Abstract
Background
Chronic idiopathic urticaria (CIU) has a significant impact on patients' quality of life.
Objective
The purpose of this study is to assess that impact and to compare differences by culture, gender, age or duration of treatment.
Methods
We used the modified chronic urticaria quality of life questionnaire, consisting of 15 questions. Over the course of 6 months, patients attending Immunology clinics at Campbelltown Hospital and private rooms in Australia and at the faculty of Medicine, University of Kelaniya in Sri Lanka were asked to fill out the questionnaires. We have obtained the data from 125 patients (43 Australian vs. 82 Sri Lankan). There were significantly more female patients (P < 0.01). The data was analysed using SAS.
Results
Overall, patients were affected mostly by itch and wheals and least affected by the side effects of treatments. Sri Lankan populations were more affected by wheals and by interference on activities, mood and food choices but were less affected by tiredness due to sleep disturbances (P < 0.01). Females were more affected by sleep disturbance (P < 0.05) while those older than 40 years of age were more impacted by tiredness and by the side effects from medications (P < 0.05), though the complaints themselves were mild. Those who suffered from CIU for more than 1 year were more affected by wheal, tiredness and irritability (P ≤ 0.05).
Chronic idiopathic urticaria (CIU) is a common condition, affecting 0.1% of the general population [1]. It is not life-threatening but several studies over the last decade have shown that it has a significant impact on quality of life (QoL) [2-4]. Its effect on QoL is comparable to that experienced by patients suffering from ischaemic heart disease with considerable loss of energy, sleep disturbance and emotional upset [2]. Compared to QoL in patients with respiratory allergy, CIU patients were more affected in physical functioning, pain perception and perceived health [3]. Compared to other dermatological conditions, the overall impact of CIU on QoL can be likened to acne and psoriasis [4]. More specifically, its physical discomfort and effect on daily living activities are similar to those suffering from atopic dermatitis and are more severe than psoriasis [5].
Despite these facts, there are only a few studies that have specifically looked at QoL in CIU. This is particularly relevant given the primary goal of CIU treatment is symptom control and improvement in QoL. As patient perception of disease and QoL can vary in different cultural contexts, understanding particular aspects of QoL specific to a given culture may bring into focus areas that need greater attention. However, there is no study to our knowledge that has compared QoL in CIU in different cultural contexts.
Most of the studies done so far have used different types of questionnaires with a varying degree of specific questions for CIU. Generic tools such as SF-36 (a health status questionnaire) and Nottingham Health Profile have the advantage of allowing comparison with different conditions but they have a potential to underestimate specific aspects of QoL that are particularly affected by CIU. Two other studies comparing QoL in CIU vs. other dermatological conditions have employed either the dermatology life quality index (DLQI) or VQ-Dermato [4, 5]. DLQI has been used extensively in assessment of dermatological conditions with good internal consistency and reliability. It has the advantage of being more relevant to dermatological conditions while allowing it to compare CIU with other dermatological diseases but again, it is not specifically developed for CIU. Recently a new tool, chronic urticaria quality of life questionnaire (CU-Q2oL), has been devised with a good level of validity, internal consistency and reliability [6]. It is able to evaluate the specific QoL issues related to CIU and at the same time, it is simple to administer, taking only a few minutes to complete.
The purpose of this study is to assess the impact of CIU on QoL and to compare the differences in different cultural contexts, in particular, in Australian and Sri Lankan populations. It also looks at whether gender, age or the duration of treatment have any impact on QoL. As this study is looking at the QoL in the same disease but in different subgroups, it was felt that administering CU-Q2oL was more appropriate for the reasons outline above.
In the first half of 2008, patients with the diagnosis of CIU attending either public or private Immunology/Allergy Clinics in Sydney, Australia and the clinic in the faculty of Medicine, University of Kelaniya in Sri Lanka were asked to fill out the questionnaire. Diagnosis of CIU was made based on history and examination by attending specialists.
We have used the CU-Q2oL published by Baiardini et al. [6] with modifications. (Fig. 1). A question on irritability was added as previous studies have indicated that CIU affects emotions and that this aspect needs to be explored further [2-5]. The questions on the use of cosmetics and limitations in choosing clothing materials were omitted as they were considered less relevant in our study populations. Indeed, in the original article by Baiardini et al. [6], these two questions ranked low in the overall impact. In addition, a question on nocturnal waking was also removed as there were already three questions pertaining to the effect of sleep disturbances. The questions on urticaria interfering with spare time and with social relationship were combined to form a question on recreational activities. The scales were increased from 0-3 to 0-6 as we felt that 0-3 scale would not capture varying degrees of discomfort experienced by patients. Score 0 was given when the patient was not affected and 6 was given when the patient was extremely affected.
Data was analysed using SAS version 9.1.3 (SAS Institute, USA). Non-parametric statistical methods were used as normality was not accepted within groups. Hence median rather than mean values were used to determine p-values although parametric tests returned similar p-values and reached the same conclusions anyway. A non-parametric alternative to a two sample t-test, Wilcoxon Mann-Whitney test, was used to ascertain significant differences. p-values ≤0.05 was considered statistically significant.
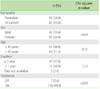
Demographics. Table 1 summarises the characteristics of the two study populations.
Questionnaire results. Overall, pruritus (median 5, mean 4.2) and wheals (median 5, mean 3.8) were the commonest complaints followed by CIU interfering with regular activities (median 4, mean 3.4), recreational activities (median 3, mean 3.1) and mood (median 3, mean 3.1). Patients were least affected by the side effects of treatments (median 0, mean 1.3) (Table 2, mean data not shown).
There were statistically significant differences noted between Australian and Sri Lankan patients in 5 out of 15 questions. The Sri Lankan population was more affected by wheals (median 5 vs. 4, P = 0.01) and by its interferences with regular activities (median 4 vs. 3, P < 0.01), mood (median 4 vs. 2, P < 0.01) and food choices (median 3 vs. 1, P < 0.01) but were less affected by tiredness due to sleep disturbances (median 1 vs. 3, P < 0.01) when compared to the Australian population (Table 2).
Females were more affected in sleep, especially with difficulty falling asleep (median 2 vs. 1, P < 0.05) but there were no differences in other parameters (Table 3). Those older than 40 years of age were more affected by tiredness due to poor sleep (median 2 vs. 1, P < 0.05) and by the side effects of medications (median 1 vs. 0, P < 0.05) though the complaints were mild. Patients who had CIU for longer than 1 year were more affected by itch (median 5 vs. 4, P = 0.01), tiredness due to poor sleep (median 2 vs. 1, P < 0.05) and irritability (4 vs. 2.5, P = 0.05).
Previous studies [2, 5] have indicated that CIU has a significant impact on QoL with notable effects on sleep, energy levels and mood so it is not surprising that the present study revealed similar results. The Australian patient population reported more sleep disturbance leading to daytime tiredness when compared to the Sri Lankan population but in both groups, those with longer duration of CIU reported more sleep disturbance, tiredness ands irritability.
Sri Lankan patients were more affected by wheals than their Australian counterparts. The reason for this is unclear and somewhat surprising as urticaria is usually less visible on darker skin. Cultural perception does not seem to play a major role in this as there was no significant difference in the level of embarrassment. Warmer climate in Sri Lanka may account for worsening wheals as urticaria is often exacerbated by heat. However, this alone does not provide an adequate explanation as other parameters such as itch were not increased. Alternatively, higher prevalence of helminth infections in Sri Lankan population with subsequent higher total IgE levels may play a role in worsening wheal formation. While there are reports of CIU associated with helminth infections, further studies will be required to clarify this issue [7, 8]. Sri Lankan patients were also more impacted by interference with regular activities and mood. The reasons for these are not apparent.
Sri Lankan populations were more inclined to limit food choices when compared to Australian patients. This may be due to a more prevalent assumption that CIU is due to food hypersensitivity in Sri Lanka. Alternatively, avoidance of certain common spicy foods in Sri Lanka that result in worsening symptoms by increasing body temperature may explain this phenomenon. While a number of significant differences in QoL parameters have been seen in this comparative study between two cultural groups, there are some potential confounders to be addressed. Firstly, there was no attempt to rank the severity of each patient's CIU. Thus it is possible that the Australian group had more severe CIU so reported more sleep disturbance. Also, while duration of treatment has been documented, we did not document the specific drugs used in individuals. If more sedating antihistamines were used by one group compared to the other, differences in tiredness may be due to this rather than the disease. However, patients in both groups ranked side effects from medication as being minimal so this is a less likely explanation.
The role of food intolerance in CIU is an area where there may be significant culturally driven differences in perception. For instance, there is a common belief, based on observation, that hot, spicy foods worsen urticaria so it is not surprising that we detected a difference between the two patient populations regarding limitations on food choices.
There were some gender-based and age-based differences noted in QoL. Overall, females from both populations had more difficulty with falling asleep. Previous studies have indicated that women have a higher prevalence of sleep disturbances compared to men and this may account for this finding [9]. Older patients were more affected by tiredness and by the side effects of medications. Both of these complaints are generally more prevalent in aging populations and this may account for the differences. Those patients affected by CIU for a longer duration were more affected by itch, tiredness due to poor sleep, and irritability. Perhaps this is a reflection of disease severity as itch can both interfere with the quality of sleep and mood. This also illustrates the fact that patients who have this condition for a long time do not necessarily 'get used to it' or become less affected by it.
In conclusion, there are significant differences noted in one third of the response to questionnaires between Australian and Sri Lankan patient populations with CIU. Some of the differences may be explained by differences in cultural perception and environmental factors, but variation in disease severity and differences in treatment regimens may also contribute in part and need further exploration.
Figures and Tables
Fig. 1
The self-administered questionnaire had four sections; personal details, practical problems, activities and mood. Respondents answered questions in the practical problems, activities and mood sections by selecting one of seven responses: not affected (score = 0), hardly affected at all (1), slightly affected (2), moderately affected (3), quite a bit affected (4), very affected (5) or extremely affected (6).

ACKNOWLEDGEMENTS
We gratefully acknowledge the help of Clive Gaskin, School of Medicine, University of Western Sydney, who performed statistical analysis.
References
2. O'Donnell BF, Lawlor F, Simpson J, Morgan M, Greaves MW. The impact of chronic urticaria on the quality of life. Br J Dermatol. 1997. 136:197–201.
3. Baiardini I, Giardini A, Pasquali M, Dignetti P, Guerra L, Specchia C, Braido F, Majani G, Canonica GW. Quality of life and patients' satisfaction in chronic urticaria and respiratory allergy. Allergy. 2003. 58:621–623.

4. Poon E, Seed PT, Greaves MW, Kobza-Black A. The extent and nature of disability in different urticarial conditions. Br J Dermatol. 1999. 140:667–671.

5. Grob JJ, Revuz J, Ortonne JP, Auquier P, Lorette G. Comparative study of the impact of chronic urticaria, psoriasis and atopic dermatitis on the quality of life. Br J Dermatol. 2005. 152:289–295.

6. Baiardini I, Pasquali M, Braido F, Fumagalli F, Guerra L, Compalati E, Braga M, Lombardi C, Fassio O, Canonica GW. A new tool to evaluate the impact of chronic urticaria on quality of life: chronic urticaria quality of life questionnaire (CU-Q2oL). Allergy. 2005. 60:1073–1078.

7. Wolfrom E, Chêne G, Boisseau H, Beylot C, Géniaux M, Taïeb A. Chronic urticaria and Toxocara canis. Lancet. 1995. 345:196.

8. Humbert P, Niezborala M, Salembier R, Aubin F, Piarroux R, Buchet S, Barale T. Skin manifestations associated with toxocariasis: a case-control study. Dermatology. 2000. 201:230–234.

9. Li RHY, Wing YK, Ho SC, Fong SYY. Gender differences in insomnia - a study in the Hong Kong Chinese population. J Psychosom Res. 2002. 53:601–609.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download