procedure and a comparative group of children who were helminth-negative and gave consent for venepuncture as the control group. Blood samples were centrifuged and serum was separated on the day of collection and stored at -70℃ until assayed for IgE. The ImmunoCAP® system, an enzyme immunoassay (Phadia, Sweden) was used to measure the serum total IgE (tIgE) and allergen-specific IgE (sIgE) for five aeroallergens: Dermatophagoides pteronyssinus, Blomia tropicalis, cat epithelium and dander, cockroach and grass pollen. These allergens were found to be the common sensitizing allergens in Sri Lankans (unpublished data).
For statistical analysis, atopy was defined as at least one positive test, i.e. sIgE value of ≥0.35 kUA/L for any allergen tested. Presence of eggs of any helminth (A. lumbricoides, T. trichiura or hookworm) in stool samples was considered as positive for these infections.
Interaction of atopic diseases, geohelminth infections, gender and tIgE were studied using the analysis of variance twoway procedure. A post hoc test was performed for individual comparisons when overall F-test indicated significant difference between mean values. The level of significance was set at p < 0.05. Logistic regression was used to determine the association between helminth infections, atopy and allergic diseases adjusting for the variables known to affect the outcome of the association.
The prevalence of allergic disease in this study population has been reported in detail previously [10]. In summary, the prevalence of asthma, rhinitis and eczema were 17%, 21.4%, and 5% respectively. 33.7% of the total study population had one or more allergic disease.
Overall, 15.5% (74/477) of children were found positive for any one or more of the helminths. Boys were more commonly infected than girls (19.1% vs. 11.3%, p = 0.019). The commonest infection was trichuriasis (14.3%), followed by ascariasis (4.2%) and hookworm (0.2%). Infection intensity was light in 51 children (68.9%), while 21 (28.4%) and 2 (2.7%) children had moderate and heavy infections respectively. Fifteen (20.3%) children had mixed infections of trichuriasis and ascariasis.
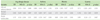
Among infected children, 49 (68.1%) did not have any allergic disease while 23 (31.9%) had evidence of one or more allergic disease (Table 1). There was no significant association between current infection and allergic disease, but overall trend is suggestive of a protective effect of helminth infections against the development of allergy (Table 2).
Serum analysis was done in a sub-sample of children (n = 203) selected as described above. Table 3 shows the baseline characteristics of the sub-sample. The geometric mean of tIgE in the study population was 686.6 kU/L [95% confidence interval (CI) 570.0 - 827.0]. A total of 159 children (78.3%) had total IgE level ≥ 200 kU/L, while 91 (44.8%) had ≥ 1,000 kU/L. The mean tIgE was not significantly different between boys (637.1 kU/L) and girls (796.5 kU/L) (p = 0.265), though girls had a higher value.
Helminth infections were significantly associated with tIgE levels in independent analysis (Table 4). The correlation coefficient between total egg count and tIgE was 0.336 (p < 0.001). Children infected with multiple helminth species had significantly higher tIgE levels than those who had monoinfection (2462.6 kU/L vs. 780.2 kU/L, p = 0.01).
A significant association between allergic disease and tIgE levels was observed in independent analysis and became non-significant when adjusted for helminth infection and sex. However, helminth infections remained significantly associated with tIgE levels, even when tIgE values were adjusted for allergic disease and sex (Table 4).
One hundred and sixty three children (80.3%) were found to be atopic, i.e. sensitized to at least one of the allergens tested. Mites (D. pteronyssinus 69.9%, B. tropicalis 84%) and cockroach (67.5%) were the most common sensitizing allergens in the study population. Although a higher proportion of boys (110/135, 81.5%) were sensitized than girls (53/68, 77.9%), the difference was not statistically significant (chi-square = 0.358, d.f. = 1, p = 0.549). Nor were sex-related differences observed for any of the allergens tested.
When children were analysed regardless of the infection status, atopy was a statistically significant risk factor only for rhinitis (Table 5). Moreover, when comparison was made between infected and non-infected children, atopy was a significant risk factor in the non-infected group [odds ratio (OR) 3.025, 95% CI 1.171 - 7.818, p = 0.022] but not in the infected group (OR 0.889, 95% CI 0.261 - 3.024, p = 0.85).
The ratio of sIgE against a specific allergen (e.g. sIgE against B. tropicalis) to tIgE was smaller in children who were infected compared to non-infected children. This was true for all the allergens except for grass pollen for which infected children had a larger ratio (Fig. 1).
In this randomly selected population of schoolchildren in the Western Province of Sri Lanka, 15.5% were infected with one or more helminth species, while 33.7% evidence of allergic disease. In general, the study population had high tIgE levels and 80.3% showed evidence of allergic sensitization. A trend for protective role of helminth infection for the development of allergic disease was noted.
According to Sri Lankan national health statistics, hospital admissions due to respiratory ailments, especially asthma, has increased over the past decade [12], whereas the prevalence of helminth infections has fallen [13]. The province selected for this study is an area with increased urbanization and economical growth. A high prevalence of allergic diseases has been observed by previous workers, similar to that observed in some developed countries [14]. However, the tIgE levels in this study population were much higher than those observed in populations in developed countries [15-17] and similar to levels reported in populations in developing countries in tropics [18]. Furthermore, tIgE levels correlated better with helminth infections than with allergic disease. The only report to date on tIgE levels in Sri Lankans is a study performed over 20 years ago at the Children's Hospital, Colombo. The mean tIgE levels for asthmatics and non-asthmatics in that study were 4,531 kU/L and 2,500 kU/L respectively [19]. These levels are five-fold higher than the values observed among asthmatic children in our study. In the intervening period, the occurrence of helminth infections has declined greatly, following mass drug treatment programs across the country [13]. All these data points to the fact that in parallel to the declining prevalence of helminth infection, allergic diseases continue to increase in the selected area.
Evidence for a protective effect of helminth infection on allergic disease has been previously reported by several research groups [7-9]. We did not see a significant relationship between helminth infection and allergic disease but a trend toward a protective role of helminth infection on allergic disease could be observed. Given the fact that the area studied reported to have a dramatic fall in occurrence of helminth infections over the last decade, it can be speculated that a higher parasite burden may have the capacity to exert a greater protective role. This finding has major clinical implications since a continuous increase in childhood allergic diseases will impose a significant burden to the country's economy as well to the health care services. Nevertheless, it should be emphasized that it is not advisable to hold current practice aim to reduce the helminth infections in the community as chronic parasitic infections have many adverse health outcomes. The ultimate goal should be to discover the exact mechanism and molecules of the parasite that exert the immunomodulatory effect in the host and be used to avert or control the allergy epidemic while keeping the population free of parasite infections.
It is well established that atopy is a strong risk factor for developing allergic disease in people living in industrialized countries [20], whereas a consistent relationship has not been demonstrated in studies done in developing regions [21-23]. One drawback of this study is that, we could not perform skin prick test on these children as a measure of allergic sensitization but rather relied on serum sIgE levels. Nevertheless, our data showed a dual pattern of allergic sensitization: atopy confer a risk of allergic disease in only non-infected children which closely resembles the association observed in more "western" populations [20] but no such association was observed for infected children. This further strengthens our view, that the children included in our study represent a generation in transition toward a disease patterns observed in affluent populations. A high rate of allergic sensitization (as measured by serum sIgE) observed in our study could be due to the capacity of parasite to stimulate polyclonal synthesis of IgE (i.e. nonspecific production of IgE) [24] that accounts for the higher tIgE. In spite of high tIgE levels, infected children had lower sIgE for 4 out of 5 allergens tested. Graves et al. [25] and Marsh et al. [26] demonstrated that synthesis of specific and non-specific IgE is regulated separately, perhaps by two sets of genes. Helminth may modulate the immune response by enhancing one (non-specific IgE) while down regulating the other (sIgE), resulting in high tIgE with low sIgE. The importance of such a complex regulatory network in terms of helminth infection and atopy is still not well understood and needs further studies to elucidate this further.
Several other mechanisms have been proposed to explain the immune-modulatory effect of helminths, of which stimulation of a cytokine network within the host by the parasite has been widely studied [27]. Parasites are capable of inducing the synthesis of regulatory cytokines such as IL-10 and TGF-β which in-turn down regulate the host Th2-mediated allergic response. Of note, there could be multiple mechanisms by which helminths exert their effect on host's immune system and such effects may depend on a multitude of factors within the host as well as on the interaction between the host and the parasite.
Observation of a cohort of children living in a region in transition from high to low burden of helminth infections has provided an opportunity to investigate the role of helminth infection in modulating the immune response in human. A trend for a protective role of helminth infections on allergic disease as well as evidence of helminth infections interfering with IgE synthesis suggests that heavy infections with helminths might have the capacity to confer a protective effect on allergic diseases through modulation of IgE synthesis. A decline in such infections will have a significant impact on the trend of allergic diseases in developing countries in the tropics.
Figures and Tables
Fig. 1
Ratio of allergen-specific IgE (sIgE) to total IgE (tIgE) for different allergens in infected and uninfected children. Vertical bars represent the mean and 95% confidence interval.

Table 1
Association between helminth infection and allergic disease in the study population (n = 477)
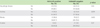
Table 2
Association between allergic disease and helminth infection. Multiple logistic regression was adjusted for sex and atopy (n = 477)
ACKNOWLEDGMENTS
The authors thank Kate Dunster and Aumann Heather of Immunology laboratory, Alfred Hospital, Melbourne, Australia for their support in laboratory work.
References
2. Shirakawa T, Enomoto T, Shimazu S, Hopkin JM. The inverse association between tuberculin responses and atopic disorder. Science. 1997. 275:77–79.

3. Shaheen SO, Aaby P, Hall AJ, Barker DJ, Heyes CB, Shiell AW, Goudiaby A. Measles and atopy in Guinea-Bissau. Lancet. 1996. 347:1792–1796.

4. Matricardi PM, Rosmini F, Riondino S, Fortini M, Ferrigno L, Rapicetta M, Bonini S. Exposure to foodborne and orofecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ. 2000. 320:412–417.

5. Leonardi-Bee J, Pritchard D, Britton J. Asthma and current intestinal parasite infection: systematic review and meta-analysis. Am J Respir Crit Care Med. 2006. 174:514–523.
7. Smits HH, Everts B, Hartgers FC, Yazdanbakhsh M. Chronic helminth infections protect against allergic diseases by active regulatory processes. Curr Allergy Asthma Rep. 2010. 10:3–12.

8. Calvert J, Burney P. Ascaris, atopy, and exercise-induced bronchoconstriction in rural and urban South African children. J Allergy Clin Immunol. 2010. 125:100–105.e1-e5.

9. Rodrigues LC, Newcombe PJ, Cunha SS, Alcantara-Neves NM, Genser B, Cruz AA, Simoes SM, Fiaccone R, Amorim L, Cooper PJ, Barreto ML. Early infection with Trichuris trichiura and allergen skin test reactivity in later childhood. Clin Exp Allergy. 2008. 38:1769–1777.

10. Amarasekera ND, Gunawardena NK, de Silva NR, Weerasinghe A. Prevalence of childhood atopic diseases in the Western Province of Sri Lanka. Ceylon Med J. 2010. 55:5–8.

11. WHO. Bench aids for the diagnosis of intestinal parasites. 1994. Geneva: World Health Organization.
12. Medical Statistics Unit, Ministry of Health Sri Lanka. Annual Health Bulletin of Sri Lanka. 2004. Colombo: Ministry of Health Sri Lanka.
13. Pathmeswaran A, Jayatissa R, Samarasinghe S, Fernando A, de Silva RP, Thattil RO, de Silva NR. Health status of primary schoolchildren in Sri Lanka. Ceylon Med J. 2005. 50:46–50.

14. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006. 368:733–743.

15. Sherrill DL, Stein R, Halonen M, Holberg CJ, Wright A, Martinez FD. Total serum IgE and its association with asthma symptoms and allergic sensitization among children. J Allergy Clin Immunol. 1999. 104:28–36.

16. Sunyer J, Antó JM, Castellsagué J, Soriano JB, Roca J. Total serum IgE is associated with asthma independently of specific IgE levels. The Spanish Group of the European Study of Asthma. Eur Respir J. 1996. 9:1880–1884.
17. Backer V, Ulrik CS, Wendelboe D, Bach-Mortensen N, Hansen KK, Laursen EM, Dirksen A. Distribution of serum IgE in children and adolescents aged 7 to 16 years in Copenhagen, in relation to factors of importance. Allergy. 1992. 47:484–489.

18. Levin ME, Le Souëf PN, Motala C. Total IgE in urban Black South African teenagers: the influence of atopy and helminth infection. Pediatr Allergy Immunol. 2008. 19:449–454.

19. Wilson PB, Fairfield JE, Beech N. Detection of IgG subclass-specific anti-IgE antibodies in normal and atopic individuals. Int Arch Allergy Appl Immunol. 1987. 84:198–204.

20. Wickman M, Ahlstedt S, Lilja G, van Hage Hamsten M. Quantification of IgE antibodies simplifies the classification of allergic diseases in 4-year-old children. A report from the prospective birth cohort study--BAMSE. Pediatr Allergy Immunol. 2003. 14:441–447.
21. Cooper PJ, Chico ME, Bland M, Griffin GE, Nutman TB. Allergic symptoms, atopy, and geohelminth infections in a rural area of Ecuador. Am J Respir Crit Care Med. 2003. 168:313–317.

22. Yemaneberhan H, Bekele Z, Venn A, Lewis S, Parry E, Britton J. Prevalence of wheeze and asthma and relation to atopy in urban and rural Ethiopia. Lancet. 1997. 350:85–90.

23. Nyan OA, Walraven GE, Banya WA, Milligan P, Van Der Sande M, Ceesay SM, Del Prete G, McAdam KP. Atopy, intestinal helminth infection and total serum IgE in rural and urban adult Gambian communities. Clin Exp Allergy. 2001. 31:1672–1678.

24. Cooper PJ, Alexander N, Moncayo AL, Benitez SM, Chico ME, Vaca MG, Griffin GE. Environmental determinants of total IgE among school children living in the rural Tropics: importance of geohelminth infections and effect of anthelmintic treatment. BMC Immunol. 2008. 9:33.

25. Graves PE, Kabesch M, Halonen M, Holberg CJ, Baldini M, Fritzsch C, Weiland SK, Erickson RP, von Mutius E, Martinez FD. A cluster of seven tightly linked polymorphisms in the IL-13 gene is associated with total serum IgE levels in three populations of white children. J Allergy Clin Immunol. 2000. 105:506–513.

26. Marsh DG, Neely JD, Breazeale DR, Ghosh B, Freidhoff LR, Ehrlich-Kautzky E, Schou C, Krishnaswamy G, Beaty TH. Linkage analysis of IL4 and other chromosome 5q31.1 markers and total serum immunoglobulin E concentrations. Science. 1994. 264:1152–1156.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download