Abstract
This study evaluated the anti-Helicobacter and anti-inflammatory effects of Sohamhyungtang (SHHT). The minimum inhibitory concentration (MIC) of SHHT against Helicobacter pylori (H. pylori) was determined by the agar dilution method. Expression of the H. pylori cagA gene in the presence of SHHT was determined by quantitative real-time polymerase chain reaction (qRT-PCR). Inhibition of H. pylori urease by SHHT was determined by the phenol-hypochlorite assay. Antiadhesion activity of SHHT was measured by ureaphenol red reagent. Inhibition of nitric oxide (NO) production in AGS cells was measured with Griess reagent. Inducible nitric oxide synthase (iNOS) and IL-8 mRNA expression in AGS cells which were infected with H. pylori was determined by qRT-PCR. IL-8 level was measured by enzyme-linked immunosorbent assay (ELISA). The MIC of SHHT was 100 µg/mL and the expression of cagA gene was decreased about 25 folds in the presence of SHHT. H. pylori urease was inhibited 90% by SHHT. SHHT inhibited H. pylori adhesion on AGS cell in a concentration dependent manner. mRNA expression of iNOS and IL-8 and the production of NO and IL-8 were significantly decreased in the presence of SHHT. In conclusion, SHHT showed anti-Helicobacter activity and has potent anti-inflammatory effect on H. pylori-induced inflammation in human gastric epithelial AGS cells.
Helicobacter pylori (H. pylori) are a gram negative, microaerobic bacilli that infects more than half of the world's population.1 H. pylori infect more than 70% of Koreans aged over 40 years.1 H. pylori infection is closely related with upper gastrointestinal diseases, such as chronic gastritis, peptic ulcer disease, and gastric cancer.2 Major virulence factors of H. pylori are the cytotoxin-associated gene A (cagA), adhesion, and urease.3 The gene coding for cagA resides at the end of the cag pathogenicity island (cagPAI), which is a gene cluster of about 40 kb that also codes the type IV secretion system (T4SS), which injects the CagA protein into human gastric epithelial cells.4 CagA injected into the epithelial cells are activated by phosphorylation during intracellular signal transduction and induces morphological changes in epithelial cells.45 H. pylori are classified into cagA-positive and negative bacteria based on the genotype. CagA-positive bacteria increase the secretion of proinflammatory interleukin-8 (IL-8) from mucosal epithelial cells, and the inflammatory response induced by IL-8 damaged gastric epithelial cells, resulting in atrophic gastritis and gastric adenocarcinoma.67 Adhesion of H. pylori on gastric epithelial cell is a key step in the initiation of infection, which leads to the development of disease.4 Another virulence factor, urease, which is found in most strains of H. pylori, is well conserved genetically between strains. In particular, urease is a very important survival factor in the strongly acidic environment of the human gastric mucosa because it degrades urea to ammonia and CO2 and neutralizes the acidic environment. However, ammonia produced by urease also damages gastric epithelial cells and the mucosal membrane. As a result of generated ammonia and cagA described above, destruction and change of mucosal cells of the stomach is induced.8 Therefore, the inhibition of bacterial attachment to gastric epithelial cell, the inhibition of H. pylori urease activity and cagA expression could be a target of H. pylori treatment. H. pylori may induce inflammatory associated gene expression in gastric epithelial cells, including inducible nitric oxide synthase (iNOS) and resulted in excessive production of NO. However, excessive NO production during the inflammatory response leads to tissue damage, cytotoxicity and exacerbates inflammation by inducing the release of proinflammatory mediators IL-8.9 Therefore, these two factors are important mediators in gastric inflammation induced by H. pylori infection. Treatments for H. pylori infection have mainly depended on the use of antibiotics and proton pump inhibitors.101112 However, conventional antibiotic therapy has limitations to eradicate H. pylori because of the increasing failure rate caused by the development of resistant strains and the low compliance of patients.1314 Therefore, it is necessary to develop other eradication methods, and natural products and photodynamic therapy are alternative methods.151617
Sohamhyungtang (SHHT) is traditional medicine described in Sanghan theory, which is consisted of Coptidis Rhizoma, Pinelliae Tuber and Trichosanthis Semen.18 SHHT is used in oriental medicine to treat chest pain, and has been clinically used more recently for abdominal pain and respiratory tract diseases (pneumonia, pleurisy, and acute bronchitis).19 However, studies on how SHHT affects H. pylori are rare. In this study, we investigated anti-Helicobacter activity and the anti-inflammatory effects of SHHT on H. pylori.
Coptidis Rhizoma, Pinelliae Tuber and Trichosanthis Semen were purchased from World Herb Co. (Kyoungdong market, Seoul, Korea). Each plant was morphologically identified at the College of Pharmacy, Sahmyook University by professor Dongsool Yim. Coptidis Rhizoma, Pinelliae Tuber, and Trichosanthis Semen were mixed at a 1:5:4 ratios, and were extracted with ethanol for 4 h, and concentrated to yield dry residue (SHHT). From 60 g of Coptidis Rhizoma, Pinelliae Tuber, and Trichosanthis Semen (6 g: 30 g: 24 g), 5.9 g of dry residue was obtained (yield rate is 9.83%). Total alkaloid of rhizome of Coptidis Rhizoma was extracted with 3% HCl-acidic ethanol and concentrated to yield dry residue (CRTA). Berberine (BRBR) was purchased from Sigma-Aldrich (B3251, Sigma Co. St. Louis, MO, USA). The specimens of the plants were deposited at the College of Pharmacy at Sahmyook University, Seoul, Korea (SYUP-14-011, SYUP-14-012, SYUP-14-013).
Pre-coated silicagel 60 F254 thin layer chromatography (TLC) plates (Merck,Germany) were used for monitoring sample and spots were detected with UV light (254 and 365nm) and then sprayed with 10% sulfuric acid followed by heating to 100 ℃.20 TLC profile of SHHT, CRTA and BRB (B3251, Sigma Co. St. Louis, MO, USA) was shown in Fig. S1.
The standard strain of H. pylori 26695 (ATCC700392) and H. pylori ATCC 43504 (type strain for the minimum inhibitory concentration test) were purchased from the Korean Collection for Type Cultures (KCTC, Daejeon, Korea). H. pylori was cultured at 37℃ in a standard microaerobic (5% O2, 10% CO2, and 85% N2 gas) atmosphere on brain-heart infusion (BHI) (Difco, Detroit, MI, USA) with 7% laked horse blood (Oxoid, Cambridge, CB5 8BZ, UK), 0.4% isovitalex (BBL, Sparks, MD, USA), vancomycin (6 µg/mL), amphotericin B (8 µg/mL), and trimethoprim (5 µg/mL). In case of liquid culture, BHI media was prepared with horse serum (Sigma Co. St. Louis, MO, USA) instead of laked horse blood.
MICs of SHHT, CRTA and BRBR were determined according to the guidelines of Clinical & Laboratory Standard Institute (CLSI).21 Samples were two- fold diluted in BHI media and 5 × 105 CFU H. pylori 26695 were spotted onto these media. After 3 days of incubation, the lowest concentration that inhibited H. pylori growth was determined as the MIC. H. pylori ATCC43504 and amoxicillin were used for quality controls.
Inhibition of H. pylori urease activity was measured by the phenol-hypochlorite method described by Weatherburn with slight modifications.22 H. pylori 26695 was harvested from a BHI agar full plate and suspended in phosphate buffered saline (PBS). Cells were disrupted by 30 s bursts using a Sonifier (VCX130, SONIC, Watertown, CT, USA) at 30 W for a 50% cycle and were centrifuged at 10,000 rpm for 20 min at 4 ℃. The supernatant was used as enzyme solution, and protein concentration was determined by UV-spectrophotometry. A 10 µL (0.5mg/mL) of enzyme solution, 2 µL of sample (1~50 µg/mL of each sample) were incubated in a 96-well plate for 5 min at 37 ℃ and 5 µL urea buffer (0.5M urea in PBS) was added. The mixture was incubated for 10 min at 37 ℃ and 6 µL 0.1 N-H2SO4 was added to stop the reaction. A 50 µL phenol reagent [1% (v/v) phenol, 0.005% (w/v) sodium nitroprusside] and 50 µL alkali reagent [0.125M NaOH, 0.145 M Na2HPO412H2O, 1% (v/v) NaOCl] were added to the mixture followed by a 20 min incubation at 60 ℃. Absorbance was measured at 630 nm and 100 mM thiourea was used as the positive control. Percentage inhibition was calculated using the equation [1 − (ODtest/ODcontrol)] × 100.
The expression of cagA gene, a virulence factor of H. pylori was tested in the presence of SHHT, CRTA and BRBR. A total of 1 × 107 cell/mL of H. pylori 26695 were incubated with 20 µg/mL of SHHT, 10 µg/mL of CRTA and 2.5 µg/mL of BRBR for 8 h, and RNA was isolated using a Hybrid-R™ (GeneAll, Seoul, Korea) kit. The concentration of each sample was 1/5 of the MIC to avoid the growth inhibition of H. pylori itself. Total RNA (200 ng) was mixed with AccuPower CycleScript RT premix (dN12) (Bioneer, Daejeon, Korea), and cDNA was synthesized according to the manufacturer's manual. To amplify cagA and cysS mRNA, specific primers were synthesized by Genotech (Genotech, Daejeon, Korea), and the primer sequences are listed in Table 1. The quantitative real-time polymerase chain reaction (qRT-PCR) procedure for each gene was as follows: the reaction mixture was composed of 2 µL of cDNA template, 10 µL of Power SYBR Green PCR Master Mix (Life Technologies, Carlsbad, CA, USA), 5 pmole of each primer in a final volume of 20 µL. The Step-One Plus Real-Time PCR System (Life Technologies, Carlsbad, CA, USA) was used under the following reaction conditions: 95 ℃ for 10 min, 40 cycles of 95 ℃ for 15 s, and 60 ℃ for 60 s as thermal cycling stage. The program for analytical melting was 15 s at 95 ℃ and 60 s at 60 ℃ and an increase to 95 ℃ at a ramp rate of 0.3 ℃ per s. The cysS served as an internal control for the ddCt calculation. Each sample was tested in triplicate.
The human gastric epithelial AGS cell (KCLB #21739) was purchased from Korean Cell Line Bank (KCLB, School of Medicine, Seoul National University, Seoul, Korea). AGS cells were cultured in the modified RPMI1640 [10% heat inactivated fetal bovine serum (Sigma Co. St. Louis, MO, USA), 25 mM HEPES (Sigma Co. St. Louis, MO, USA), 1% penicillin-streptomycin (Sigma Co. St. Louis, MO, USA), L-glutamine (300 mg/L, Sigma Co. St. Louis, MO, USA), 25 mM NaHCO3 (Sigma Co. St. Louis, MO, USA)] at 37 ℃ in a standard cell culture atmosphere (5% CO2). In case of H. pylori infection, antibiotics free modified RPMI1640 was used.
The MTT [3-(4, 5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide] (Sigma Co. St. Louis, MO, USA) assay was performed to test cytotoxicity of SHHT, CRTA, and BRBR. A 1 ×106 AGS cells/well was inoculated into a 6-well plate and incubated with SHHT, CRTA, and BRBR for 24 h. The concentrations of SHHT were 60~100 µg/mL, those for CRTA were 10~50 µg/mL, and those for BRBR were 7~12.5 µg/mL. After the incubation, the supernatants were removed and 100 µL (5 mg/mL) of MTT reagent was added to each well and further incubated for 4 hr. After that, the supernatant was removed and 1 mL of dimethyl sulfoxide (DMSO, Sigma Co. St. Louis, MO, USA) were treated for 5 min, and absorbance was determined at 540 nm with ELISA reader (Synergy HT; Bio-TEK, Winooski, VT, USA). AGS cells that were not treated with sample were used as controls, and cell viability was compared with the control group. Each sample was tested in triplicate.
To test antiadhesion activity of SHHT, CRTA and BRBR, 1 × 106 AGS cells/well were inoculated into 96 well culture plate23. After 48 h incubation, the cells were washed three times with PBS. Nonspecific binding was blocked by 1 h of incubation at 37 ℃ with 0.5% BSA and then washed two times with PBS. After 30 min preincubation with SHHT (35, 70 µg/mL), CRTA (20, 10 µg/mL) and BRBR (10, 5 µg/mL), H. pylori was inoculated into AGS cells at a concentration of 1 × 108 cells/well and incubated for 3 h. After incubation, nonadherent bacteria were washed two times with PBS and 100 µL of urea phenol red solution (0.03% phenol red and 2% urea in PBS, pH 5.2) was added to each well. After 15 min incubation at 37 ℃, absorbance was measured at 560 nm with microplate reader. The percentage of attached H. pylori cells was calculated as follows: attached % = 100 − [(ODtest − ODnegative) / (ODpositive − ODnegative) × 100]. The negative control contained only AGS cells with no bacteria, and the positive control contained AGS cells and bacteria without sample. Each test was conducted in triplicate on different days.
Synthesis of NO was determined by an assay of culture supernatants for nitrite. Cells were treated with H. pylori 26695 with or without SHHT (35 and 70 µg/mL), CRTA (10 and 20 µg/mL), and BRBR (5 and 10 µg/mL) for 24 hr. A 100 µL of culture medium was mixed with the same volume of Griess Reagent (modified) and then incubated at room temperature for 10 min. Nitrite was measured by optical density (OD) at 540 nm using NaNO2 standard to generate a standard curve. Each sample was tested in triplicate.
AGS cells (1 × 106/well) were incubated for 24 hr and treated with 35 and 70 µg/mL of SHHT, 10 and 20 µg/mL of CRTA, and 5 and 10 µg/mL of BRBR. After 1 hr, H. pylori were infected in to each cell at a ratio of 1:300 (AGS: H. pylori). After 6 hr of incubation, AGS cells were homogenized with 1 mL of Trizol reagent, and total RNA were isolated with Hybrid-R™ (GeneAll, Seoul, Korea) kit. Total RNA (200 ng) was reverse transcribed to cDNA using the AccuPower CycleScript RT premix (dT20) (Bioneer, Daejeon, Korea) according to the manufacturer's manual. To amplify cDNA encoding iNOS, IL-8, and β-actin genes, specific primers synthesized by Genotech (Genotech, Daejeon, Korea) and sequences of PCR primers were listed in Table 1. The real-time PCR procedure for each gene was as follows: the reaction mixture was composed of 2 µL of cDNA template mixed with 10 µL of Power SYBR Green PCR Master Mix (Life Technologies, Carlsbad, CA, USA), 0.5 µL of each primer and in a final volume of 20 µL. The Step-One Plus Real-Time PCR System (Life Technologies, Carlsbad, CA, USA) was used with the following reaction conditions: 95 ℃ for 10 min, 40 cycles of 95 ℃ for 15 s, 60 ℃ for 60 s as thermal cycling stage. The program for analytical melting was 15 s at 95 ℃ and, 60 s at 60 ℃, and an increase to 95 ℃ at a ramp rate of 0.3 ℃ per s. β-actin was served as an internal control for the ddCt calculation. Each sample was tested in triplicate.
AGS cells (1 × 106/well) were seeded in a 24-well plate and incubated 24 hr. The cells were treated with SHHT (35 and 70 µg/mL), CRTA (10 and 20 µg/mL), and BRBR (5 and 10 µg/mL) and after 1 hr, H. pylori were infected at a ratio of 1:300 (AGS: H. pylori). After 24 hr incubation, the culture medium was collected for measuring IL-8 using human IL-8 ELISA kit (Thermo Scientific, Rockford, IL, USA) according to the manufacturer's manual. Each sample was tested in triplicate.
For each parameter of interest of the study, group variances were compared using Bartlett's test at the 0.05 significance level. When differences between group variances were not found to be significant, a parametric one-way analysis of variance (ANOVA) was performed. If significant differences among the means were indicated by the ANOVA (p ≤ 0.05), then Dunnett's test was used to perform the group mean comparisons between the control group and each treated group. All values are expressed as mean ± S.E. Statistical differences were evaluated using GraphPad PRISM ver. 5.0 software (GraphPad Software, La Jolla, CA, USA).
In the treatment of H. pylori infection, a major concern is the failure of primary treatment because of the development of resistant strains that make eradication difficult. The failure rate of treatment in Korea is approximately 20% because of bacterial resistance to antibiotics and the low compliance of patients.24 Accordingly, new bacterial eradication methods are needed as alternatives to antibiotic treatments in patients with strains of H. pylori resistant to primary antibiotic therapy. SHHT is a traditional medicine described in Sanghan theory,18 which is consisted of Coptidis Rhizoma, Pinelliae Tuber, and Trichosanthis Semen. According to previous studies, SHHT has antibacterial activity against methicillin-resistant Staphylococcus aureus and anti-inflammatory effect.2526 However, studies on how SHHT affects H. pylori are rare. This study was performed to investigate the effects of SHHT on the virulence factors of H. pylori and the anti-inflammatory effect against H. pylori-infected AGS cells. SHHT showed anti-Helicobacter activity. The MICs of SHHT, CRTA and BRBR were 100 µg/mL, 50 µg/mL and 12.5 µg/mL respectively (Table 2). According to the results of MTT assay, AGS cell viability was not affected at a concentration of 70 µg/mL of SHHT, 20 µg/mL of CRTA and 10 µg/mL of BRBR (Fig. 1). Acute toxicity to C57/BL6 mice did not appear until 2,000 mg/kg (data was not shown). Therefore, inhibition of SHHT, CRTA and BRBR on H. pylori induced mRNA and protein expression were not the results of its possible cytotoxic effect on H. pylori or AGS cells. As shown in Fig. 2, SHHT significantly inhibited urease activity of H. pylori. Compared with thiourea (100 mM), a representative urease inhibitor, SHHT, CRTA and BRBR inhibited 80~90% urease activity at a concentration of 10 and 50 µg/mL. Some studies have focused on urease inhibitors from natural product, such as biscoumarine.272829 Therefore, SHHT is also can be a candidate urease inhibitor for H. pylori infection. The antiadhesion activity was measured by urea-phenol red method. The antiadhesion activities of SHHT, CRTA and BRBR were observed in a concentration dependent manner. At a concentration of 70 and 35 µg/mL of SHHT, only 4.44% and 14.22% of adherent H. pylori cells were observed as compared with positive control (Fig. 3). The adhesion of H. pylori to epithelial cells is an important step for the growth and colonization of H. pylori and disease formation by H. pylori.30 The cagA protein is transported to the host cell via T4SS after H. pylori adheres to epithelial cell.4 Therefore, the antiadhesion activity of SHHT may relieve the inflammation and decrease the risk of gastric disorders.
To investigate the effects of SHHT, CRTA, and BRBR on the gene expression of cagA, which is a representative H. pylori virulence factor, qRT-PCR was performed. One-fifth of the MICs of SHHT (20 µg/mL), CRTA (10 µg/mL), and BRBR (2.5 µg/mL) were used to avoid growth inhibition of H. pylori by each sample. As shown in Table 3, cgaA gene expression was decreased significantly in the presence of SHHT (relative quantification [RQ] 1 vs. 0.039), CRTA (RQ 1 vs. 0.049), and BRBR (RQ 1 vs. 0.029). CagA injected into gastric epithelial cells is activated by phosphorylation during intracellular signal transduction and induces morphological changes in epithelial cells.45 CagA also increases the secretion of proinflammatory interleukin IL-8 from mucosal epithelial cells, and inflammatory response induced by IL-8 damage gastric epithelial cells and resulting in atrophic gastritis and gastric adenocarcinoma.67 Therefore, inhibiting cagA gene expression by SHHT, CRTA and BRBR may help regulation of inflammatory and immune processes in response to H. pylori. SHHT have been used as anti-inflammatory agents for a number of years. However, the anti-inflammatory effect against H. pylori has not been reported. Therefore, we investigated the effects of SHHT on the pro-inflammatory mediators (iNOS and IL-8). As we described above, cagA expression was significantly decreased in the presence of SHHT and therefore IL-8 was the target cytokine determined in this study. As shown Fig. 4, H. pylori increased NO production in AGS cells. And pretreatment of SHHT, CRTA, and BRBR in AGS cells significantly decreased NO production from 32.4% to 43.2% compared with control group. After 6 h co-culture with H. pylori, iNOS and IL-8 gene expression were increased significantly in AGS cells. However, treatment of SHHT, CRTA and BRBR inhibited H. pylori-induced iNOS and IL-8 gene expression in a concentration dependent manner (Table 4). In case of iNOS mRNA expression, the RQ of AGS was 1, that of AGS + H. pylori was 2.23, and that of SHHT (70 µg/mL) was 0.43. In case of IL-8 mRNA expression, RQ of AGS was 1, that of AGS + H. pylori was 85.03, and that of SHHT (70 µg/mL) was 25.63. H. pylori significantly increased IL-8 levels in AGS cells (1,400 pg). However, IL-8 level was significantly decreased in the presence of 70 µg/mL SHHT (1,036 pg, 27.36%), 20 µg/mL CRTA (1,013 pg, 52.7%), and 10 µg/mL BRBR (1108 pg, 42.0%) compared with those of control group (Fig. 5). According to the results, treatment of SHHT significantly reduced NO production in H. pylori-infected AGS cells. iNOS and IL-8 mRNA expression were also significantly reduced in the presence of SHHT and IL-8 production was also significantly reduced. Early reports clearly related IL-8 induction in gastric cells to a functional cagA. In our experiment, cagA gene expression in H. pylori was markedly reduced by SHHT (Table 3) and IL-8 production in AGS cells was also reduced (Fig. 5). These results suggest that reduced cagA expression in H. pylori by SHHT might result in reduced production of IL-8 in H. pylori-infected AGS cells. IL-8 secreted by gastric epithelial cells is an important mediator of neutrophil migration to the infection site and then getting serious inflammation in H. pylori infected gastric epithelial cells.3132 According to our results, SHHT and berberine from Coptidis Rhizoma effectively reduced IL-8 mRNA expression and IL-8 production in H. pylori infected AGS cells. These results indicate that SHHT may play an important role in gastric mucosa infected by H. pylori and could be a candidate anti-Helicobacter agent. In this study, we focused on the SHHT and one of its component, Coptidis Rhizoma and berberine, however according to our results, other components of SHHT might have urease inhibitory activity, inhibition of NO production and IL-8 production. Therefore, it is necessary to study other components of SHHT (Pinelliae Tuber and Trichosanthis Semen) and to study in vivo test in the future.
Figures and Tables
 | Fig. 1AGS cell viability test in the presence of various concentrations of SHHT (60~100 µg/mL), CRTA (10~50 µg/mL), and BRBR (7~12.5 µg/mL) for 24 hr. Changes in survival rate are presented as percentages of the control. Values are expressed as the mean ± SE of triplicate tests. *p < 0.05, **: p < 0.01, ***: p < 0.001. vs. control by ANOVA and Dunnett's multiple comparison test. Control: AGS cells, SHHT: AGS cells + Sohamhyungtang, CRTA: AGS cells + total alkaloid of rhizome of Coptidis Rhizoma, BRBR: AGS cells + Berberine. |
 | Fig. 2Inhibition of H. pylori urease in the presence of SHHT, CRTA, and BRBR. Changes in inhibition are presented as percentages of the control (100mM thiourea). Values are expressed as the mean ± SE of triplicate test. SHHT: Sohamhyungtang, CRTA: Total alkaloid of rhizome of Coptidis Rhizoma, BRBR: Berberine. |
 | Fig. 3Antiadhesion of SHHT, CRTA and BRBR against H. pylori to AGS human gastric cells. Antiadhesive activity was determined by urea phenol red method. The positive control means without samples and used to establish 100% attachment. The results are the mean ± SE for three independent experiments. *p < 0.05, **: p < 0.01, ***: p < 0.001. vs. control by ANOVA and Dunnett's multiple comparison test. |
 | Fig. 4Effects of SHHT, CRTA, and BRBR on H. pylori 26695-induced NO production in AGS cells. Changes in NO production are presented as percentages of control. Values are expressed as the mean ± S. E in triplicate tests. **: p < 0.01, ***: p < 0.001. vs. control by ANOVA and Dunnett's multiple comparison test. None: AGS cells, Control: AGS cells + H. pylori, SHHT: AGS cells + H. pylori + Sohamhyungtang, CRTA: AGS cells + H. pylori + Total alkaloid of rhizome of Coptidis Rhizoma, BRBR: AGS cells + H. pylori + Berberine. The effects of SHHT, CRTA, and BRBR itself on the AGS cells, they showed no difference compared with AGS cells (data was not shown). |
 | Fig. 5Effects of SHHT, CRTA, and BRBR on H. pylori 26695-induced IL-8 production in AGS cells. Changes in IL-8 production are presented as percentages of the control. Values are expressed as the mean ± S. E. in triplicate tests. **: p < 0.01, ***: p < 0.001 vs. control by ANOVA and Dunnett's multiple comparison test. Non: AGS cells, Control: AGS cells + H. pylori,SHHT: AGS cells + H. pylori + Sohamhyungtang, CRTA: AGS cells + H. pylori + Total alkaloid of rhizome of Coptidis Rhizoma, BRBR: AGS cells + H. pylori + Berberine. The effects of SHHT, CRTA and BRBR itself on the AGS cells, they showed no difference compared with AGS cells (data was not shown). |
Table 1
Primer sequences for qRT-PCR analysis

Table 2
MICs of SHHT, CRTA and BRBR against H. pylori 26695
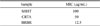
| Sample | MIC (µg/mL) |
|---|---|
| SHHT | 100 |
| CRTA | 50 |
| BRBR | 12.5 |
Table 3
Comparison of relative cagA expression in the presence of the SHHT, CRTA and BRBR

Table 4
Comparison of relative iNOS and IL-8 mRNA expression in H. pylori infected AGS cells in the presence of the SHHT, CRTA and BRBR

References
1. Kim JH, Kim HY, Kim NY, Kim SW, Kim JG, Kim JJ, Seo JK, Sim JG, Roe IH, Ahn H, Yoon BC, Lee SW, Lee YC, Chung IS, Jung HY, Hong WS, Choi KW. Korean J Med. 2000; 59:388–397.
2. Peek RM Jr, Blaser MJ. Nat Rev Cancer. 2002; 2:28–37.
3. Grahma DY, Yamaoka Y. Heliocbacter. 2000; 5:S3–S9.
4. Odenbreit S, Püls J, Sedlmaier B, Gerland E, Fischer W, Haas R. Science. 2000; 287:1497–1500.
5. Tegtmeyer N, Wessler S, Backert S. FEBS J. 2011; 278:1190–1202.
6. Blaser MJ, Perez-Perez GI, Kleanthous H, Cover TL, Peek RM, Chyou PH, Stemmermann GN, Nomura A. Cancer Res. 1995; 55:2111–2115.
7. Crabtree JE, Wyatt JI, Trejdosiewicz LK, Peichl P, Nichols PH, Ramsay N, Primrose JN, Lindley IJ. J Clin Pathol. 1994; 47:61–66.
8. Marshall BJ, Barrett LJ, Prakash C, McCallum RW, Guerrant RL. Gastroenterology. 1990; 99:697–702.
9. Lee YC. Korean J Gastroenterol. 2005; 46:159–165.
10. Bell GD, Bate CM, Axon AT, Tildesley G, Kerr GD, Green JR, Emmas CE, Taylor MD. Aliment Pharmacol Ther. 1995; 9:513–520.
11. Misiewicz JJ, Harris AW, Bardhan KD, Levi S, O'Morain C, Cooper BT, Kerr GD, Dixon MF, Langworthy H, Piper D. Gut. 1997; 41:735–739.
12. Spinzi GC, Boni F, Bortoli A, Colombo E, Ballardini G, Venturelli R, Minoli G. Aliment Pharmacol Ther. 2000; 14:325–330.
13. Egan BJ, Marzio L, O'Connor H, O'Morain C. Helicobacter. 2008; 13:35–40.
14. Romano M, Iovene MR, Russo MI, Rocco A, Salerno R, Cozzolino D, Pilloni AP, Tufano MA, Vaira D, Nardone G. J Clin Pathol. 2008; 61:1112–1115.
15. Brown JC, Huang G, Haley-Zitlin V, Jiang X. Appl Environ Microbiol. 2009; 75:848–852.
16. Cha WS, Kim JH, Lee KH, Kwon HJ, Yoon SJ, Choi UK, Cho YJ. J Korean Soc Food Sci Nutr. 2006; 35:315–320.
17. Choi SS, Lee HK, Chae HS. J Photochem Photobiol B. 2010; 101:206–209.
18. Hong YH, Peacher WG. SHANG HAN LUN: The great classic of Chinese medicine. California: Oriental healing arts institute;1981. p22.
19. Kook YB. Bangjekak. Seoul: Younglimsa;1999. p. 535–536.
20. Xie PS. Characteristic chemical fingerprints of traditional Chinese medicine. Beijing: People's Publishing House;2005. p. 314–322.
21. Clinical and Laboratory Standards Institute (CLSI). Document M100-S19. Performance standards for antimicrobial susceptibility testing: 19th Informational Supplement. Pennsylvania: CLSI;2009.
22. Weatherburn MW. Anal Chem. 1967; 39:971–974.
23. Lee JH, Shim JS, Chung MS, Lim ST, Kim KH. Phytother Res. 2009; 23:460–466.
24. Choi YS, Cheon JH, Lee JY, Kim SG, Kim JS, Kim N, Lee DH, Kim JM, Jung HC, Song IS. Korean J Gastroenterol. 2006; 48:156–161.
25. Kim JE, Yun HJ, Choi DY, Park SD. Kor J Ori Med Physiol Pathol. 2010; 24:61–66.
26. Yum DY, Baek DG, Song YS. Kor J Ori Med Physiol Pathol. 2012; 26:886–893.
27. Bae EA, Han MJ, Kim DH, Kim NJ. Biol Pharm Bull. 1998; 21:990–992.
28. Khan KM, Iqbal S, Lodhi MA, Maharvi GM, Ullah Z, Choudhary MI, Rahman AU, Perveen S. Bioorg Med Chem. 2004; 12:1963–1968.
29. Lodhi MA, Shams S, Choudhary MI, Lodhi A, UI-Haq Z, Jalil S, Nawaz SA, Khan KM, Iqbal S, Rahman AU. Biomed Res Int. 2014; 2014:935039.
30. Guruge JL, Falk PG, Lorenz RG, Dans M, Wirth HP, Blasér MJ, Berg DE, Gordon JI. Proc Natl Acad Sci U S A. 1998; 95:3925–3930.
31. Harris PR, Mobley HL, Perez-Perez GI, Blaser MJ, Smith PD. Gastroenterology. 1996; 111:419–425.
32. Huang J, O'Toole PW, Doig P, Trust TJ. Infect Immun. 1995; 63:1732–1738.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download