INDICATIONS FOR TREATMENT OF PATIENTS WITH SPECIAL NEEDS UNDER GENERAL ANESTHESIA
Limited literature exists regarding the indications for treatment of patients with special needs under general anesthesia. Dougherty [
3] attempted to review the literature in this area almost a decade ago and encountered a marked lack of relevant studies. Nonetheless, several similar reviews have identified that the primary indication for general anesthesia is lack of patient cooperation due to anxiety, intellectual disability, or some other impairment [
236].
These indications are largely supported by other studies in patients receiving dental treatment under general anesthesia—both in patients with special needs and in the general population. For example, a review by Nunn et al. [
7] examined the files of patients treated under general anesthesia at the Dental Hospital of the University of Newcastle upon Tyne in the United Kingdom. They found that 30.2% of the adult and pediatric patients had an intellectual impairment. Other commonly cited reasons were the presence of multiple handicaps (24.0%), or dental phobia (21.4%). Similarly, a review of the Dental Program for Persons with Disabilities at Mount Sinai Hospital in Toronto, Canada, found concordant results [
8]. Patients treated under general anesthesia were more likely to live in group institutions than at home with their family. Furthermore, such patients were more likely to have intellectual disabilities, autism, behavioral problems, scoliosis, and seizure disorders. Patients with a limited history of dental procedures (i.e. those who had only undergone examinations and preventive treatment in the dental clinic) were also more likely to be treated under general anesthesia, as were those taking seizure-related and psychotropic medications [
8].
Specifically, behavior has been identified as a significant indicator across many studies, not purely those carried out in special needs populations. A review conducted by the Helsinki Public Dental Service in Finland found that the main reasons for treatment under general anesthesia were extreme non-cooperation (65%), dental phobia (37%), and an urgent need for treatment (26%) [
9]. Many studies have confirmed these findings [
10111213].
Still further considerations have been cited as influencing the decision to treat patients under sedation or anesthesia, including the overall health of the patient, the preferences of the patient, carers, or family, the indicated procedures, and operator or facility-related factors [
71214]. Issues of cost may also be relevant in certain settings [
12]. However, few studies in intellectually disabled patients have considered how complaints or concerns of family and carers may affect the assessment of these patients.
As many patients with special needs present resistance to conventional dental examination, Hennequin et al. [
13] examined whether assessments involving carers could be used to accurately evaluate the dental treatment needs of these patients. In that study, carers who were familiar with the patients were questioned about their causes for concern, asked to estimate the degree of pain or discomfort they felt the patient was likely to be suffering, and asked to estimate the number of oral sites where they felt treatment was needed. Common concerns that prompted carers to seek treatment included suspicions of pain (67%), the presence of an obvious swelling (26%), and the presence of obvious decay (7%). There were often multiple indicators, including change in behavior (64%), halitosis (44%), drooling (23%), and aspiration of foods and/or liquids (9%). Before surgery, both the carers and dentists underestimated the treatment that would be required. In addition, no correlation was found between the pain rating provided by carers and the treatment required [
13]. Therefore, although carers may be familiar with the regular behavior of patients, their concerns appear to have little correlation with the clinical need for treatment.
In any case, it is clear that there are limited treatment options for patients that exhibit a certain level of resistance or lack of cooperation in the dental chair, and that general anesthesia is likely to be an appropriate method of treatment in such patients. However, the patients' lack of cooperation means that oral health professionals need to make decisions about whether a general anesthetic procedure is required without the relevant clinical data—such as descriptions and localization of pain, clinical examination, or radiographs—that would otherwise be used to develop diagnoses and appropriate treatment plans [
1415].
For this reason, many studies have questioned whether dentists can justify the use of general anesthesia as a means of routine dental review in these patients; even if they can, it is still not clear how long the review period should be in a patient who is otherwise uncooperative in the dental surgery [
16]. Furthermore, no literature exists on the suitability or safety of repeated general anesthesia in patients with special needs [
3]. Thus, this matter cannot be satisfactorily resolved on the basis of the current literature, raising the question of whether other forms of sedation could be used to facilitate treatment. The apparent consensus is that the presence of a behavioral problem, whether anxiety-related or associated with intellectual impairment, should not be the sole indicator for treatment under general anesthesia. Rather, the threshold for such treatment should be considered based on the relative success of behavioral management strategies and other forms of sedation. In the interests of the patient's life-long and ongoing care, general anesthesia should only be considered where other techniques have failed, and in recognition of the inherent risks, costs, and difficulties associated with treatment under general anesthesia [
2316].
Go to :

ASSESSMENT FOR TREATMENT UNDER GENERAL ANESTHESIA IN PATIENTS WITH SPECIAL NEEDS
Many organizations have published guidelines regarding the appropriate use of sedation and general anesthesia in dentistry among patients with special needs and in the general population [
171819202122]. These guidelines concern restrictions, educational requirements, and legislation in different jurisdictions and should be known by dental practitioners administering or treating patients under sedation. However, many of the same guidelines fail to discuss appropriate pre-operative assessment of patients who are to undergo general anesthesia. The aim of this assessment is to conduct clinical investigations prior to the anesthetic procedure and thereby reduce the risk associated with the surgery and anesthesia, improve the quality of peri-operative care, restore the patient to the desired level of function, and obtain informed consent for the procedure itself. Such assessments are usually based on medical records, a clinical interview, and physical examination where possible, as well as relevant additional tests [
23].
The consensus statement of the British Society for Disability and Oral Health specifically discusses the management of oral healthcare using general anesthesia in patients with special needs [
17]. The document provides guidance on the management of such patients throughout the assessment, admission, operative, and discharge stages. The statement recommends that preoperative assessments and consent procedures should be conducted by both the treating dental surgeon and the anesthesiologist where possible. The document also advises that these assessments should, where possible, include a detailed medical, social, and anesthetic history (including family history), a physical examination focusing on both general health and dentition, and any further diagnostic tests relevant to either the planned dental procedure or anesthesia [
17].
Prabhu et al. [
12] proposed using a standardized screening tool to assess the suitability of patients with special needs for treatment under sedation or general anesthesia. The tool combined a number of the aforementioned factors into one questionnaire to simplify and standardize the assessment process for less experienced practitioners. It used the American Society of Anesthesiologist's (ASA) Physical Status Classification System, as well as the Prognosis and Assessment of Risk Scale (PARS), to assess the risk associated with the patients' medical history (ASA/PARS Class I-V). In addition, the tool involved further assessments concerning the level of cooperation (cooperative, limited cooperation, uncooperative), nature of treatment procedure (limited treatment, complex treatment), type of anesthesia (local anesthesia, oral, inhalation, intravenous, general anesthesia), and type of setting most suitable for the patient's condition (primary/community, secondary/hospital). Attempts to validate the tool found that, although the management strategies identified were consistent after using the tool, there were problems with agreement among many of the measures [
12].
Unfortunately, such tools fail to take into account how these basic assessments can be significantly more complicated in patients with special needs. Although they may promote consistency in the process of assessment, lack of compliance from the patient is likely to hamper most forms of evaluation suggested—both medical and dental [
41424].
The dental assessment of any patient undergoing general anesthesia would ideally involve a thorough clinical examination and pre-operative radiographs to allow a treatment plan to be established. This would facilitate appropriate informed consent and adequate planning for the procedure. As mentioned above, one of the main indications for treatment of patients under general anesthesia is their lack of compliance during basic procedures—often including examination. As a result, a large part of treatment planning comprises estimations of the patients' treatment needs, as well as ensuring that adequate time, facilities, and equipment are available to accommodate these needs. There has been minimal discussion in the literature about whether other forms of sedation are sufficient to increase cooperation in patients with special needs and thus enable a more thorough pre-operative assessment [
5].
In addition to dental assessment, examination of the oral cavity may facilitate anesthetic assessment of the patient's airway. Airway management remains one of the most crucial aspects of patient care during sedation. Pre-operative assessment is often standardized using the Mallampati classification, which involves visual inspection of the distance from the base of the tongue to the roof of the mouth while the patient is in a seated position with their mouth open and tongue protruded. In this way, the airway is graded from class I to IV; higher classifications are associated with less clearance, difficulty with intubation, and an increased likelihood of obstruction [
25]. Other criteria often associated with potentially difficult airways include large protuberant incisors, large overbite, an inability to advance the mandible, small interincisal distance, large tongue, narrow or high-arched palate, shorter thyromental distance (including retrognathia and micrognathia), excessive mandibular soft tissue, short neck, increased neck circumference, and decreased range of neck motion [
2526]. In some jurisdictions, endotracheal intubation is not used routinely for deep sedation. Nonetheless, it is highly recommended to prevent complications associated with airway management [
27]. In addition, dental practitioners often prefer nasotracheal intubation to allow for treatment in the oral cavity. For this reason, inspection of the nasal cavity is recommended. Likewise, anesthesiologists should be aware that various congenital syndromes can alter airway anatomy [
24].
Furthermore, as part of the same physical assessment, the following parameters should also be measured: weight, height, vital signs (blood pressure and pulse), respiratory rate, oxygen saturation, and ability to obtain venous access. Unlike assessments of the oral cavity, many of these are minimally invasive and can be conducted in most patients, including those with special needs. These baseline details are essential as reference data for intra-operative monitoring and drug administration. Where possible, to supplement information about medical history, a cardiac and pulmonary examination is also recommended. Similarly, the patients' physical stamina during exertion could be observed as part of this examination in cases where such information is otherwise unobtainable [
232528].
In addition to these physical examinations, a thorough medical history is essential if patients are being considered for treatment under sedation or general anesthesia. This can present its own set of challenges. For example, most intellectually impaired patients will attend appointments with their carers. In many situations, these carers are not direct family members, and they may not be intimately familiar with the patient. This can present significant obstacles to dentists when trying to obtain suitable information regarding medical history and previous anesthetic experience [
614].
In addition to obtaining suitable information, dentists must also tailor and convey messages to the most appropriate carer during the pre-operative interview when dealing with patients who have special needs. For example, discussions regarding consent for treatment must be conducted with the correct responsible party in cases where the patient is unable to provide consent for themselves. Likewise, when the patient does not live with their family, pre-operative instructions regarding fasting and medication dosage, or post-operative instructions, need to be conveyed to the patient's primary carers [
623]. With regards to obtaining medical information, individuals living with family often have ongoing medical care provided by a general medical practitioner, with whom the family has developed a close relationship. In such cases, this professional may be the most valuable source of medical information. However, in the case of patients living in supported residential facilities, each resident should have a journal with copies of medical records and examinations, medications, and other relevant details [
6].
Unlike the general population, special needs patients are more likely to have multiple medical comorbidities that can complicate anesthetic risk assessment [
42429]. For example, patients may have underlying unstable systemic diseases, physical limitations that may affect physiological function, physiological or anatomical abnormalities associated with specific syndromes, multiple medical conditions, and psychiatric illness or cognitive impairment [
424]. In this regard, the impact of advanced age on physiological and functional reserve has been widely discussed. This is relevant to the present topic, because many patients with special needs experience changes akin to the symptoms of premature aging. Furthermore, individuals with intellectual disabilities may have undiagnosed medical problems because they do not convey conventional signs and symptoms [
4].
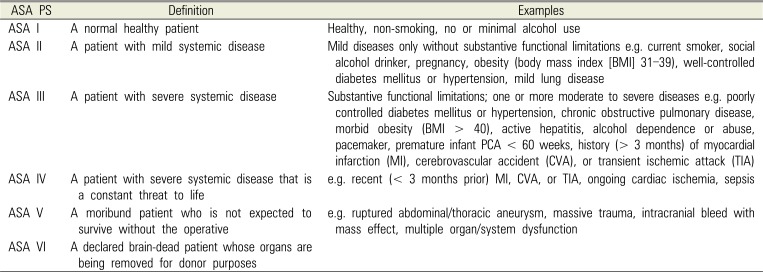
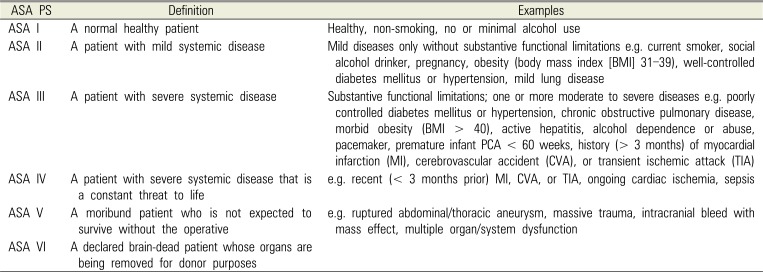
To quantify the impact of such medical conditions, the ASA Physical Status Classification System is often used in pre-anesthetic assessments. Designed initially as a statistical tool, rather than to prognosticate anesthetic risk, this system is often used as a guideline to assess patients; several studies have shown that it provides some indication of post-operative outcome [
4303132]. The physical status of the patient is categorized from ASA I to VI based on the presence and control of systemic disease. A summary of the classification is provided in
Table 1 [
30]. The literature has suggested that patients classed as ASA I or II are acceptable candidates for sedation, but that those in higher categories should be treated in hospital facilities [
4].
Table 1
The American Society of Anesthesiologists Physical Status Classification System (Oct 2014)
|
ASA PS |
Definition |
Examples |
|
ASA I |
A normal healthy patient |
Healthy, non-smoking, no or minimal alcohol use |
|
ASA II |
A patient with mild systemic disease |
Mild diseases only without substantive functional limitations e.g. current smoker, social alcohol drinker, pregnancy, obesity (body mass index [BMI] 31–39), well-controlled diabetes mellitus or hypertension, mild lung disease |
|
ASA III |
A patient with severe systemic disease |
Substantive functional limitations; one or more moderate to severe diseases e.g. poorly controlled diabetes mellitus or hypertension, chronic obstructive pulmonary disease, morbid obesity (BMI > 40), active hepatitis, alcohol dependence or abuse, pacemaker, premature infant PCA < 60 weeks, history (> 3 months) of myocardial infarction (MI), cerebrovascular accident (CVA), or transient ischemic attack (TIA) |
|
ASA IV |
A patient with severe systemic disease that is a constant threat to life |
e.g. recent (< 3 months prior) MI, CVA, or TIA, ongoing cardiac ischemia, sepsis |
|
ASA V |
A moribund patient who is not expected to survive without the operative |
e.g. ruptured abdominal/thoracic aneurysm, massive trauma, intracranial bleed with mass effect, multiple organ/system dysfunction |
|
ASA VI |
A declared brain-dead patient whose organs are being removed for donor purposes |
|

However, although such classifications may be useful as guidelines, they fail to address the complexity and individuality required of patient assessments. Often, when assessing a patient, it is more important to understand how their medical history can influence the risk associated with the procedure and appropriate patient management.
In particular, cardiac problems represent a significant concern for clinicians using general anesthetic procedures; to minimize risk in this regard, pre -operative assessments should aim to identify patients who require appropriate testing or therapeutic measures [
23]. The American College of Cardiology and the American Heart Association have published the most comprehensive guidelines concerning peri-operative cardiovascular evaluation [
33]. In particular, these guidelines mention concerns related to coronary artery disease, heart failure, symptomatic arrhythmia, pacemakers or implantable cardioverter defibrillators, or orthostatic intolerance. They also discuss the severity, stability, and management of these conditions [
33].
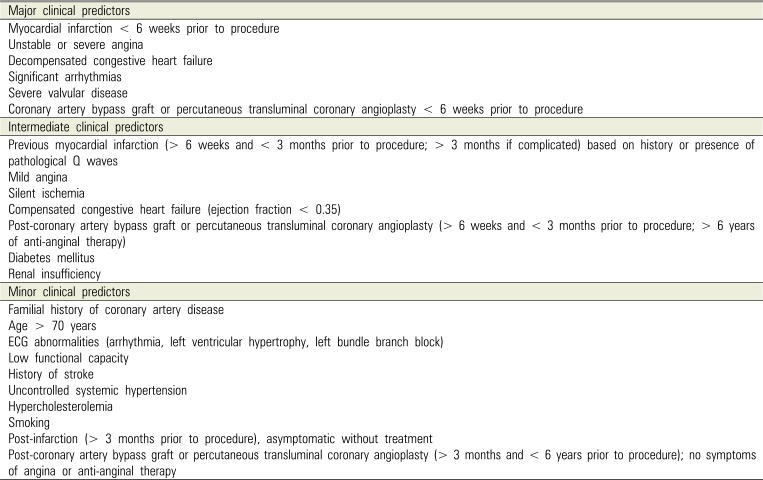
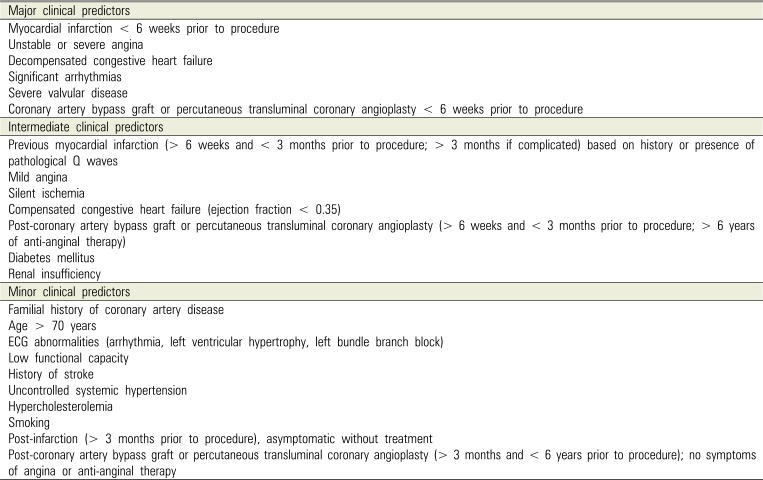
An extensive review of the implications of cardiac conditions and their management in light of general anesthetic procedures is beyond the scope of this article. However, existing guidelines suggest that the perioperative management of these patients depends on the stability of their condition. A summary of patient-related factors associated with peri-operative cardiac complications is provided in
Table 2.
Table 2
Patient-related predictors of risk for peri-operative cardiac complications [32]
|
Major clinical predictors |
|
Myocardial infarction < 6 weeks prior to procedure |
|
Unstable or severe angina |
|
Decompensated congestive heart failure |
|
Significant arrhythmias |
|
Severe valvular disease |
|
Coronary artery bypass graft or percutaneous transluminal coronary angioplasty < 6 weeks prior to procedure |
|
Intermediate clinical predictors |
|
Previous myocardial infarction (> 6 weeks and < 3 months prior to procedure; > 3 months if complicated) based on history or presence of pathological Q waves |
|
Mild angina |
|
Silent ischemia |
|
Compensated congestive heart failure (ejection fraction < 0.35) |
|
Post-coronary artery bypass graft or percutaneous transluminal coronary angioplasty (> 6 weeks and < 3 months prior to procedure; > 6 years of anti-anginal therapy) |
|
Diabetes mellitus |
|
Renal insufficiency |
|
Minor clinical predictors |
|
Familial history of coronary artery disease |
|
Age > 70 years |
|
ECG abnormalities (arrhythmia, left ventricular hypertrophy, left bundle branch block) |
|
Low functional capacity |
|
History of stroke |
|
Uncontrolled systemic hypertension |
|
Hypercholesterolemia |
|
Smoking |
|
Post-infarction (> 3 months prior to procedure), asymptomatic without treatment |
|
Post-coronary artery bypass graft or percutaneous transluminal coronary angioplasty (> 3 months and < 6 years prior to procedure); no symptoms of angina or anti-anginal therapy |

In particular, several areas of cardiovascular history are significant to anesthetic assessment:
Peri-operative morbidity. Procedures should be postponed until the patient's condition can be appropriately managed. In certain cases, beta-blockers may be used to assist with control by reducing demand on the heart while improving revascularization. Otherwise, pre-operative anti-hypertensive treatment should be continued throughout the peri-operative period [3233].
Myocardial and ischemic heart disease are associated with a higher incidence of post-operative heart failure. In fact, the risk of reinfarction is highest within 6 weeks. Therefore, elective procedures should be postponed for at least this long, but ideally for 6 months after a myocardial infarction, or until the patient's cardiologist is satisfied that the measures taken have addressed the problem of unstable angina [3233].
Valvular heart disease and arrhythmias often raise concerns for dental practitioners because they require appropriate management using antibiotic prophylaxis due to the risk of infective endocarditis. For the anesthesiologist, patients with these conditions present concerns related to the sufficiency of cardiac output because sedation and general anesthesia can alter the heart rate. Peri-operative monitoring of the patient's ECG, blood pressure, and pulse oximetry, in conjunction with pre-operative references, are usually sufficient for management [3233].
Patients with cardiac problems, and particularly those with heart failure, should be placed in a supine position post-operatively because they may experience symptoms related to pulmonary congestion [23].
Despite these complications associated with cardiac conditions, sedation is often considered an appropriate pharmacological measure to manage the stress associated with dental procedures and thus reduce cardiovascular stress. Importantly, when patients suffer from such conditions, it is essential that dentists liaise with the cardiologist to ensure that all relevant medical details have been obtained, appropriate adjunct testing has been carried out, and the patient is being managed in a manner appropriate to their individual needs [
232533].
Few respiratory diseases cause significant alterations to the anesthetic management of patients. Nonetheless, post-operative lung complications constitute a significant proportion of morbidity and mortality, often being reported at higher rates than cardiac complications [
2832]. Specifically, the literature mentions an increased risk of atelectasis, infection, the necessity for prolonged mechanical ventilation, respiratory failure, exacerbation of underlying chronic lung disease, and bronchospasm [
23]. One review found that the risk of complications increased with the presence of chronic lung disease, current smoking status, and procedures lasting longer than 3–4 hours, and that this risk is inversely proportional to the distance between the surgical incision and the diaphragm [
23]. In all pulmonary conditions, the most important aspects to consider in an assessment are the precipitating factors of disease exacerbation, the severity of the condition, and medical management. For patients with clinically significant chronic obstructive pulmonary disease, peri-operative oxygen should be administered with caution to avoid causing respiratory depression through elimination of the hypercapnic drive [
2328]. Additionally, a history of apnea should be recorded to ensure appropriate post-operative airway management. Ideally, patients with moderate to severe disease would be scheduled for their procedure in mid-to-late morning [
2328].
Essentially, all medical conditions can impact anesthetic procedures. Thus, the medical history should be assessed thoroughly to ensure that patients are managed in light of their individual needs. Most conditions can be managed effectively when controlled, but dentists should be aware of the implications for peri-operative care of these patients. For example, epilepsy is common among patients with special needs, particularly in those with neurological or global developmental delay disorders. Such patients should continue their prescribed medications during the peri-operative period, as anesthetic procedures are associated with an increased risk of seizures. Patients with poorly-controlled epilepsy or advanced neurological conditions, such as multiple sclerosis, muscular dystrophy, and myasthenia gravis, should be treated in hospitals with inpatient facilities due especially to the risk of respiratory depression and airway management [
28].
Similarly, patients with stable diabetes mellitus pose little concern for anesthesiologists. However, patients with poor glycemic control may have suffered damage to other organs. In these patients, further pre-operative assessment of cardiovascular and renal status may be required, and glucose levels should be monitored closely peri-operatively. Likewise, although gastrointestinal conditions are not of significant concern if controlled, patients with significant impairments to kidney and liver function may be immunocompromised to varying degrees. This may affect post-operative healing and pain management. In addition, significant liver disease should raise concerns regarding bleeding risk, and delayed recovery should be expected due to the impaired clearance of anesthetic medications [
28].
The medication regime of patients will often provide significant information regarding the status of their medical condition. For this reason, it should form a significant part of their anesthetic assessment. Patients being treated for gastroesophageal reflux should be noted, because they have an increased risk of aspiration during procedures involving deeper sedation. Likewise, the risk of adrenal insufficiency should be considered in patients taking corticosteroids; pre-operative and post-operative prophylactic adjustments to their medications may be warranted to prevent adrenal crisis. Although rare, awareness of allergies to medications will also help to prevent adverse reactions or drug interactions throughout the procedure [
232528].
Guidelines for the pre-anesthetic assessment of patients with special needs are limited, and those that have been published often fail to fully appreciate the complexity of assessing these patients [
1217]. Many of these assessments are affected by a lack of patient cooperation; often dentists must garner appropriate information from multiple sources regarding the patient's medical history. In addition, patients with special needs often present with complex medical histories, with further complications associated with other impairments that may be of minimal concern in the general population. For example, scoliotic or kyphotic spinal changes can impact airway management and intubation, as well as the risk of aspiration and the residual capacity of the lungs [
16]. Although these assessments form a basic pillar of anesthetic care, clinicians must accept that all of this information is unlikely to be available prior to the procedure. Thus, health professionals must exercise due diligence when treating these patients to ensure that they obtain and assess this information where available and to understand the relevant and potential complications. Such an approach will allow clinicians to appreciate and effectively address the treatment needs of patients with special needs.
Go to :

COMPLICATIONS EXPERIENCED BY PATIENTS WITH SPECIAL NEEDS TREATED UNDER GENERAL ANESTHESIA
As we can see, patients with special needs have high levels of medical comorbidity, as well as risks factors for complications associated with general anesthesia. However, there have been limited reports in the literature regarding morbidity and mortality in these populations. Moreover, most such reports were not specific to treatment conducted under general anesthesia, but also examined complications associated with other forms of sedation.
For instance, a retrospective study conducted by Caputo [
15] reported that 14% of their sample comprised patients with special needs; 79% of the patients reviewed had experienced post-operative issues, with the majority of them experiencing either vomiting (16%), nausea (12%), or both (28%). Other commonly reported issues included elevated temperature (15%) and decrease in appetite (6%) [
15]. Other studies have identified nausea and vomiting to be the most common post-operative complications after treatment under general anesthesia in special needs populations and children [
3435]. Conversely, bacteremia was only mentioned as a potential complication in one study of intellectually-disabled patients undergoing general anesthesia for dental treatment. However, the significance or level of bacteremia was not discussed [
36]. In other studies, the complication rates were much lower. In a retrospective review performed by Messieha [
4] and involving 363 patients with special needs who had been treated at the University of Illinois in Chicago, only two morbidities were noted. These involved other medical complications discovered after the general anesthetic procedure had been initiated. Similarly, a prospective study carried out by Boynes [
37] reported a complication rate of 23.8% for all forms of sedation and anesthesia in patients with special needs. This prospective study examined peri-operative complications in 202 patients with special needs who had been treated at the Special Needs Clinic of the University of Pittsburgh School of Dental Medicine; 95.8% of the peri-operative complications in these patients were classified as mild, and 4.2% as moderate. There were no severe complications. That is, none of the patients required hospitalization or emergency room treatment. In addition, there were no significant differences in incidence of complication among the various types of sedation. The most common problems encountered were airway obstruction (11.4%), followed by nausea or vomiting (9.4%), and hypotension (3.0%). Complications were more likely to be associated with patients classified as ASA III (12.4%) or Mallampati class III (9.9%), as well as with those who had been treated under intravenous sedation (19.8%). Treatment duration was not associated with an increased risk of complications [
37].
Based on medical diagnosis, those with cerebral palsy experienced the highest percentage of complications (44.4%)—most of these were associated with airway problems [
37]. Furthermore, 30.4% of patients experienceing a complication had autism, 29.2% had Down syndrome, 25.0% had Alzheimer's disease, 17.1% had other forms of intellectual disability, and 14.3% had a behavioral disorder. Amongst these conditions, nausea was the most common complication [
37].
Overall, these studies reported that complication rates in special needs populations were comparable to those among other patients in the community. However, none of the identified studies discussed the rates of cardiovascular or respiratory complications specific to procedures conducted under general anesthesia in patients with special needs. Most classified nausea and vomiting as minor complications, probably because these symptoms have a relatively minor impact on the medical status of patients. However, this judgement is made in the context of the general population. In patients with special needs, particularly those with intellectual impairments that commonly undergo these procedures, even these apparently mild adverse events may be distressing for both patients and carers, and thus should not be dismissed.
Several studies have suggested that the complication rates vary in patients with special needs. In fact, some have suggested they may be lower than in the general population, perhaps because the multiple previous anesthetic procedures may prevent complications [
437]. It may be that this is a result of effective record keeping, or that it reflects the level of care provided to patients with special needs in facilities that understand the potential morbidities associated with their histories. Conversely, it may be that many complications go unreported in these groups because there is a paucity of research in this area. Furthermore, in many situations, such complications may not have been associated with the anesthetic procedure, because some patients with special needs experience ongoing medical complications on a day-to-day basis.
The multiple comorbidities experienced by patients with special needs are similar to the many complications associated with aging. The relationship between aging and general anesthetic complications has been discussed more extensively throughout the literature. Several reviews have reported that the risk of mortality increases in age. Specifically, the risk of mortality is 2.2% in patients aged 60–69 years, but increases to 8.4% in patients over the age of 90 years, largely because the patients' physiological and functional reserve has deteriorated [
383940].
This may be exacerbated by the presence of co-existing diseases in the elderly population, just as with most patients who have special needs. Indeed, the leading causes of post-operative death are myocardial infarction and respiratory and cerebrovascular events [
38]. Therefore, cardiovascular disease and decreased cardiac function as a result of the aging process are thought to be significant risk factors highlighting the importance of cardiac and respiratory function in the anesthetic assessment of all patients [
38].
Further to these risks of mortality, increased morbidity has been associated with general anesthesia in elderly patients. Two studies conducted as part of the International Study of Postoperative Cognitive Dysfunction raised concerns regarding post-operative cognitive dysfunction in elderly patients [
4142]. One of these studies found that 21.8% of patients over the age of 60 experienced post-operative cognitive dysfunction 1 week after surgery, and that this had persisted in 7.7% of patients 3 months after the procedure. Furthermore, the increased risk was associated with the duration of surgery, a second operation, post-operative infections, and respiratory complications [
41].
From the literature available, it is clear that patients with special needs commonly treated under general anesthesia are at risk of significant morbidity and mortality. Surgeons must ensure that these issues are discussed if they are to obtain appropriate informed consent. However, health professionals have difficulties in this regard, because the literature is limited in this area, and because most studies have dismissed many reported post-operative complications as minor. This is dangerous and dismissive of the importance of individual patient assessment. Practitioners experienced in the treatment of patients with special needs will recognize that general anesthesia is associated with a significant risk, and that even minor complications can cause significant distress to these patients.
Go to :

CONCLUSIONS
Patients with special needs often require dental treatment to be adapted to meet their oral health needs. For a proportion of these patients, dental treatment is only possible through other modalities, such as sedation or general anesthesia. General anesthesia in particular provides a relatively safe option for the management of patients with behavioral and compliance issues. Unfortunately, due to the presence of medical comorbidities, these patients are at higher risk of peri-operative complications, although the available literature reported that these occur at a similar rate or less often than in the general population. Moreover, even minor morbidities may manifest in more significant ways in the special needs patient. Therefore, thorough pre-operative assessments are crucial to reducing the risk of complications associated with surgery, especially in this cohort. Although the anesthetic literature is replete with such assessments, clinicians must appreciate the difficulties associated with assessing patients who have special needs. Additionally, the presence of multiple impairments, medical conditions, and anatomical and physiological changes can significantly complicate this process, especially when not all of the information is attainable.
Furthermore, the available literature leaves many questions unanswered. For example, in patients with special needs who require general anesthesia to facilitate treatment, what constitutes an effective recall strategy for repeat procedure? Is it appropriate and safe for general anesthesia to be an ongoing part of their oral healthcare management? Likewise, is this form of management in the best interest of all patients who require a procedure under general anesthesia or are other sedation modalities safer and more amenable to the patient's care?
Effective management of patients with special needs, especially those treated under general anesthesia, requires an appreciation of the factors discussed above. Health professionals must understand and account for how these factors are relevant in each unique special needs patient.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download