Introduction
Allergic responses have two phases: an early phase mediated by mast cells and a late phase mediated by T cells.12 Mast cells are important effecter cells in allergic reactions as well as in allergy processes due to their ability to secrete numerous mediators including cytokines, enzymes, and biogenic amines.34 Activated mast cells release pro-inflammatory cytokines, such as interleukin (IL)-6 and IL-8, and inflammatory mediators including histamine.567 The importance of mast cell in immunomodulation has been discussed in recent reviews and reports.8910
Signal transducers and activators of transcription (STATs) were identified as a unique family of DNA-binding proteins.11 STAT proteins have been shown to play an important role in cytokine signaling pathways.12 Activated STAT3 has been reported to up-regulate the expression of one of the most important mediators of inflammation.13 STAT3 also induces the expression of genes relevant to tissue injury and inflammation, referred to as acute phase response genes.1114
Sinensetin is, one of methoxyflavones found commonly in Citrus species, known to be involved in various pharmacological activities including anti-angiogenesis, anti-diabetic and anti-inflammatory activities. Recent studies have reported that sinensetin inhibits not only NF-κB p65 translocation by regulating the protein level of IκBα but also inflammatory gene expression and STAT1 activation.1516 However, its anti-allergic effects on interleukin 6 via STAT3 in human mast cell - 1 (HMC-1) remain unknown.
In the present study, sinensetin was evaluated for its inhibitory effect on the IL-6 production, and phosphorylation of STAT3 in PMA plus A23187-induced HMC-1 along with IL-4, 5, and 8 mRNA expressions.
Experimental
Cell culture
A human mast cell line, HMC-1, was obtained from the Korea Research Institute of Bioscience and Biotechnology (South Korea) and grown in IMDM Medium containing 10% fetal bovine serum and 100 U/ml penicillin/streptomycin sulfate. Cells were incubated in a humidied 5% CO2 atmosphere at 37 ℃.
Drugs and chemicals
IMDM, penicillin, and streptomycin were purchased from Hyclone (Logan, UT, USA). Bovine serum albumin, phorbol 12-myr-istate 13-acetate (PMA) and A23187 were purchased from Sigma (St. Louis, MO, USA). Anti-mouse IL-6 antibody and biotinylated anti-mouse IL-6 antibody were purchased from BD Biosciences (BD Pharmingen, San Diego, CA). p-STAT3, STAT3, p-NF-κB(p65), NF-κB(p65) antibodies were purchased from Cell Signaling Technology, Inc. (Danvers, MA). Sinensetin (ASB-00019265-010) was purchased from ChromaDex Inc. (Irvine, CA, USA).
Determination of interleukin-6 levels
Cells were seeded at 1 × 106/ml per well in 24 well tissue culture plates and pretreated with the indicated concentration of sinensetin for 30 min before stimulation. After 24 h, the supernatant was decanted into a new micro centrifuge tube, and the amount of IL-6 was determined using the ELISA kit according to the procedure described by the manufacturer (BD Bioscience, USA). All subsequent steps took place at room temperature, and all standards and samples were assayed in duplicate.
Western blot analysis
Protein expression was assessed by Western blot analysis according to the standard procedure. Briey, HMC-1 was cultured in 60 mm culture dishes (2 × 106/ml) and then pretreated with various concentrations of sinensetin (0.8, 4, 20 µM). After 30 min of pretreatment, PMA plus A23187 was added to the culture medium, and the cells were then incubated at 37 ℃ for 20 min. Following incubation, the cells were washed twice in ice cold PBS (pH 7.4). Immunoreactivity was then detected using enhanced chemiluminescence (ECL: Amersham, Milan).
RNA Extraction and reverse transcription-polymerase chain reaction (RT-PCR)
Total cellular RNA was isolated using an easy-BLUETM RNA extraction kit according to the manufacturer's instructions. PCR was then performed using a reaction mixture comprised of 50 mM KCl, 10 mM Tris-HCl (pH 8.3), 1.5 mM MgCl2, 0.2 mM dNTPs, 2.5 units of Taq DNA polymerase, and 0.1 µM each of primers specific for IL-6, IL-4, IL-5, IL-8 and GAPDH. Amplification conditions were as follows: denaturation at 94 ℃ for 3 min for the first cycle and for 45 s starting from the second cycle, annealing of IL-6 at 55 ℃ for 30 s, for 25 cycles and annealing of IL-4,5,8 at 55 ℃ for 30 s, for 30 cycles. Final extension was performed at 72 ℃ for 7 min. PCR products were then electrophoresed on a 1.5% agarose gel and stained with ethidium bromide. Primers used were 5′–AAAGAGGCA CTGGCAGAAAA–3′ (sense) and 5′–AAAGCTGCGCA GAATGAGAT–3′ (antisense) for IL-6, 5′–ACTGCTTCC CCCTCTGTTCT–3′ (sense) and 5′–CTCTGGTTGGCTT CCTTCAC–3′ (antisense) for IL-4, 5′–GAGACCTTGG CACTGCTTTC–3′ (sense) and 5′–ATCTTTGGCTGCA ACAAACC–3′ (antisense) for IL-5, 5′–AGGGTTGCCA GATGCAATAC–3′ (sense) and 5′–GTGGATCCTGGCT AGCAGAC–3′ (antisense) for IL-8, 5′–GTCAGTGGTG GACCTGACCT–3′ (sense) and 5′–AGGGGAGATTCA GTGTGGTG–3′ (antisense) for GAPDH.
Result and Discussion
The cell viability test with sinensetin in the human mast cell (HMC-1) revealed no toxicity up to 20 µM (data not shown). Activated mast cells release a broad spectrum of mediators including cytokines such as IL-4, IL-5, IL-6, and IL-8.10 Interleukin-6 (IL-6) is known as a pro-inammatory cytokine.17 The preliminary results of sinensetin showed that exhibited anti-inflammatory activity using IL-6 expression. Culture supernatants were assayed for IL-6 levels using the ELISA method. In stimulated mast cells, the level of IL-6 was elevated, and treatment of sinensetin lowered the elevated IL-6 levels in a dose-dependent manner (Fig. 1.A). The effect of sinensetin on IL-6 mRNA expression induced by PMA plus A23187 was examined using RT-PCR. As shown in Fig. 1.B., treatment of PMA plus A23187 increased the mRNA expression of IL-6, whereas sinensetin suppressed this increase (Fig. 1.B).
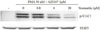
The importance of the STAT pathway in the survival proliferation and acute phase reaction is well reported elsewhere.1819 STAT3 is activated by phosphorylation at Tyr705, which induces nuclear translocation, and DNA binding.20 Activated STAT3 not only plays important roles in the regulation of inflammation gene expression but can also be further activated by cytokine binding to receptors.21 Regulators of the IL-6/STAT pathway, such as suppressors of cytokine and protein inhibitors of activated STAT proteins, function to modulate the immune response and maintain homeostasis.22 The effect of sinensetin on STAT3 phosphorylation induced by PMA plus A23187 was examined using Western blotting analysis. As shown in Fig. 2., when treated with sinensetin, STAT3 phosphorylation was suppressed in a dose dependent manner, implying that STAT3 may be involved in lowering IL-6 expression.23 It was examined that effect of sinensetin on the stimulated phosphorylation of STAT3 in HMC-1 using western blot analysis. As shown in Fig. 2., when treated with sinensetin, STAT3 phosphorylation was suppressed in a dose dependent manner. The amount of non-phosphorylated STAT3 was unaffected by either PMA plus A23187 or sinensetin treatment.
The roles of nuclear factor-kappa B (NF-κB) and signal transducers and activators of transcription 3 (STAT3) in pathogenesis of inflammation have been extensively investigated.24 NF-κB plays an important pathophysiological role in the regulation of cell survival and expression of pro-inammatory mediators, including IL-6.25 The protein levels of p65, the major component of NF-κB, in nuclear extracts were investigated by Western blotting analysis. In addition, we measured cytoplasmic levels of IκBα in order to determine whether blockade of translocation of p65 by sinensetin is related to IκBα degradation. It was found that sinensetin inhibits IκBα degradation and p65 translocation (Fig. 3), leading to suppression of NF-κB activation. NF-κB (p65) is the major component of NF-κB activated by PMA plus A23187 in mast cell, we investigated the protein levels of p65 in nuclear extracts by Western blot analysis. HMC-1 was incubated with PMA plus A23187 in the presence or absence of sinensetin for 20 min. The PMA plus A23187-induced nuclear translocation of p65 was inhibited by sinensetin in a dose-dependent manner (Fig. 3). Since nuclear translocation is preceded by IκBα degradation, we measured cytoplasmic levels of IκBα by Western blot analysis to determine whether the inhibition of p65 by sinensetin is related to IκBα degradation.
Furthermore, IL-4, and 5 have been associated with causing several allergic diseases including allergic rhinitis and asthma. IL-8 can be secreted by any cells with toll-like receptors that are involved in the innate immune response. Since sinensetin inhibited the allergic-related cytokine, we investigated the effect of sinensetin on stimulated IL-4, 5, 8 expressions by RT-PCR. In stimulated cells, IL-4, 5, and 8 mRNA expression was increased, while pretreatment of sinensetin decreased mRNA levels in a dose-dependent manner (Fig. 4).
From these observations, STAT3 and NF-κB seemed to be involved in the production of IL-4, IL-5, IL-6 and IL-8 in PMA plus A23187 stimulated mast cell.26 Previous study, sinensetin show anti-inflammatory activity by regulating the protein level of IκBα.16 In this study, sinensetin is thought to induce its anti-allergic activity by inhibiting the release or expression of IL-4, 5, 6, and 8 via suppressing STAT3 and NF-κB activation stimulated by PMA plus A23187 in human mast cells.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download