Abstract
Drug-induced sleep endoscopy (DISE) is used to identify areas of upper airway obstruction, which occurs when patients with obstructive sleep apnea (OSA) snore. DISE enables effective diagnosis and appropriate treatment of the obstruction site. Among surgical treatment methods for OSA, maxillomandibular advancement surgery (MMA) is performed to move a jaw forward; the surgery has a high success rate for OSA treatment. In DISE, anesthetics such as propofol and midazolam must be administered to induce snoring while the patient is deeply sedated for an accurate diagnosis to be made. When inducing deep sedation in a patient with OSA, airway obstruction may increase, causing oxygen saturation to drop; airway interventions are necessary in such cases. Effective DISE and MMA surgery can be performed by administering propofol through target-controlled infusion while monitoring the bispectral index (BIS).
Obstructive sleep apnea (OSA) is sleep-associated respiratory distress characterized by snoring and repeated upper airway obstruction. Patients with OSA have cognitive disorders. In addition, excessive sleepiness interferes with daily activities and continued hypoxemia can induce lifestyle diseases including hypertension and arrhythmia. Continuous positive airway pressure (CPAP) devices or oral appliances may be used for OSA treatment. Surgical treatments including maxillomandibular advancement (MMA) may also be performed [1]. Drug-induced sleep endoscopy (DISE) is a method to visually identify causes of upper airway obstruction to increase the success rate of OSA treatment [2]. Drug-induced sleep induction must be performed to induce snoring before performing DISE. Anesthetics such as propofol, midazolam, and dexmedetomidine are primarily used for this procedure [3]. To increase the DISE success rate, drugs that induce near-normal sleep should be administered, and sleep and snoring must be maintained by ensuring anesthetics are within appropriate concentration ranges. However, when deep sedation is induced in a patient with OSA until the patient begins to snore, airway obstruction may become more severe than expected, and the patient may stop breathing, resulting in decreased oxygen saturation. Airway management must be performed, and airway interventions such as cardiopulmonary resuscitation (CPR) may be necessary. Oxygen administration is essential in DISE, and clinicians must monitor patients carefully to ensure respiratory failure or airway obstruction does not occur.
Dexmedetomidine has a lower rate of respiratory depression than propofol, is hemodynamically stable, and can induce sleep that resembles normal sleep [45]; therefore, it is reported to be more appropriate for DISE [6]. However, propofol has the advantages of rapid onset, maintenance of blood drug concentration through target-controlled infusion (TCI), and sedation depth control using a bispectral index (BIS) monitor, and is therefore recommended for DISE use [7]. In this study, we report a patient who underwent simultaneous successful DISE using propofol, followed by successful MMA surgery.
A 24-year-old male patient (height, 174 cm; mass, 85 kg) was diagnosed with severe OSA with reduced oxygen saturation based on polysomnography results (apnea-hypopnea index [AHI]: 72.9, respiratory disturbance index [RDI]: 75.5, minimum oxygen saturation: 78.0%). The patient showed a propensity for obesity (body mass index [BMI], 28), and used a CPAP device for excessive daytime somnolence.
Skeletal class II malocclusion and pronounced cervicomental fat deposition due to mandibular retrognathism were observed during a radiologic examination. MMA surgery accompanied by genial tubercle advancement (GTA) to secure and stabilize the pharyngeal airway was scheduled. In preparation for preoperative orthodontic treatment, the patient's posterior teeth were extracted, and he received orthodontic treatment for approximately 2.5 yr.
After preoperative orthodontic treatment was completed, MMA accompanied by anterior segment osteotomy (ASO) and GTA was scheduled. To investigate closure patterns at the obstruction site and velum and to assess improvement after MMA, DISE was performed immediately before general surgical anesthesia.
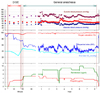
Immediately prior to surgery, the patient's hemoglobin and platelet levels were 15.7 g/dl and 271 × 103/µl, respectively. No abnormal liver or kidney functions or chest radiographs were observed. After submitting written consent, the patient fasted for 8 h, and entered the operation room without premedication. Hartman solution was administered through an 18-gauge intravenous catheter in the patient's left arm. To reduce nasal and intraoral stimulation during nasoendoscopy, local anesthesia was administered as a 10% lidocaine spray in both sides of the nasal cavity and 4% lidocaine gel in the oral cavity. A non-invasive blood pressure monitor, pulse oximetry, ECG, and BIS sensor were attached. Oxygen was supplied through a nasal cannula in the mouth at 5 L/min; capnography monitoring was performed simultaneously (Fig. 1). Before anesthesia, oxygen saturation was 98%, blood pressure was 117/77 mmHg, and breathing rate was 15 breaths/min.
To prevent excessive oral secretions during endoscopy, 0.5 mg of atropine was administered intravenously. To encourage sleep, lights were dimmed and noise was minimized. After 3 ml of 1% lidocaine was intravenously administered for pain reduction within blood vessels, propofol (Fresofol 2%, Fresenius Kabi, Bad Homberg, Germany) was intravenously injected using an Orchestra syringe pump system (Fresenius Orchestra, Fresenius Kabi) through TCI to induce deep sedation. Propofol was initially infused at an effect site concentration of 2.5 µ g/ml, then increased to 3.0 µg/ml when sleep was not induced after 3 min. After 5 min of infusion, the patient's BIS decreased to 70-80, the patient lost consciousness (Fig. 2), and began to snore appropriately. An endoscope was inserted into the right nostril to check the tubular site and the obstruction site during snoring. The BIS decreased over time and the patient's breathing became inhibited. The patient's mandible was lifted forward to assess enlargement of the airway space. During DISE, the patient's BIS was approximately 70 and oxygen saturation was maintained at 90-95%. The respiratory rate was 5-12 breaths/min, end tidal carbon dioxide (ETCO2) was 40-50 mmHg, and blood pressure was 90-120/40-60 mmHg.
It took 15 minutes from the drug administration to DISE termination. The velum, oropharynx, tongue, and epiglottis were assessed for evidence of circular obstruction. As a moderate to high degree of airway enlargement following mandible advancement was expected, surgery was performed.
To induce general anesthesia, the target concentration of propofol was increased to 5.0 µg/ml, and remifentanil (Ultiva®, GlaxoSmithKline, Brentford, London, UK) was administered at an effect site target concentration of 5.0 ng/ml. A 40 mg dose of rocuronium was intravenously administered as a muscle relaxant. After confirming sufficient muscle relaxation, nasotracheal intubation was performed using a laryngoscope and a 7.0 gauge RAE tube. Anesthesia was maintained with propofol and remifentanil infused at target concentrations of 4-5 µg/ml and 5-10 ng/ml, respectively, while monitoring BIS and vital signs. Rocuronium was continuously administered. A LeFort I osteotomy with ASO was performed on the maxilla to advance the posterior region using the extraction space, and to advance the maxilla by 3 mm overall. For the mandible, bilateral sagittal split ramus osteotomy (BSSRO) with ASO was performed to advance the left side of the mandible 7.5 mm and the right side 6 mm. The final location of the mandible was fixed with a wafer, and then GTA was performed to advance the chin by 6 mm.
After the patient recovered spontaneous breathing, he was returned to the recovery room. In the recovery room, the patient fully regained consciousness, and his breathing patterns and vital signs returned to normal. After monitoring the patient for 1.5 h, swelling was observed underneath the tongue and throughout the face. Extubation was delayed and the patient was returned to the intensive care unit while maintaining spontaneous breathing. In the intensive care unit, the patient was administered 35% humidified oxygen. No excessive secretion was observed in the endotracheal tube. Extubation was performed the next morning after confirming only a small volume of submandibular drain and no swelling. No breathing difficulties were observed, and oxygen saturation was maintained at 98%. No postoperative surgical or medical complications were observed. Postoperative pain was managed with a patient-controlled analgesia device, and the patient was discharged 1 week later. At the time of the patient's next visit to an outpatient clinic, discomfort while sleeping, which is experienced by patients after surgery, was significantly reduced.
OSA is a complete or incomplete airway obstruction that repeatedly occurs during sleep, which leads to decreased blood oxygen saturation. Patients with OSA show anatomical abnormalities of the upper airways and physiological alterations. Fat accumulation around the upper airways can be observed in obese patients with OSA. The incidence of OSA is estimated to be 0.89% in adults aged 25 years or older, and is higher among men, obese patients, and patients with hypertension and diabetes [8]. Patients with symptoms of OSA exhibit additional risk factors, including cardiovascular events, systemic inflammation, excessive daytime sleepiness, and fatigue [9]. Severity of OSA can be classified as mild (AHI 5-15), moderate (AHI 15-30), or severe (AHI > 30) [10]. The patient in this case had an AHI of 72.9.
OSA treatment can be nonsurgical, including weight loss, behavioral modification, and use of CPAP or oral appliances, or surgical, including tracheostomy, UPPP, isolated hard or soft tissue surgery, and MMA [1]. MMA can enlarge the velo-orohypopharyngeal airway and is indicated for patients with severe OSA who cannot use a CPAP device. It has a high success rate, ranging from 60% to 100% [10]. In MMA, the maxilla and mandible are advanced; accordingly, the velopharyngeal aponeurotic attachment in the posterior region of the maxilla, and the tongue base with pterygomandibular aponeurotic attachment in the linguo-posterior region of the mandible are stretched. This creates tension in the aponeurosis, causing the cross-sectional area and the volume of velo-orohypopharyngeal airway to increase, which improves airflow [9].
Methods to assess OSA other than DISE include physical examination of the upper airways, lateral cephalometry, computed tomography (CT) scanning, and polysomnography. However, these tests are performed while the patient is awake and do not accurately assess the airway conditions during sleep, as respiratory drive, muscle tone, and reflex sensitivity are different. DISE, introduced by Croft and Pringle in 1991 [2], assesses upper airway obstruction that occurs during snoring. Through DISE, clinicians visually observe upper airway obstruction that occurs during sleep, and can accurately diagnose airway obstruction in patients with sleep apnea. Assessment of the site and pattern of airway obstruction and the effectiveness of oral devices may help clinicians determine appropriate treatment methods. In the present case, obstruction of the velum, oropharynx, tongue, and epiglottis, as well as circular obstruction upon velum closure, were assessed through DISE, and airway enlargement of a moderate to high degree could be expected during MMA [11].
Profopol, midazolam, and dexmedetomidine are used in DISE as sleep-inducing agents. When choosing an ideal drug for DISE, understanding of sedation-induced neuropharmacology and sleep-related neurophysiology is necessary. Airway obstruction during sleep usually occurs during non-rapid eye movement (NREM)1/NREM2 and rapid eye movement (REM) sleep, and is relatively less severe during NREM3 [12]. An ideal drug for DISE should be able to be administered intravenously, have rapid onset, and have a short half-life, which allows for easy control of sedation depth. In addition, it must have low residual effects so the patient can safely return home after sleep endoscopy, and have amnestic properties so the patient will not remember the DISE procedure.
Recent studies report dexmedetomidine induces a state that resembles normal sleep, has a lower rate of respiratory depression and is more hemodynamically stable than propofol, and is more appropriate for DISE [6]. The onset of dexmedetomidine takes approximately 5 minutes, and it takes time to control the concentration [613]. Propofol has the advantage of rapid onset, easy concentration control using TCI [14], and sedation depth control using a BIS monitor; it is therefore recommended as a primary drug for DISE [7].
Although DISE is useful, there is still no standardized protocol available, and observations made during DISE and natural sleep can differ. As observations are made under an endoscope, different results may also be obtained by different examiners [15]. No study has investigated how effectively DISE induces natural sleep, or compared natural sleep and DISE in the same patient. A minimum of 1.5 µg/ml of propofol is needed for the patient to endure the stimuli from the flexible endoscope, and 2.33 µg/ml is needed on average [16]. Depth of sedation can be controlled according to the BIS. A BIS of 65-75 indicates moderate sedation; consciousness is inhibited but the patient can still respond to verbal orders and mild stimuli. Airway intervention is not required. Spontaneous breathing and cardiovascular functions are maintained and the patient begins to snore lightly [17]. When a patient reaches deep sedation, spontaneous breathing may become difficult, cardiovascular functions are conserved, and an airway intervention may be required [17]. The BIS is 50-60 at this stage. Extra care is required for patients with OSA, as they are at high risk of airway collapse [18]. An assessment of airway collapsibility following propofol administration at three different blood concentrations (2.5, 4.0, and 6.0 µg/ml) through TCI found that average upper-airway collapsibility significantly increased [19].
Drug-induced sedation is a high-risk procedure for patients with OSA, as oxygen saturation in these patients drops even during normal sleep. In drug-induced sleep, reflexes of the muscles and mucous membranes of the upper airways become inhibited, making airways more prone to obstruction and decreasing oxygen saturation, although the severity of the phenomenon depends on the sedation depth. For this reason, capnography and pulse oximetry monitoring are essential. For most patients under moderate sedation, the condition can be improved by administering a stimulus during respiratory inhibition or performing the jaw thrust maneuver. If necessary, Ambu bagging can be performed to calm the patient. In conclusion, we successfully performed DISE by administering propofol through TCI. We also performed anesthesia during MMA surgery by continuously infusing propofol and remifentanil intravenously.
Figures and Tables
References
1. Hong SD, Dhong HJ, Kim HY, Sohn JH, Jung YG, Chung SK, et al. Change of obstruction level during drug-induced sleep endoscopy according to sedation depth in obstructive sleep apnea. Laryngoscope. 2013; 123:2896–2899.

2. Croft CB, Pringle M. Sleep nasendoscopy: A technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci. 1991; 16:504–509.

3. Yoon JY, Kim EJ. Current trends in intravenous sedative drugs for dental procedures. J Dent Anesth Pain Med. 2016; 16:89–94.

4. Chi SI, Kim HJ, Seo KS. Dexmedetomidine intravenous sedation using a patient-controlled sedation infusion pump: A case report. J Dent Anesth Pain Med. 2016; 16:55–59.

6. Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS. A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope. 2016; 126:763–767.

7. Traxdorf M, Tschaikowsky K, Scherl C, Bauer J, Iro H, Angerer F. Drug-induced sleep endoscopy (dise) with target controlled infusion (tci) and bispectral analysis in obstructive sleep apnea. J Vis Exp. 2016.

8. Rodrigues AP, Pinto P, Nunes B, Barbara C. Obstructive sleep apnea: Epidemiology and portuguese patients profile. Rev Port Pneumol (2006). 2017; 23:57–61.

9. Kim T, Kim HH, Hong S, Baek SH, Kim KW, Suh SH, et al. Change in the upper airway of patients with obstructive sleep apnea syndrome using computational fluid dynamics analysis: Conventional maxillomandibular advancement versus modified maxillomandibular advancement with anterior segmental setback osteotomy. J Craniofac Surg. 2015; 26:e765–e770.
10. Doff MH, Jansma J, Schepers RH, Hoekema A. Maxillomandibular advancement surgery as alternative to continuous positive airway pressure in morbidly severe obstructive sleep apnea: A case report. Cranio. 2013; 31:246–251.

11. El AS, El H, Palomo JM, Baur DA. A 3-dimensional airway analysis of an obstructive sleep apnea surgical correction with cone beam computed tomography. J Oral Maxillofac Surg. 2011; 69:2424–2436.

12. Ratnavadivel R, Chau N, Stadler D, Yeo A, McEvoy RD, Catcheside PG. Marked reduction in obstructive sleep apnea severity in slow wave sleep. J Clin Sleep Med. 2009; 5:519–524.

13. Shteamer JW, Dedhia RC. Sedative choice in drug-induced sleep endoscopy: A neuropharmacology-based review. Laryngoscope. 2017; 127:273–279.

14. Roblin G, Williams AR, Whittet H. Target-controlled infusion in sleep endoscopy. Laryngoscope. 2001; 111:175–176.

15. Gillespie MB, Reddy RP, White DR, Discolo CM, Overdyk FJ, Nguyen SA. A trial of drug-induced sleep endoscopy in the surgical management of sleep-disordered breathing. Laryngoscope. 2013; 123:277–282.

16. Rabelo FA, Braga A, Kupper DS, De Oliveira JA, Lopes FM, de Lima Mattos PL, et al. Propofol-induced sleep: Polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol Head Neck Surg. 2010; 142:218–224.

17. Donaldson M, Goodchild JH. Use of bispectral index system (bis) to monitor enteral conscious (moderate) sedation during general dental procedures. J Can Dent Assoc. 2009; 75:709.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download