Abstract
Background
Atopic dermatitis (AD) is a chronic inflammation of the skin that often appears in early childhood. The manifestation is related to the tendency towards T helper 2 cytokine immune responses (interleukin (IL)-4, IL-5). Genetic factors are suggested to play important roles in AD, and it can be transmitted to newborns, increasing their risk of developing allergies.
Objective
To determine the association between cord-blood cytokine levels (IL-5, interferon (IFN) γ), cord-blood total immunoglobulin E (IgE) level, perinatal environmental exposure, and the risks of allergy as well as the development of AD in the first 6 months of life.
Methods
A 6-month cohort study with a nested case-control within was conducted on newborns in Jakarta from December 2008 until May 2009. After the umbilical cord blood samples were taken and stored, subjects were followed up monthly until 6 months old. The occurrence of AD and lifestyle or environmental exposures were recorded. The allergic risk was determined using a modified pediatric allergy immunology work groups scoring system based on allergic history (allergic rhinitis, asthma, AD) in the family. The levels of IL-5 and IFN-γ were measured using ELISA and total IgE by CAP system FEIA. Multivariate analysis was used to evaluate risk factors.
Results
This study was conducted on 226 subjects. The incidence of AD was 16.4%; of those, 59% had low risk allergy, 38.5% moderate, and 2% high risk. AD mostly occurred at the age of 1 month (57%). Cord blood samples were examined in 37 subjects with AD and 51 without AD; of those, 25% showed high levels of total IgE (>1.2 IU/µL), and 51% showed normally-distributed high absorbance IL-5 values (≥0.0715, absolute value was undetected). The increased level of IL-5 was directly proportional to IgE. High absorbance IFN-γ values (≥0.0795, absolute value = 18.681 pg/µL) were observed in 52% of subjects.
Atopic dermatitis (AD) is a chronic inflammatory disease with peak onset in infancy. Recently, the incidence had been increasing rapidly. A study in Jakarta showed that among 635 allergic patients, 156 patients (24.6%) had AD skin symptoms (Munasir Z, Kurniati N, Akib A, Suyoko D, Siregar SP. Epidemiology asthma and allergy in Jakarta. 2006. unpublished data). A prospective study in England on children aged 0-42 months had shown that AD incidence was 21% at the age of 0-6 months, 11.2% at 7-18 months, and 3.8% at 19 to 30 months old. AD occurring in the early months of life can cause substantial pressure or burden on the family, affecting feeding and sleep patterns of infants and increasing medical expenses. Furthermore, AD can become a risk factor of allergen sensitization, asthma, allergic rhinitis, and hives in the future [1, 2].
Several studies have supported the existence of a critical period at an early age, including the perinatal period. Genetically, atopic infants have a higher risk of sensitization to food allergens. Interventions should be performed as early as possible in the perinatal period to obtain higher success rates. Important risk factors for atopy that can be controlled are formula feeding, introduction of hyperallergenic solid foods at an early age, exposure to environmental tobacco smoke, and lack of information about allergic disease [3].
Some studies showed that neonates with allergic risk factors have different cytokine profiles, in which peripheral blood mononuclear cells are stimulated by mitogens and allergens. All of these studies support the theory that the balance between cytokines suppressing allergic responses (T helper (Th) 1 response), such as interleukin (IL)-12 and interferon (IFN)-γ, and those contributing to allergies (IL-4, 5, 10, and 13) produced by Th2 cells is disrupted [4].
There are three interesting facts about the contribution of the fetal environment in the incidence of allergic disease. First, an elevated level of total immunoglobulin-E in umbilical cord blood is not a sensitive measurement in the incidence of allergic diseases later in life. Research has shown that fetus exposure to allergens in the womb is probably more significant in the incidence of allergic diseases. It was suggested that before birth, a fetus could form specific immunoglobulin E (IgE) induced by IL-4 [1, 3]. Second, the specific reactivity in neonates at birth against common allergens such as house dust mites, cow's milk, and eggs supports the concept of fetal exposure to the mother's food consumption and inhalant allergens, and it depends on the maturity of the immune system to respond against specific antigens [1, 3]. Third, the risk of allergic disease, especially in early infancy, is determined by both parents. If both have allergic diseases, the pregnancy period tends to be critical in determining the incidence of allergic diseases later in life. The risk of allergy in children born to allergic mothers was proven to be 4 times higher than those with an allergic father [1, 3].
The purpose of this study was to determine the association between cord-blood cytokine levels, cord-blood total IgE level, perinatal environmental exposure, and the risks of allergy, as well as the development of AD in the first 6 months of life.
This was a 6-month cohort study conducted between December 2008 to May 2009. Subjects were normal term newborns (delivered vaginally, birth weight >2,500 g) with high, moderate, or low allergic risks, who were recruited consecutively at the Neonatology Ward, Cipto Mangunkusumo Hospital, Harapan Kita Hospital, and Budi Kemuliaan Hospital Jakarta. The risk of allergy was obtained by the history of allergy (asthma, allergic rhinitis, and AD) in the family. Every positive answer was given a score of 2 if the allergy had been diagnosed by doctors and a score of 1 if it was only based on history taking. The total score showed the risk of allergy, and subjects were classified into three groups: high risk, moderate risk, and low risk [5-7].
The subjects were followed for 6 months to see the emergence of AD. The diagnosis was based on Hanifin Rajka criteria. Hyperallergenic food consumption during pregnancy (cow's milk, seafood, eggs, and nuts), breastfeeding, pets/domestic animals, carpets, and tobacco smoke exposure were noted. Exclusive breast feeding for the first 6 months (as recommended by Indonesian Ministry of Health) with the introduction of solid foods postponed to after the end of the sixth month was recommended. Umbilical cord blood examination for cytokine levels of IL-5, IFN-γ, and total IgE was done only in AD subjects and control subjects who didn't show AD manifestation in the first 6 months in the nested case control group. Total IgE examination was done by using CAP system specific IgE FEIA with kit Immulite 2000. IL-5 and IFN-γ levels were done by using quantikine immunoassay lot 268604 catalog no. D5000 kit (R&D systems, USA). The total sample population of this study was 269 subjects. This study was approved by the Ethical Commitee of Medical Faculty, University of Indonesia, Jakarta. The correlation between the dependent and independent variables was done by bivariate analysis followed by logistic multivariate analysis using SPSS 15.0 (SPSS, USA).
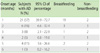
There were 269 subjects who fulfilled the eligibility criteria; of these, 226 could be followed up until 6 months after birth. Subjects' characteristics are shown on Table 1. Only a minority of children (2.2%) had a high risk of allergies.
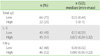
Table 2 shows 37 subjects with AD that occurred in their first 6 months of life; 91.9% had low to medium allergic risk. Most subjects had AD first appearing in the first month.
The bivariate correlation between some independent variables with incidence of AD is shown in Table 3. This study found that 98.2% of the subjects consumed hyperallergenic food (cow's milk, sea food, and nuts), whereas 1.8% of the subjects did not. Statistical tests showed no significant relationship (p = 0.372). From 33.2% of the subjects who were exclusively breastfed, 26.7% of the subjects suffered from AD. From non-exclusive breastfeeding subjects that consisted of 66.8% subjects, only 11.3% suffered from AD (p < 0.01; relative risk (RR) 2.369; 95% confidence interval (CI) 1.321-4.249).
In this study, 41.2% of the subjects that had a carpet in the house, and of these, 14% suffered from AD. Among the other 58.8% who had no carpet inside the house, 18% of the subjects suffered from AD. There was no significant difference found between groups (p = 0.461; RR 0.775; 95% CI 0.416-1.441).
From the total subjects who had pets/domestic animals (21.2%), 25% of the subjects suffered from AD; from 78.8% of the subjects who had no pets/domestic animals, 14% of the subjects suffered from AD. No significant differences were obtained (p = 0.069; RR 1.780; 95% CI 0.967-3.276).
In this study, 65.5% of the subjec ts were exposed to environmental tobacco smoke (ETS), and 34.5% of the subjects were not exposed. The result is not statistically significant (p = 0.931).
A multivariate test was performed including the factors that resulted in p < 0.25, that is, pets/domestic animals (p = 0.069; RR 1.780; 95% CI 0.967-3.276) and consumption of breast milk/non-breast milk (p < 0.01; RR 2.369; 95% CI 1.321-4.249). After the multivariate test, the pets/domestic animals factor combined with the risk of allergies and consumption of breast milk, are clinically the trigger factors with odd ratio (OR) 5.653 (Table 4) or RR 1.96 but statistically was not significant (Table 5).
From 88 examined blood samples (37 AD subjects and 51 control subjects in the nested case control group), 25% of the subjects showed high levels of total IgE (>1.2 IU/µL). From the AD subjects, 18.9% of the subjects showed high levels of IgE. No significant relationship was found statistically and clinically (p = 0.262; OR 1.786; 95% CI 0.644-4.950) (Table 6).
From this group, 51% of the subjects had a high level of IL-5 in umbilical cord blood. From the AD subjects, 49% of subjects showed high levels of IL-5. No significant correlation was found statistically and clinically (p = 0,344; OR 1.508; CI 0.643-3.536).
The increasing of IL-5 is inconsistent with increasing IgE. IL-5 distribution appeared to follow the pattern of IgE status, when it was compared with the IL-5 distribution for AD status (Figs. 1 and 2). However, there was no significant association.
Examination of this group showed that 52% of the subjects had a high level of IFN-γ. From the AD subjects, 59% of the subjects had a high level of IFN-γ. No significant correlation was found statistically and clinically (p = 0.473; OR 0.733; CI 0.313-1.716) (Table 7).
The occurrence of AD in this study is similar to the incidence of AD in other countries in the world (10-20%). According to the hygiene theory, the incidence of AD in Jakarta must be lower than incidence of AD in Western countries because the incidence and prevalence of infectious disease are still high. However, it has changed since infectious disease rates have decreased and pollution has increased in Jakarta. Of the subjects with AD, 91.9% had low to medium risk while 8.1% had a high risk. In most subjects, AD appeared in the first month, similar to the incidence of AD in a study performed in England [1]. The result of this study strongly supports the importance of early allergic detection as an early screening tool to enable early prevention of allergic disease. Although a bivariate test showed significant results, a multivariate test combined with pets/domestic animal and breastfeeding showed insignificant results. Ngamphaiboon et al. [8] reported a retrospective study in which 3,502 children were evaluated for atopic score. From their study, 35.2% developed allergy diseases (AD, asthma, and rhinitis) with the most manifestations appearing on average at 14.7 months (2 weeks to 5 years); the median was 9 months regardless of the atopic state in the family. Most of the allergy symptoms appeared in the first year of life (78.3%). Male children showed more atopic diseases than females (p < 0.001; OR 1.5; 95% CI 1.3-1.719). All the subjects with a score of 1 had a significant correlation with the manifestation of allergy disease with OR 2.64-3.22 with p < 0.01 and 95% CI. The score that could be used for screening of the high-risk infant was more than 2 with 68.8% sensitivity and 56% specificity. Eller et al. [9] found that early long-term sensitization worsens the prognosis, but 38% of all children have a debut later than 18 months of age. Boys had earlier onset of AD than girls. Our study showed no significant differences between males and females. This may be explaind by the fact that both boys and girls live in the same indoor environment in early life.
This study showed no significant correlation between hyperallergenic food consumption during pregnancy with the incidence of AD. The previous study showed that the fetus was able to respond against food and other allergens. Sometimes, food-specific IgE can be found [10], in addition to a T cell response against cow's milk protein, eggs, and aero allergens in the newborn baby [11]. Our study results support the American Academy of Pediatrics recommendations and European guidelines which do not recommend maternal avoidance of hyperallergenic foods during pregnancy. Meta analysis studies have shown that there was no benefit of maternal avoidance during pregnancy in preventing the occurrence of allergy in the fetus in later life [12].
The difference in AD incidence between exclusively and non-exclusively breastfed subjects is statistically significant (p ≤ 0.01; RR 2.369; 95% CI 1.321-4.249). These findings may give the impression that breast milk is a causative agent of AD. There are some possible explanations. First, most AD appeared in the first month of life (57%), in which infants were still exclusively breastfed. Since the important factor of AD pathogenesis is the skin's barrier defect, breastfeeding for a month is not enough to protect babies against allergic disease; however, breastfeeding may give protection in the gut barrier like in food allergy. Secondly, breastfeeding might be the cause of AD not because of the breast milk itself, but due to hyperallergenic food intake from the mother or the lack of anti-allergy components in breast milk which were not explored in this study. However, the multivariate test combined with allergy risk and pets/domestic animals showed insignificant result.
Out of the subjects who had pets/domestic animals (21.2%), 25% suffered from AD. Out of 78.8% subjects who had no pets/domestic animal, 14% suffered from AD. This difference statistically seems to be a causative factor regardless of other confounding factors. This is inconsistent with study results which showed that early and frequent exposure to pets/domestic animals may reduce sensitization resulting in allergy occurrence. After multivariate analysis, the presence of pets/domestic animals combined with the risk of allergies and consumption of breast milk were found to be clinical trigger factors of allergic disease but statistically were not significant.
The difference in AD incidence in subjects exposed and unexposed to ETS was not statistically significant. Mills et al. [13] reported their study on 150 AD patients showed that ETS was not linked to the risk of AD (p = 0.8; OR 1.1; 95% CI 0.65-1.86). However, the exposure to ETS during pregnancy increases the risk of AD in children. Therefore, ETS avoidance is very important during pregnancy for early allergy prevention [14].
The increasing IL-5 level is inconsistent with increasing IgE. IL-5 distribution appeared to follow the pattern of IgE status, when it was compared with the IL-5 distribution for AD status (Figs. 1 and 2). However, there was no significant association. The increasing IL-5 distribution in the group with high total IgE levels can be explained by the fact that the production of total IgE by B cells is influenced by the activity of Th2 (in this case IL-5). The question that might arise is whether the increase of IgE besides allergy-related factors could also be cause by helminthic or other parasitic infestations of the mother. Ustun et al. [15] reported increasing of IL-5 in helminthic and protozoal infestation while Malhotra et al. [16] showed that the fetus is able to produce the same cytokine as the mother's upon antigen stimulation. Such an infestation may be due to parasitic infestation in the subjects; however, this possibility was not explored in this study.
Cord blood examinations in subjects suffering from AD and control subjects that showed the mean level of IFN-γ was not significantly different between both groups. AD mostly appeared by 1 month of age, when the possibility of allergen sensitization was still low. This could occur due to staphylococcal colonization, which starts from birth. Further studies are needed to ascertain such an influence The OR for IFN-γ was 0.733, which indicates a protective effect, but the association was statistically not significant.
In conclusion, this study showed that the role of influence factors that have been observed with the occurence of AD in the first 6 months of age were not significant. It means that these factors were not important, but still other factors may have correlation with the occurence of AD in the first 6 months of age. As shown by Nagelkerke R = 0.116, it means that 88.4% of factors were not known in this study. The most important factor in AD is the skin barrier defect due to the fillagrin gene mutation. The genetic factor needs further study. The levels of IgE, IL-5 and IFN-γ of cord blood may not be sensitive predictive factors for AD, especially in developing countries where infection and parasitic infestation rates are still high.
Figures and Tables
Table 1
Subjects' characteristics and the occurrence of atopic dermatitis in the first 6 months of life (n = 226)

Table 3
The bivariate correlation between some independent variables with incidence of atopic dermatitis (AD) (n = 226)

Table 4
Multivariate correlation between allergy risk, pets/domestic animals, breastfeeding with the incidence of atopic dermatitis (n = 226)

Table 5
The relative risk (RR) calculation of multivariate correlation between allergy risk (AR), pets/domestic animals (P), breastfeeding (BF) with the incidence of atopic dematitis (n = 226)

ACKNOWLEDGEMENTS
We would like to thank Sopiyudin Dahlan M.D. for statistical advice, Professor Lee Be Wah from National University of Singapore, Mohamad Iqbal M.D., and Nikmah Salamia Idris M.D. for their comments during manuscript preparation. We also thank all the parents for their participation in this study.
References
1. Wadonda-Kabondo N, Sterne JA, Golding J, Kennedy CT, Archer CB, Dunnill MG. ALSPAC Study Team. A prospective study of the prevalence and incidence of atopic dermatitis in children aged 0-42 months. Br J Dermatol. 2003. 149:1023–1028.

2. Halken S, Høst A, Hansen LG, Østerballe O. Effect of an allergy prevention programme on incidence of atopic symptoms in infancy. A prospective study of 159 "high-risk" infants. Allergy. 1992. 47:545–553.
4. Prescott SL, Macaubas C, Holt BJ, Smallacombe TB, Loh R, Sly PD, Holt PG. Transplacental priming of the human immune system to environmental allergens: universal skewing of initial T cell responses toward the Th2 cytokine profile. J Immunol. 1998. 160:4730–4737.
5. Croner S. Prediction and detection of allergy development: influence of genetic and environmental factors. J Pediatr. 1992. 121:S58–S63.

6. Hansen LG, Halken S, Høst A, Møller K, Østerballe O. Prediction of allergy from family history and cord blood IgE levels. A follow-up at the age of 5 years. Cord blood IgE. IV. Pediatr Allergy Immunol. 1993. 4:34–40.
7. Bergmann RL, Edenharter G, Bergmann KE, Guggenmoos-Holzmann I, Forster J, Bauer CP, Wahn V, Zepp F, Wahn U. Predictability of early atopy by cord blood-IgE and parental history. Clin Exp Allergy. 1997. 27:752–760.

8. Ngamphaiboon J, Tansupapol C, Chatchatee P. Atopic risk score for allergy prevention. Asian Biomed. 2009. 3:121–126.
9. Eller E, Kjaer HF, Høst A, Andersen KE, Bindslev-Jensen C. Development of atopic dermatitis in the DARC birth cohort. Pediatr Allergy Immunol. 2010. 21:307–314.

10. Michel FB, Bousquet J, Greillier P, Robinet-Levy M, Coulomb Y. Comparison of cord blood immunoglobulin E concentrations and maternal allergy for the prediction of atopic diseases in infancy. J Allergy Clin Immunol. 1980. 65:422–430.

11. Warner JA, Miles EA, Jones AC, Quint DJ, Colwell BM, Warner JO. Is deficiency of interferon gamma production by allergen triggered cord blood cells a predictor of atopic eczema? Clin Exp Allergy. 1994. 24:423–430.

12. Fälth-Magnusson K, Kjellman NI. Development of atopic disease in babies whose mothers were receiving exclusion diet during pregnancy--a randomized study. J Allergy Clin Immunol. 1987. 80:868–875.
13. Mills CM, Srivastava ED, Harvey IM, Swift GL, Newcombe RG, Holt PJ, Rhodes J. Cigarette smoking is not a risk factor in atopic dermatitis. Int J Dermatol. 1994. 33:33–34.

14. Wang IJ, Hsieh WS, Wu KY, Guo YL, Hwang YH, Jee SH, Chen PC. Effect of gestational smoke exposure on atopic dermatitis in the offspring. Pediatr Allergy Immunol. 2008. 19:580–586.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download