Abstract
Patients with severe gag reflex (SGR) have difficulty getting the treatment they require in local clinics, and many tend to postpone the start of their treatment. To address this problem, dentists have used behavioral techniques and/or pharmacological techniques for treatment. Among the pharmacological methods available, propofol IV sedation is preferred over general anesthesia because it is a simpler procedure. Propofol in combination with remifentanil is characterized by stable sedative effects and quick recovery, leading to a deep sedation. Remifentanil acts to reduce the pain caused by lipid-soluble propofol on injection. The synergistic effects of propofol-remifentanil include reduction in the total amount of drug required to achieve a desired sedation level and anti-emetic effects. In this case report, we outline how the use of propofol-remifentanil IV sedation enabled us to successfully complete a wide range of dental treatments in a patient with SGR.
Gag reflex (GR) is described as a normal defense mechanism that prevents foreign bodies from entering the trachea, pharynx, or larynx. However, some patients have a severe gag reflex that makes it difficult for them to receive dental treatment, and they may consequently miss or postpone treatment.
The etiology of GR is categorized as either somatic or psychologic. Somatic responses occur in response to physical stimuli in the posterior palate, base of tongue or throat, while psychologic responses are induced by fear or horror [1]. A psychological GR can be also triggered by fear and anxiety associated with previous dental care, in the absence of physical stimuli.
Research has continued to manage GR in patients with SGR by applying behavioral techniques and pharmacological techniques. At the same time, the IV sedation method, which is commonly used to relieve gagging and fear during gastrointestinal endoscope examination, has been introduced and widely used for dental treatment [2]. In this case report, we present a case of effective use of propofol-remifentanil IV sedation for dental treatment on a patient with SGR.
A 41-year-old male patient (60 kg, 170 cm) without significant medical history was admitted to our hospital for restorative and prosthetic treatment. During his visit, consent for release of information was obtained. It was found that he suffered from SGR and postponed dental treatment for a long time due to his fear and anxiety about dental care.
The patient had undergone treatment in local clinics using various behavioral and pharmacological techniques, but could not continue treatment due to severe gagging. He visited our hospital after discovering the availability of sedation-based care. After admission, he showed considerable fear and anxiety during routine oral examinations, and had GR when the dental mirror was placed inside his mouth, forcing us to examine his anterior teeth, and take a panoramic radiograph only. The patient requested IV sedation to have a periapical radiograph taken, and his posterior teeth examined. After consultation with the patient, we decided to both treat his anterior teeth, and examine his posterior teeth under the 1st sedation.
On the appointment date, the patient returned to the hospital after an 8-hour fast. After a systemic examination, sedation was administered. Supplemental oxygen at 2 L/min was supplied via a nasal cannula, and the IV line established using conventional venipuncture for propofol-remifentanil administration (Fig 1). A target controlled infusion (TCI) device (Orchestra Infusion Workstation, Fresenius Vial, Brezins, France) was used to set and administer remifentanil at a target plasma concentration of 1.0 ng/ml, which was then followed by the infusion of propofol at a target plasma concentration of 1.3 µg/ml under neuroleptanalgesia (Fig 2). After administration, upon the observation of ptosis, we began the oral examination.
During examination, the patient remained conscious and expressed his fear and anxiety, but his gagging significantly diminished, making it possible to examine the posterior teeth, carry out calculus debridement, place anterior injections and restore anterior teeth, in the absence of SGR.
When GR reappeared slightly, we increased the target concentration of drugs to control gagging, and then restored it to the previous level. Meanwhile, the patient remained conscious, maintained respiration, and cough caused by water aspiration, thus showing no sign of deep sedation. During treatment, the patient maintained a stable respiratory rate of 10 breaths/min, blood pressure of 140-122/95-72 mmHg, pulse rate of 80-90 bpm, and SpO2 of 93-98%. After treatment, the infusion was stopped and the nasal cannula removed. The patient immediately left the dental chair to go to the recovery room. At the time of discharge, consciousness was fully regained, and he left after 20-30 minutes with his caregiver.
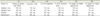
The patient has subsequently undergone IV sedation six times. The procedures and dental treatment, sedation and operation time, and dose of drugs administered are detailed in Table 1.
Gag reflex is a natural defense response elicited by the stimulation of posterior intraoral structures. It prevents foreign bodies from entering the upper respiratory tract by contracting oropharyngeal muscles and removes unwanted irritants. The levels of sensitivity and extent of GR tolerance vary among people. The etiology of GR has been categorized as either somatic or psychologic [3]. Somatic responses are induced by intraoral stimuli i.e., GR occurs due to a foreign body sensation being felt when dental instruments enter the posterior intraoral region. The intraoral trigger zones include palatoglossal and palatopharyngeal folds, base of tongue, palate, uvula, and posterior pharyngeal wall [4]. Psychological responses are associated with negative memories, fear or anxiety developed from previous dental care, and may occur without a direct stimulus.
Many dentists have used behavioral and/or pharmacological techniques to manage GR for the last several years [5]. Behavioral techniques are designed to reduce gagging reactions by maintaining conversation, distracting attention, and stimulating the intraoral area steadily and repeatedly to desensitize the patient. The effects of behavioral techniques vary among patients; even if the techniques work for some patients, it may not help them undergo dental treatment successfully. Another disadvantage is that the techniques are time-consuming. Topical anesthesia of the oral mucosa has been effective for some patients but worsened symptoms in others, with general anesthesia being chosen as an alternative. The risks associated with general anesthesia and high costs still make it a last resort, and there is high demand for IV sedation because of its relatively high level of safety, and quick recovery [5].
Routes of sedation include oral, inhalation, and intravenous injection. Oral sedation is characterized by different times for onset of action and low sedation success, while inhalation sedation is characterized by low sedative and analgesic effects, low potency, and ineffectiveness. In contrast, IV sedation delivers quick onset time of sedation and allows control of sedative effects, rapid recovery, and safety.
Propofol is highly lipid-soluble and provides quick redistribution, rapid onset of action, short duration of effect, and rapid recovery with minimal postanesthetic side effects, making it popular for IV sedation [6]. In addition, low incidences of nausea or vomiting postanesthesia enable early discharge and, when an appropriate dose is used, anxiolytic effects like midazolam and amnesiatic effects are observed [7]. However, propofol causes a 30% drop in arterial blood pressure due to decreases in peripheral vascular resistance and myocardial contractility. This result can be partly avoided by reducing the rate of drug ingestion. Therefore, propofol must not be used for hypovolemic patients. Propofol can still exhibit severe respiratory suppression phenomenon by suppressing hypoxic ventilation, and hence, the administration of supplemental oxygen and specialist supervision are required.
Remifentanil is a fast-acting opioid analgesic with minimal residual effects, and acts on opioid receptors in the brain and spinal cord. Remifentanil is rapidly broken down by nonspecific esterases in blood and tissues, leading to a final elimination half-life of less than 10 min, and a context-sensitive half-life of 3 min with almost no accumulation, regardless of duration of infusion [89].
Remifentanil in combination with propofol reduces the total dose of propofol required to achieve deep sedation, resulting in reduced recovery time and reduced severe pain related to sedation. A study comparing the incidences of SGR after the administration of remifentanil and propofol reported that remifentanil is more effective in suppressing GR when the patient can cooperate during the treatment process because propofol has stronger sedative effects than attenuating effects on GR [1011].
However, prolonged use of propofol can cause propofol infusion syndrome, which induces lipidemia and metabolic acidosis, and reduced cardiac contraction due to lowered peripheral vascular resistance attributable to suppression-induced vasoconstriction. Thus, arterial blood pressure can drop due to decreasing preload. Remifentanil therefore can raise the risk of cardiac arrest when administered to children less than 3 years old, elderly patients, and patients taking drugs to reduce heart rate, and respiratory suppression when its dose for induction of anesthesia is excessive. Immediate airway clearance is therefore required, and administration should be performed under specialist supervision. To avoid excessive administration, infusion pumps like TCI are needed.
This case report describes a patient with SGR admitted to our hospital after failing to get treatment from local clinics. We could complete various dental procedures successfully without triggering SGR. Unlike general anesthesia, conscious sedation maintains consciousness during the treatment process, making it easy to monitor patient symptoms and signs, and is useful for procedures where patient cooperation is needed. Since then, general treatment that could be performed without stimulating the intraoral region was provided in an outpatient setting, as patient sensitivity to GR decreased with increasing familiarity with the dental environment and relaxation [12]. This case confirms that patients with SGR can receive almost all dental treatments under IV sedation. It is also likely that effective behavioral outcomes, and desensitization of the intraoral region, help increase the threshold of gag reflex.
In approximately 60 cases treated over the last 4 years, there has been no situation in which severe gag reflex was not controlled and treatment had to be discontinued. In conclusion, we report that propofol-remifentanil IV sedation is an effective method for reducing SGR, and enables almost all dental treatments to be completed successfully, along with positive effects on behavior management.
Figures and Tables
Table 1
Dental treatment provided under each of six sedative states (IV)
References
1. Kramer RB, Braham RL. The management of the chronic or hysterical gagger. ASDC J Dent Child. 1997; 44:111–116.
2. Dies DF, Clarkston WK, Schratz CL. Intravenous ketorolac tromethamine versus meperidine for adjunctive sedation in upper gastrointestinal endoscopy: a pilot study. Gastrointest Endosc. 1996; 43:6–9.

3. Saunders RM, Cameron J. Psychogenic gagging: identification and treatment recommendations. Compend Contin Educ Dent. 1997; 18:430–433.
4. Meeker HG, Magalee R. The conservative management of the gag reflex in full denture patients. N Y State Dent J. 1986; 52:11–14.
5. Bassi GS, Humphris GM, Longman LP. The etiology and management of gagging: A review of the literature. J Prosthet Dent. 2004; 91:459–467.

6. O SR, Lee J. Intravenous sedation using propofol and midazolam in the exaggerated gag reflex patient's dental implant treatment: a case report. J Korean Dent Soc Anesthesiol. 2010; 10:27–33.

7. Tesniere A, Servin F. Intravenous techniques in ambulatory anesthesia. Anesthesiol Clin North America. 2003; 21:273–288.

8. Korean Dental Society of Anesthesiology. Dental Anesthesiology. 3rd ed. Seoul, Koonja: 2015. p. 440–518.
9. Glass PS, Dyar OJ, Jacobs JR, Reves JG. Intravenous anesthetic drugs: Infusion regimens. Int Anesthesiol Clin. 1991; 29:73–82.

10. Moerman AT, Herregods LL, De Vos MM, Mortier EP, Struys MM. Manual versus target-controlled infusion remifentanil administration in spontaneously breathing patients. Anesth Analg. 2009; 108:828–834.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download