Abstract
Background
Every patient who undergoes mandibular third molar surgery is concerned about post-operative pain. Indeed, previous researchers have used various methods to treat such pain. This study aimed to assess the effectiveness of sublingual injection of dexamethasone (8 mg) to treat post-operative pain after mandibular third molar surgery.
Method
This was a randomized, double-blind, split-mouth, clinical trial, involving 48 healthy patients who required surgical removal of two mandibular third molars with similar bilateral positions. All operations were performed by the same experienced surgeon. The patients were randomized into a study group (8 mg dexamethasone injection) and a placebo group (normal saline injection). Both interventions were injected into the sublingual space immediately after local anesthesia, 30 min before the first incision. The study group received an 8 mg dexamethasone injection, while the placebo group received a normal saline injection. The wash period between the patients' two operations was 3 to 4 weeks. Pain was assessed by recording the number of analgesic tablets (rescue drug) consumed, as well as by noting the patients' responses to the visual analog scale (VAS) on the first, second, and third days after surgery.
Surgical extraction of the mandibular third molar is the most common procedure in oral surgery, and all clinicians must consider post-operative pain after mandibular third molar surgery. Indeed, many dental researchers have focused on reducing post-operative pain [12345].
Although the inflammatory response mediates wound healing, an excessive response can lead to a variety of complications. Therefore, several approaches have been taken to overcome post-operative pain. Clinicians mostly prescribe non-steroidal anti-inflammatory drugs, opioids, or a combination of both. However, corticosteroids, especially dexamethasone, are among the most effective drugs in terms of overcoming post-operative pain, facial swelling, and mouth opening (trismus) [123456]. In fact, facial swelling and inflammation contribute towards pain and mouth opening, even though inflammation plays an important role in wound healing.
Dexamethasone has numerous and widespread effects, including alterations in carbohydrate, protein, and lipid metabolism, maintenance of fluid and electrolyte balance, and preservation of normal function in the cardiovascular and immune system, as well as in the kidneys, skeletal muscle, endocrine system, and nervous system. Dexamethasone endows organisms with the capacity to resist noxious stimuli and environment change [789].
The analgesic effect of dexamethasone is thought to be mediated through its anti-inflammatory and immunosuppressive activity, which result in decreased production of various inflammatory mediators that amplify and maintain pain perception [1011]. Mirzai et al. have demonstrated that corticosteroids, in combination with bupivacaine, have an analgesic effect, both locally in the spine and systemically. Furthermore, dexamethasone microspheres prolong block duration in both animal and human studies [12].
Similarly, Movafegh et al. combined 8 mg of dexamethasone with 34 mL of 1.5% lidocaine. They then compared the duration of sensory and motor blockade between this drug combination (study group) and 1.5% lidocaine alone (control group ). In the study group, the sensory blockade lasted 242 ± 76 min, whereas it lasted 98 ± 33 min in the control group. The motor blockade lasted 310 ± 817 min in the study group and 130 ± 31 min in the control group. All of these differences were significant [13].
The aim of the present study was to evaluate the effectiveness of sublingual injection of dexamethasone (8 mg) on postoperative pain after mandibular third molar surgery. In this regard, many clinicians report corticosteroid use in very general terms, and they rarely mention details regarding the type, dosage, and duration of administration.
The protocol of this investigation was approved by the research ethics committee of Mahidol University Institutional Review Board (COA No. MU-DT/PY-IRB 2016/021.2303), and written informed consent was obtained from all of the participants before surgery.
Forty-nine consecutive patients were enrolled in the study; all were aged between 18 and 30 years and underwent bilateral extraction of impacted third mandibular molars in the Department of Oral and Maxillofacial Surgery. The minimum sample size—calculated using the world health organization (WHO) sample size calculator—was 32 patients, with a 5% level of significance, a power of 60%, and a confidence interval of 17.53%.
This randomized, prospective study with a split-mouth, clinical trial design was carried out at the Department of Oral and Maxillofacial Surgery of the Faculty of Dentistry, Mahidol University. The study was managed by a single investigator and randomized using coin tosses. All operations were performed by the same experienced surgeon. Both the surgeon and the patients were blinded to the study design.
To qualify for inclusion in the study, the patients were required to (1) be healthy (ASA I), (2) have bilateral symmetrically impacted third molars, as visualized using on panoramic investigation and defined according to the Pell and Gregory classification [14], and (3) have no systemic disease.
Patients were excluded from the study if they (1) had undergone treatment using analgesic or any related drugs ≤ 15 days prior to surgery, (2) were pregnant, (3) were allergic to corticosteroids, (4) had lesions around the impacted mandibular third molars, (5) did not fulfil postoperative instructions or adhere to the follow-up regime.
All the impacted mandibular third molars were removed using the same standard surgical technique; the patients were given local anesthesia (two capsules of 4% articaine with 1:100,000 epinephrine). After inferior alveolar nerve block and local infiltration (numbness of the lip and tongue), 2 mL of normal saline with 8 mg of dexamethasone, or 2 mL of normal saline alone, was injected into the sublingual space. Subsequently, the standard technique of lower third molar surgery was performed. The washout period between the two mandibular third molar operations was at least 3 weeks.
Pre-operatively, no medication was given to the patients; however, after each operation, all patients were given postoperative instructions and asked to provide a pain score using the 100 mm VAS on the first, second, and third postoperative days. The duration of surgery from the first incision to the final suture was also recorded, as was rescue drug consumption (paracetamol; 500 mg) during the 7 days after surgery.
To compare between protocols (dexamethasone and placebo), statistical analysis was performed using the Statistical Package for the Social Science (SPSS version 22; SPSS Inc., USA). To evaluate the normality of the data, the Shapiro–Wilk test was used, with the application of either parametric or non-parametric tests. All P-values < 0.05 were considered significant.
In total, 97 impacted mandibular third molar teeth were surgically removed in this investigation. One of the patients underwent only one operation (using normal saline), and was excluded from the study. Data were collected from the remaining 48 patients between March and June 2016 at the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University, Bangkok. Data regarding sex and duration of surgery are provided in Table 1. There was no significant difference in the duration of surgery between the dexamethasone and placebo groups.
The angulations of the mandibular third molars in this study were as follows: mesioangular (37.5%), horizontal (33.4%), vertical (18.7%), and distoangular (10.4%), as shown in Table 2. Table 3 shows the classifications of the mandibular third molars in this study: there were 10 patients in class IIA, 26 patients in class IIB, nine patients in class IIC, one patient in class IIIA, and 2 patients in class IIIB.
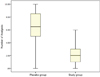
There was a significant difference between the dexamethasone and placebo groups with regard to pain on the first, second, and third days after surgery, based on the 100 mm VAS (Table 4 and Figure 1). Furthermore, a significant difference occurred between the groups regarding analgesic consumption (Figure 2).
The removal of impacted mandibular third molars can be associated with intra-operative and postoperative complications, such as nerve damage, tooth or root displacement into the adjacent anatomical spaces, mandibular fracture, facial swelling, trismus, and pain. However, the incidence of these postoperative complications is relatively low, and they can be minimized or avoided through comprehensive pre-operative evaluation, thorough treatment planning, and by following standard principles of surgery [115161718].
To overcome postoperative complications such as pain, which is a normal physiological response to surgery, clinicians and researchers have used low laser therapy [19], non-steroidal anti-inflammatory drugs [202122232425], opioid drugs [26], cold-ice therapy [27], acupuncture [262829], tube drains [30], secondary closure of the surgical wound [31], and corticosteroids [1347891011121315161718].
The present study evaluated the efficacy of dexamethasone in this regard; it represents a class of drugs commonly prescribed pre-operatively before oral and maxillofacial procedures. To this end, symmetrical mandibular third molar surgery was chosen as the study subject. Cooper [32] stated that three categories of surgery lead to dental pain: complicated oral, periodontal, and impacted third molar removal. In particular, mandibular third molar removal is associated with moderate and severe pain.
The present study was a split-mouth, randomized, double-blind, clinical trial; it was performed using a placebo to reduce bias. Because we assessed symmetrical mandibular third molar teeth on either side of the same patient (split-mouth), our study had advantages in terms of the difficulty and duration of surgery, as well as the patients' perception of postoperative pain. There were no significant differences between the groups with regard to the surgical procedures or demographic data (sex, age, number of operations, duration of surgery, difficulty of mandibular third molar surgery according to the Pell and Gregory classification [14], incision design, bone removal, and tooth sectioning).
Dexamethasone has often been considered in the management of pain, swelling, and trismus after mandibular lower third molar surgery, and it has been used previously to test the efficacy of pre-emptive analgesia for postoperative pain control. For instance, Boonsiriseth et al. [1] recommended that pre-operative dexamethasone (8 mg), both by intramuscular injection or oral consumption can decrease postoperative pain, facial swelling, and limited mouth opening.
Another study by Mojsa et al. concluded that a submucosal injection of dexamethasone (4 mg) both before and after surgery eased pain more effectively. The same researchers reported that pre- and postoperative submucosal injection of dexamethasone alleviated pain to a similar degree, and that there was no difference in the total rescue analgesic intake [33]. However, in our study, dexamethasone was injected sublingually after the onset of local anesthesia, and 1 h prior to surgery, as the onset time of dexamethasone is 1 h. Such dexamethasone injection before the first incision appears to have benefits; for example, significantly less pain and decreased rescue analgesic drug intake. These are likely due to the biological life and peak level time of dexamethasone. Joshi et al. [34] and Hupp et al. [35] showed that corticosteroids must be administered before the tissue is damaged, not during or after surgery [7232425]. Using these drugs, peak levels of bradykinin release occur within 3 h of tissue trauma.
In the present study, we injected the dexamethasone sublingually, because we believed that this is more comfortable for the patient then intramuscular, intravenous, or deep intra-potential injection. The sublingual space is considered a potential superficial site for drug administration. Sublingual injection ensures systemic administration; the space has high permeability and a rich blood supply. Furthermore, the sublingual route can induce rapid onset of the effects of dexamethasone. Sublingual injection of dexamethasone (8 mg) is believed to be a more effective method of drug administration than the buccal mucosa and intramuscular routes.
In conclusion, 8 mg of dexamethasone, pre-operatively injected into the sublingual space, can reduce postoperative pain after mandibular third molar extraction. The sublingual space is well supplied with vascular and lymphatic drainage, and first pass metabolism in the liver is avoided using this route, as is pre-elimination in the gastrointestinal tract. In the present study, pre-operative dexamethasone injection into the sublingual space resulted in significant different VAS pain scores and analgesic intake. We recommend sublingual injection of dexamethasone (8 mg) to ameliorate postoperative pain.
Figures and Tables
Table 1
Sex and duration of surgery
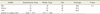
| Variable | Dexamethasone Group | Placebo Group | Total | Percentage | P-value |
|---|---|---|---|---|---|
| Men | 19 | 19 | 38 | 39.6 | 0.3 |
| Women | 29 | 29 | 58 | 60.4 | |
| Total | 48 | 48 | 96 | 100.0 | |
| Duration of surgery (min) | 20.06 ± 6.61 | 19.47 ± 6.99 |
Table 2
Angulation of mandibular third molar
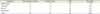
| Angulations | Dexamethasone Group | Placebo Group | Total | Percentage |
|---|---|---|---|---|
| Mesioangular | 18 | 18 | 36 | 37.5 |
| Horizontal | 16 | 16 | 32 | 33.4 |
| Vertical | 9 | 9 | 18 | 18.7 |
| Distoangular | 5 | 5 | 10 | 10.4 |
| Total | 48 | 48 | 96 | 100.0 |
ACKNOWLEDGEMENTS
The authors would like to thank the staff and dental assistants, including our colleagues in the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University.
Notes
References
1. Boonsiriseth K, Klongnoi B, Sirintawat N, Saengsirinavin C, Wongsirichat N. Comparative study of the effect of dexamethasone injection and consumption in lower third molar surgery. Int J Oral Maxillofac Surg. 2012; 41:244–247.

2. Kitade T, Ohyabu H. Analgesic effects of acupuncture on pain after mandibular wisdom tooth extraction. Acupunct Electrother Res. 2000; 25:109–115.

3. Gozali P, Kiattavornchareon S, Wu M, Wonsirichat N, Suphangul S. Bethamethasone and methylprednisolone usage in lower third molar surgery: Review literature. M Dent J. 2015; 35:273–280.
4. Latt MM, Kiattavornchareon S, Boonsiriseth K, Pairuchvej V, Wongsirichat N. The efficacy of dexamethasone injection on postoperative pain in lower third molar surgery. J Dent Anesth Pain Med. 2016; 16:95–102.

5. Bjornsson GA, Haanes HR, Skoglund L. A randomized, double blind crossover trial of paracetamol 1000 mg four times daily vs ibuprofen 600 mg: effect on swelling and other postoperative events after third molar surgery. Br J Clin Pharmacol. 2003; 55:405–412.
6. Michalek-Sauberer A, Heinzl H, Sator-Katzenchlager SM, Monov G, Knolle E, Kress HG. Perioperative auricular electroacupuncture has no effect on pain and analgesic consumption after third molar tooth extraction. Anesth Analg. 2007; 104:542–547.

7. Gersema L, Baker K. Use of corticosteroids in oral surgery. J Oral Maxillofac Surg. 1992; 50:270–277.

8. Hebel SK. Drug facts and comparisons. St. Louis: Facts and Comparisons;1999. p. 122.
9. Beirne OR, Hollander B. The effect of methylprednisolone on pain, trismus, and swelling after removal third molars. Oral Surg Oral Med Oral Pathol. 1986; 61:134–138.

10. Messer EJ, Keller JJ. The use of intraoral dexamethasone after extraction of mandibular third molars. Oral Surg Oral Med Oral Pathol. 1975; 40:594–598.

11. Hargreaves KM, Shmidt EA, Mueller GP, Dionne RA. Dexamethasone alters plasma levels of beta-endorphin and postoperative pain. Clin Pharmacol Ther. 1987; 42:601–607.

12. Mirzai H, Tekin I, Alincak H. Perioperative use of corticosteroid and bupivacaine combination in lumbar disc surgery: a randomized controlled trial. Spine. 2002; 27:343–346.

13. Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006; 102:263–267.

14. Pell GJ, Gregory BT. Impacted mandibular third molars: classification and modified techniques for removal. Dent Digest. 1933; 39:330–338.
15. Laureano Filho JR, Maurette PE, Allais M, Cotinho M, Fernandes C. Clinical comparative study of the effectiveness of two dosages of dexamethasone to control postoperative swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Patol Oral Cir Bucal. 2008; 13:E129–E132.
16. Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Beretta M, Farronato D, et al. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: a prospective study. J Oral Maxillofac Surg. 2007; 65:2218–2226.

17. Graziani F, D'Aiuto F, Arduino PG, Tonelli M, Gabriele M. Perioperative dexamethasone reduces post-surgical sequelae of wisdom tooth removal. A split-mouth randomized double-masked clinical trial. Int J Oral Maxillofac Surg. 2006; 35:241–246.

18. Ustun Y, Erdogan O, Esen E, Karsli ED. Comparison of the effects of 2 doses of methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:535–539.

19. Landucci A, Wosny AC, Uetanabaro LC, Moro A, Araujo MR. Efficacy of a single dose of lowlevel laser therapy in reducing pain, swelling, and trismus following third molar extraction surgery. Int J Oral Maxillofac Surg. 2016; 45:392–398.

20. Costa FWG, Soares ECS, Esses DFS, Silva PG, Bezerra TP, Scarparo HC, et al. A split-mouth, randomized, triple-blind, placebo-controlled study to analyze the pre-emptive effect of etoricoxib 120 mg on inflammatory events following removal of unerupted mandibular third molars. Int J Oral Maxillofac Surg. 2015; 44:1166–1174.

21. Al-Sukhun J, Al-Sukhun S, Penttilä H, Ashammakhi N, Al-Sukhun R. Pre-emptive analgesic effect of low doses of celecoxib is superior to low doses of traditional nonsteroidal anti-inflammatory drugs. J Craniofac Surg. 2012; 23:526–529.

22. Sisk AL, Grover BJ. A comparison of pre-operative and postoperative naproxen sodium for suppression of postoperative pain. J Oral Maxillofac Surg. 1990; 48:674–678.

23. Morse Z, Tump A, Kevelham E. Ibuprofen as a pre-emptive analgesic is as effective as rofecoxibfor mandibular third molar surgery. Odontology. 2006; 94:59–63.

24. Saito K, Kaneko A, Machii K, Ohta H, Ohkura M, Suzuki M. Efficacy and safety of additional 200-mg dose of celecoxib in adult patients with postoperative pain following extraction of impacted third mandibular molar: a multicenter, randomized, double-blind, placebo controlled, phase II study in Japan. Clin Ther. 2012; 34:314–328.

25. Lustenberger FD, Gratz KW, Mutzbauer TS. Efficacy of ibuprofen versus lornoxicam after third molar surgery: a randomized, double-blind, crossover pilot study. Oral Maxillofac Surg. 2011; 15:57–62.

26. Pozos-Guillen A, Martinez-Rider R, Aguirre-Banuelos P, Perez-Urizar J. Pre-emptive analgesic effect of tramadol after mandibular third molar extraction: a pilot study. J Oral Maxillofac Surg. 2007; 65:1315–1320.

27. Zandi M, Amini P, Keshavarz A. Effectiveness of cold therapy in reducing pain, trismus, and oedema after impacted mandibular third molar surgery: a randomized, self-controlled, observer-blind, split-mouth clinical trial. Int J Oral Maxillofac Surg. 2016; 45:118–123.

28. Patten JR, Patten J, Hutchins MO. Adjunct use of dexamethasone in postoperative dental pain control. Compendium. 1992; 13:580. 582. 584 passim.
29. Tavares MG, Machado AP, Motta BG, Borsatto MC, Rosa AL, Xavier SP. Electro-acupuncture efficacy on pain control after mandibular third molar surgery. Braz Dent J. 2007; 18:158–162.

30. Chukwuneke FN, Oji C, Saheeb DB. A comparative study of the effect of using a rubber drain on postoperative discomfort following lower third molar surgery. Int J Oral Maxillofac Surg. 2008; 37:341–344.

31. Osunde OD, Adebola RA, Saheeb DB. A comparative study of the effect of suture-less and multiple suture techniques on inflammatory complications following third molar surgery. Int J Oral Maxillofac Surg. 2012; 41:1275–1279.

33. Mojsa IM, Pokrowiecki R, Lipczynski K, Czerwonka D, Szczeklik K, Zaleska M. Effect of submucosal dexamethasone injection on postoperative pain, oedema, and trismus following mandibular third molar surgery: a prospective, randomized, double-blind clinical trial. Int J Oral Maxillofac Surg. 2017; 46:524–530.

34. Neupert EA III, Lee JW, Philput CB, Gordon JR. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992; 50:1177–1182.

35. Hupp JR. Principles of surgery. In : Peterson LJ, Ellis E, Hupp JR, Tucker MR, editors. Contemporary oral and maxillofacial surgery. 3rd ed. St. Louis: Mosby;1998. p. 56.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download