Abstract
Background
This study is aimed to evaluate the level of fear and to reduce the overall fear, thereby enabling patients to receive treatment via timely visits.
Methods
In a survey conducted by 460 South Korean middle school students, we used 453 data that faithfully responded to the survey. Multiple regression analysis was conducted to investigate the factors influencing subjective oral health and dental fear. The significance level used for statistical significance was α = 0.05.
Results
The level of fear was higher for upper grade, female students. The factors affecting dental fear were higher for gingival bleeding and dental pain. Regarding factors for dental fear affecting subjective oral health, lower fear of puncture needle and tooth removal tool resulted in higher subjective oral health.
Conclusion
The study found that adolescents had higher fear of dental care when they had gingival bleeding and tooth pain. Gingival bleeding is a symptom of early gingival disease and dental pain is likely due to advanced dental caries. These results suggested that it is necessary to have a program to reduce dental fear and anxiety as well as a program to prevent dental diseases through regular periodic screening and education.
Recently, the Federation Dentaire Internationale (FDI) introduced a new definition for oral health: the ability to speak, smile, taste, chew and swallow without any diseases of the craniofacial complex, pain or discomfort, thus including both physical and mental well-being [12]. Although much progress has been made in maintaining dental health, nearly all adolescents undergo various forms of dental treatment from their childhood. Despite the breakthrough of dento-medical devices and treatment-related technologies, there is still a fear of dento-medical treatment among patients. Dental treatment differs from other treatments as it takes long time to treat the disease. Moreover, the visits are more frequent. In many cases, except for preventive care, pain is often accompanied by a tendency to fear dental treatment.
There are many definitions of dental fear; generally, it is defined as a response to dental treatment-related stimulation, and it varies in the degree of anxiety or fear that the patient feels subjectively [3]. Moore et al. reported that the causes of dental fear are dental experiences that cause mental trauma, leading to secondary problems associated with social learning, and psychological problems associated with feelings of helplessness and not being in control [4]. Toothache owing to dental caries is common in teenagers. Dental pain is a major cause of fear. Fear in turn increases the pain and leads to postponement or avoidance of dental care [5]. Fear of dental treatment has long been studied; however, only in the late 1960s, Corah began to systematize, starting with the development of the Dental Anxiety Scale (DAS) [6]. Molin and Seeman conducted a study to measure dental fear [7]. Lautch investigated whether the fear of dental treatment was due to the personality and characteristics of the patient [8]. Gale evaluates the fear of dentistry and stated that under certain circumstances, the patient should be aware of the situation rather than the actual pain [9]. The Dental Fear Survey (DFS), developed by Kleinknecht et al. was composed of various items related to dental fear, and it was designed to specifically and clearly measure the dental treatment, physiological response, and dental treatment stimulation [10]. The relationship between dental pain and dental fear was studied using Japanese DFS scale in 1988 [11]. The Korean version of the Dental Fear Scale (K-DFS) was translated and evaluated by Kim et al [12131415]. According to Shim et al [16], the dental fear anxiety scale, a tool used to measure dental fear, was used to distinguish dental fear as dental associative fear and dental fear secondary to age and indirect pain [17]. Subjective oral health status is easier to use in dental health care than the traditional indicators of objective oral health status [18]. Studies have shown that oral symptoms affect oral function, which again determines subjective oral health status and affects the quality of life. In other studies conducted in Korea, the objective and subjective oral health statuses have been reported to be highly relevant [19]. It has been reported that the subjective perception of an individual has a greater effect on the self [20].
In the case of adolescents with a high fear of dental treatment, even if they are aware of the symptoms, their oral health statuses may deteriorate because they are reluctant to visit dental clinics. Therefore, to address this, this study aimed to evaluate the feeling of fear more than any other symptom and reduce the overall fear, thereby enabling patients to receive treatment via timely visits.
As the study subjects, Korean students (first to third grades in a junior middle school in Sanbon-City, Gyeonggi-Do) were selected using the convenience sampling method. This study was approved by the institutional review board in accordance with the policy on research with human participants (Wonkwang University Daejeon Dental Hospital IRB NO. W1411/002-001). Regarding the questionnaire survey, we conducted a pre - consultation for the researchers and the self - entry method was used. The questionnaires were administered directly in the field and valid responses were obtained from 460 of 475 patients. Of these, 453 patients were considered after excluding those who responded inappropriately. The survey items considered in this study were demographic characteristics, subjective oral health status, and dental fear. The demographic characteristics were composed of two items: the sex and middle school grade of the adolescent. Subjective oral health status consisted of a total of five items, including gingival bleeding, dental pain, bad breath, retained food and dry mouth. The subscales of the subjective oral health status included 5 points on the Likert scale and 5 points on the scale of “very” and “not very”, however, there were few responses of “very” and “not very”. Moreover, the interpretation of these responses was considered inconsistent. Statistical analysis was performed by converting the grades into 3 points of “yes”, “normal” and “not”. Dental phobia was measured using the Korean version of the Dental Fear Scale (K-DFS) developed by Kleinknecht and others in 2015 by translating the dental fear survey scale. A total of 20 items were categorized. The item-by-item scales were 5 points on the Likert scale: very unlikely, 1 point; almost not so, 2 points; normal, 3 points; genenally yes, 4point; very yes, 5 points. The collected data were analyzed using the SPSS 19.0 software (SPSS Inc. Chicago, IL, USA). The frequency and percentage of the population sociological characteristics and the subjective oral health status were calculated, and the average of the dental fear items was obtained. The reliability was analyzed to confirm the internal consistency of dental fear-inducing variables. The overall Cronbach's α coefficient was 0.953. In addition, multiple regression analysis was performed to investigate the factors influencing subjective oral health and dental fear. The significance level used for statistical significance was α = 0.05.
The demographic characteristics of the subjects are shown in Table 1. Regarding the sex, 231 (51.0%) were female students and 222 (49.0%) male students. Depending on the middle school grade, 154 students (34.0%) were from the third grade, 151 (33.3%) from the second grade, and 148 (32.7%) from the first grade. There were 101 cases (22.3%) of gingival bleeding and 38 cases (8.4%) of tooth pain. There were 83 cases (18.3%) with bad breath, 28 (6.2%) with food stress, and 80 (17.7%) with symptoms of dry mouth.
Table 2 shows the mean scores of the subjects' dental fear per item. The dental fear of the subject was 2.69 points in the item of “fear of seeing tooth removal equipment.” In the dental fear, male students had the highest score (2.30) for both the “fear of the needle puncture” and “fear of tooth clearing.” In the case of female students, “fear of seeing tooth removal equipment” was the highest with 3.11 points. Overall, dental fear was higher for girls(female students; 2.33) than for boys(male students; 1.85).
Table 3 shows the results of multiple regression analysis of the factors affecting dental fear. The explanatory power of the variables was 52.6%, and gingival hemorrhage and dental pain were found to have a significant effect on the total dental fear. In other words, the more the gingival hemorrhage and tooth pain, the higher was the total dental fear.
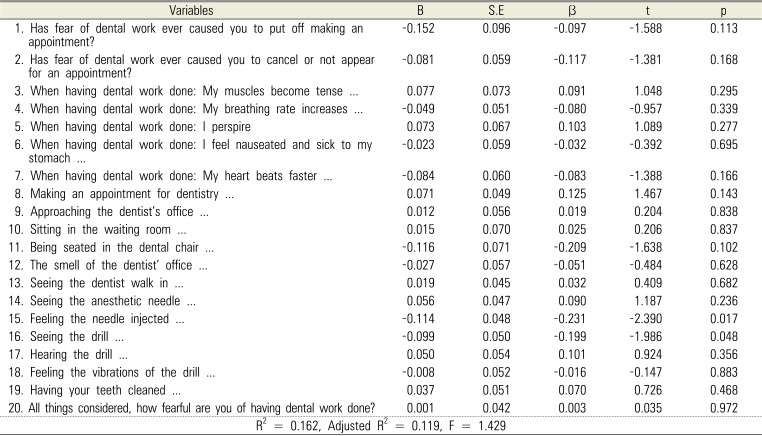
The results of multiple regression analysis of the factors of dental fear in subjective oral health are shown in Table 4. The descriptive power of the variables was 11.9%. The lower the fear of the puncture needle, the lower was the fear of the tooth removal tool, and the higher was the subjective oral health.
Nearly 70 years ago, the WHO (1948) defined health as “a state of complete physical, mental, and social well-being, and not merely the absence of disease or infirmity.” The editorial by Glick and colleagues summarizes the new FDI definition of oral health: oral health is multi-faceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow, and convey a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex. Further attributes indicate that it is a fundamental component of health and physical and mental well-being [21]. Willits and Crider found that a subjective assessment of health could be a more accurate predictor of the quality of life than a clinical assessment of the clinical illness [22]. Moore et al. [23] compared the overall fear and demographic factors with the degree of dental fear. Holtzman et al. reported that patients who were afraid of dental treatment were three times more likely to break treatment commitments than patients who were not. Fear and anxiety decreased as age increased; muscle relaxation was a significant response symptom when sitting in a dental chair. Moreover, one study reported that women showed more fear on stimulation during dental treatment than men [24]. Landgren et al. studied the psychophysical aspects of dental fear [25]. The cause and extent of dental fear for various age groups have been extensively studied; a total of 5-22% adults and 13% elderly people cancel appointments or postpone visits [262728]. This indicates that dental care is a subject of horror at all ages, from children to the elderly individuals. These dental fears are caused by fear of odor, noise, and instrument sounds. In the clinical setting, treatment activities, such as tooth removal, extraction, and periodontal treatment, are accompanied by local anesthesia. In particular, teenagers are known to have a high fear of dental treatment because they are psychologically and physically immature [2930]. The higher grade and female students were the higher the rate of experience of fear. Further, the level of dental fear was higher in female subjects. In the sub-domain, the maximum fear was associated with “fear of seeing the tooth removal tool” in female patients and the “fear of needle piercing” and “fear of the tooth removal tool” in male subjects. The level of dental fear according to the subjective oral health factors showed that a higher level of dental fear was associated with greater gingival bleeding and dental pain. Conversely, the factors of dental fear affecting subjective oral health were less fear of needle puncture and less fear of the tooth removal tool; these were indicative of better subjective oral health. This study on Korean youths found that adolescents had more fear of dental care when they had gingival bleeding and tooth pain. Gingival bleeding is a symptom of early gingival disease, and dental pain is likely to be due to advanced dental caries. According to Kim et al., higher dental fear was associated with cases of bad breath, dental caries, loss of teeth, and dental pain [31]. In a study by Choi and Kim, dental fear was higher for cases with bad breath and gum disease, which was consistent with the reported association between self-perceived oral disease symptoms and fear of dental treatment [32]. If the dental disease progresses to a degree that is not healthy due to the oral symptoms, there is a higher likelihood of pain during treatment. If the level of dental fear is high, the vicious cycle of avoiding dental clinic visits and treatment is inevitable. Therefore, according to the results of this study, in adolescents with a high dental fear, it is necessary to have a program to reduce the dental fear and anxiety as well as a program to prevent dental diseases through regular screening and education.
References
1. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. J Am Dent Assoc. 2016; 147:915–917. PMID: 27886668.

2. Diener E, Scollon CN, Lucas RE. The evolving concept of subjective wellbeing: the multifaceted nature of happiness. In : Diener E, editor. Assessing wellbeing: the collected works of Ed Diener. New York: Springer;2009. p. 67–100.
3. Klages U, Kianifard S, Ulusoy O, Wehrbein H. Anxiety sensitivity as predictor of pain in patients undergoing restorative dental procedures. Community Dent Oral Epidemiol. 2006; 34:139–145. PMID: 16515678.

4. Moore R, Brødsgaard I, Rosenberg N. The contribution of embarrassment to phobic dental anxiety: a qualitative research study. BMC Psychiatry. 2004; 19:4–10.

5. Sullivan MJ, Neish NR. Catastrophizing, anxiety and pain during dental hygiene treatment. Community Dent Oral Epidemiol. 1998; 26:344–349. PMID: 9792127.

7. Molin C, Seeman K. Disproportionate dental a and anxiety. Clinical and nosological considerations. Acta Odontol Scand. 1970; 28:197–212. PMID: 5268145.
10. Kleinknecht RA, Thorndike RM, McGlynn FD, Harkavy J. Factor analysis of the dental fear survey with crossalidation. J Am Dent Assoc. 1984; 108:59–61. PMID: 6582116.
11. Domoto PK, Weinstein P, Melnick S, Ohmura M, Uchida H, Ohmachi K, et al. Results of a dental fear survey in japan: impli-cations for dental public health in Asia. Community Dent Oral Epidemiol. 1988; 16:199–201. PMID: 3165743.

12. Shim YS, Kim AH, An SY. Dental fear and anxiety of juveniles in some areas of Gyeonggi province. J Korean Acad Pediatr Dent. 2011; 38:362–367.

13. Choi JE, Yang HJ, An SY. Dental fear and anxiety of middle school students in D middle school in Gyeonggi-Do, 2012. J Korean Dent Assoc. 2013; 51:405–413.
14. Shim YS, Kim AH, An SY. Dental Fear and the associated Factors of some Middle School Students in Cheongju-City. J Korea Contents Assoc. 2013; 13:295–304.

15. Kim AH, Shim YS, Park SO, Kim HW, An SY. Reliability and validity of the Korean version of the Dental Fear Survey. J Dent Anesth Pain Med. 2015; 15:85–92. PMID: 28879263.

16. Shim YS, Park SO, An SY. The Survey of Fear Associated with Dental Treatment in Some Middle School Students in Cheongju. Korean J Health Serv Manag. 2014; 8:165–173.

17. Matthias RE, Atchison KA, Lubben JE, De Jong F, Schweitzer SO. Factors affecting self-ratings of oral health. J Public Health Dent. 1995; 55:197–204. PMID: 8551458.

18. Wilson IR, Cleary PD. Linking clinical variables with health related quality of life; a conceptual model of patient outcomes. J Am Med Assoc. 1995; 273:59–65.
19. Lee SM, Kim SK, Kang BW. Adults concern for oral health and subjective oral health symptoms. J Korean Soc Dent Hyg. 2011; 11:871–880.
20. Reisine ST, Bailit HI. Clinical oral health status and adult perceptions of oral health. Soc Sci Med Med Psychol Med Sociol. 1980; 14A:597–605. PMID: 7209633.

21. Lee JY, Watt RG, Williams DM, Giannobile WV. A New Definition for Oral Health: Implications for Clinical Practice, Policy, and Research. J Dent Res. 2017; 96:125–127. PMID: 27879422.

22. Willits FK, Crider DM. Health rating and life satisfaction in later middle years. J Gerontol. 1988; 43:S172–S176. PMID: 3418042.
23. Moore R, Birn H, Kirkegaard E, Brødsgaard I, Scheutz F. Prevalence and characteristics of dental anxiety in Danish adults. Community Dent Oral Epidemiol. 1993; 21:292–296. PMID: 8222604.

24. Holtzman JM, Berg RG, Mann J, Berkey DB. The relationship of age and gender to fear and anxiety in response to dental care. Spec Care Dentist. 1997; 17:82–87. PMID: 9582708.

25. Lundgern J, Berggren U, Carlsson SG. Psychophysiological reactional phobic patients during video stimulation. Eur J Oral Sci. 2001; 109:172–177. PMID: 11456347.
26. Skaret E, Raadal M, Berg E, Kvale G. Dental anxiety and dental avoidance among 12 to 18 year olds in Norway. Eur J Oral Sci. 1999; 107:422–428. PMID: 10625100.

27. Bedi R, MeGrath C. Factors associated with dental anxiety among older people in Britain. Gerodontology. 2000; 17:97–103. PMID: 11813685.

28. Kvalge G, Berg E, Nilsen CM, Raadal M, Nielsen GH, Johansen TB, et al. Validation of the dental fear scale and the dental be life survey in a Norwegian sample. Community Dent Oral Epidemiol. 1997; 25:160–164. PMID: 9181291.
29. Moon SJ, Park JH, Choi YC, Choi SC. The study of changes in oral health care of preschoolers in taebaek city through oral hygiene education. J Korean Acad Pediatr Dent. 2009; 36:71–77.
30. Park SY, Won YS. Influences of previous pain experiences during dental treatment on dental fear. Korean J Health Serv Manag. 2012; 6:141–151.

31. Kim SK, Kim MH, Choi HJ, Hwang JG. Related factors to dental fear in some adults. J Korean Soc Dent Hyg. 2014; 14:881–886.

32. Choi MH, Kim NS. The effect of factors dental treatment fear of dental hygiene and non-dental hygiene students. J Korean Soc Dent Hyg. 2011; 11:523–532.
Table 1
General characteristics of the subjects
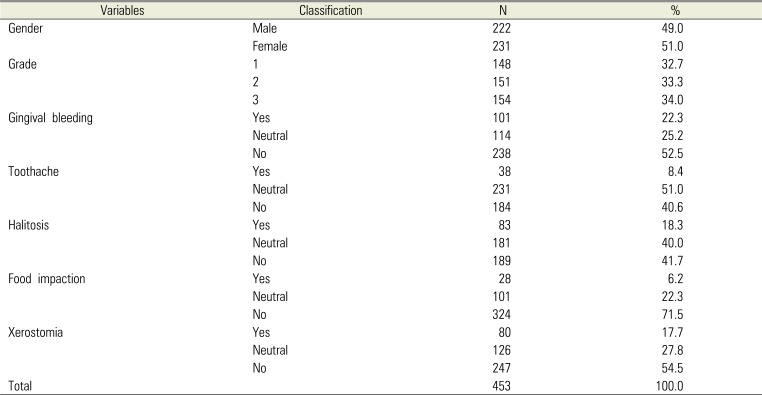
Table 2
Average score for each item of dental fear,factors affecting dental fear
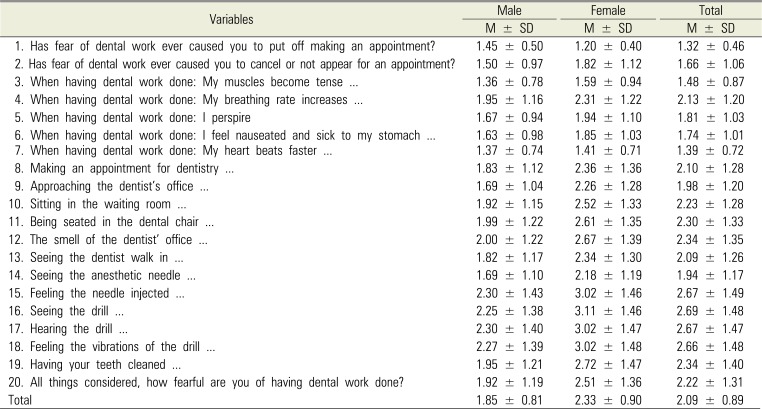
Table 3
Factors affecting dental fear
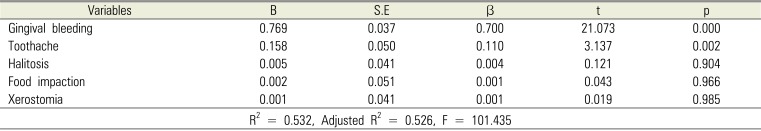
Table 4
Factors affecting subjective oral health




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download