Abstract
In cases of multiple facial trauma and other specific cases, the anesthesiologist may be asked to convert an oral endotracheal tube to a nasal endotracheal tube or vice versa. Conventionally, the patient is simply extubated and the endotracheal tube is re-inserted along either the oral or nasal route. However, the task of airway management can become difficult due to surgical trauma or worsening of the airway condition. Fiberoptic bronchoscopy was considered a novel method of airway conversion but this method is not useful when there are secretions and bleeding in the airway, or if the anesthesiologist is inexperienced in using this device. We report a successful airway conversion under the aid of both, a fiberoptic bronchoscope and a C-MAC video laryngoscope.
Go to : 
In cases of multiple facial trauma and other specific cases, an anesthesiologist may be asked to convert an oral endotracheal tube to a nasal endotracheal tube or vice versa. Conventionally, the patient is simply extubated and the endotracheal tube is re-inserted along either the oral or nasal route. However, this can be a challenge to an anesthesiologist if there is bleeding and/or edema due to previous surgery or nasal trauma, or during nasal endotracheal tube insertion. Edema due to prior surgery can cause anatomical changes in the airway, too. To address these situations, various methods have been reported including tube exchangers, fiberoptic bronchoscopes (FOB), nasogastric tubes and other methods [123456]. Each method has its own advantages and disadvantages. Here we have reported two cases of tube exchange with the aid of FOB and a C-MAC video laryngoscope with consent from the patients for publication of their cases.
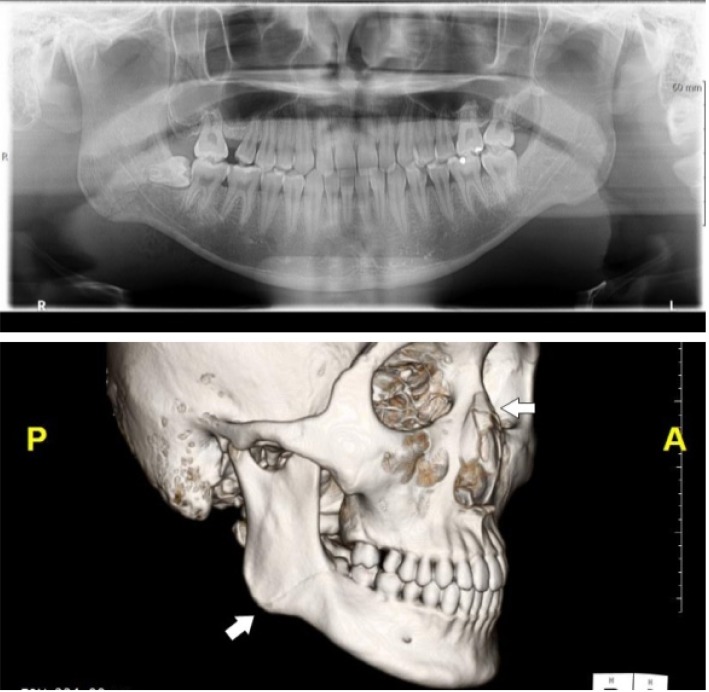
A 21-year-old man (ASA class I, weight 67 kg, height 171 cm) with a nasal bone and mandible fracture was scheduled for closed reduction of the nasal bone and open reduction with internal fixation of the right mandibular angle (Fig. 1). His past medical history was unremarkable; he had no history of previous surgeries. Preoperative evaluation including laboratory tests, electrocardiography, and chest radiography was normal. There were no specific findings upon airway examination, including mouth opening, thyromental distance, and Mallampati classification (grade II).
We discussed the anesthetic plan with the surgeon who suggested nasal intubation with an endotracheal tube (ETT) while performing the mandible surgery and oral intubation while performing the nasal bone surgery.
General anesthesia was induced using intravenous injection of 60 mg lidocaine, 100 µg fentanyl, 120 mg propofol, and 50 mg rocuronium, with standard monitoring and preoxygention. After the induction of anesthesia, 3 cotton swabs with water soluble jelly mixed with a 0.01% epinephrine solution were inserted into the right nostril. After mask ventilation for 3 minutes with 100% oxygen and 4 vol% sevoflurane, we removed the cotton swabs and inserted a lubricated 6.5-mm Polar™ Preformed Tracheal Tube (Smith Medical, Keene, NH, USA) under the guidance of an FOB (3.8 mm, Pentax, Japan). General anesthesia was maintained using 1.5-3 vol% sevoflurane; open reduction and internal fixation of the mandible was performed successfully; within an operating time of 1 hour and 45 minutes. We then tried to use an FOB to intubate the patient orally, but bleeding and secretions blocked the view of the FOB despite repeated suctioning. Subsequently, used a C-MAC® video laryngoscope (Karl Storz Endoscopy-America, CA, USA) to guide the route of FOB. The C-MAC® video laryngoscope showed a clear view of the glottis while the view of the FOB was blurred with secretion and blood. Using the C-MAC® video laryngoscope we successfully guided and inserted the FOB into the trachea without manipulating the nasal ETT (Video 1, 2). After confirmation of the tracheal ring on the FOB view, we removed the nasal ETT and followed with the railroading of an oral ETT via the FOB (Video 1). After confirming the EtCO2 curve, mechanical ventilation was resumed. Closed reduction of the nasal bone was performed after the nasal to oral endotracheal tube exchange. Upon completion of the procedures, any residual muscle relaxation was reversed with atropine and neostigmine. The patient was successfully recovered without complications and was extubated. The postoperative period was uneventful.
Go to : 
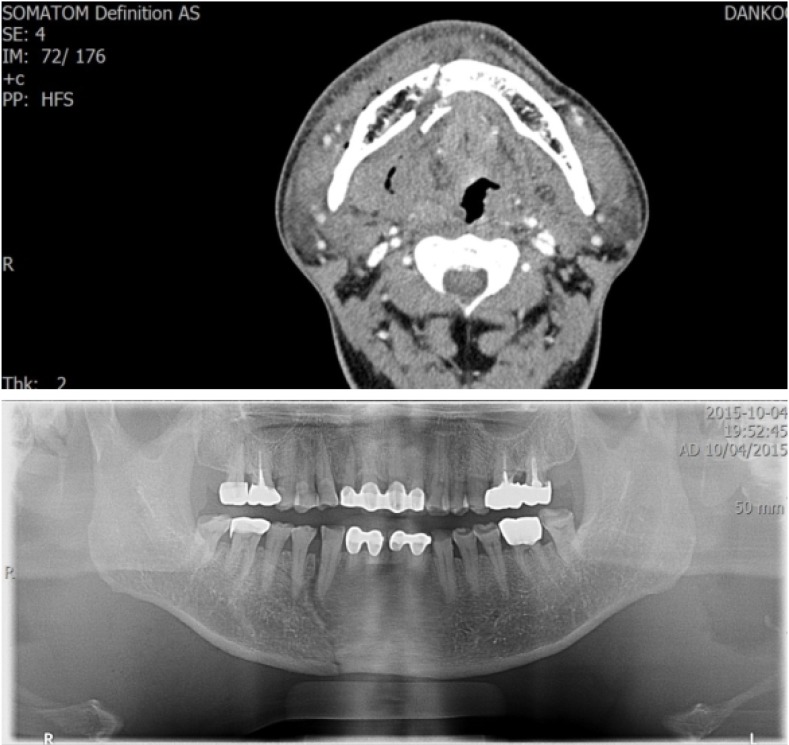
A 69-year-old man (ASA class II, weight 79 kg, height 168 cm) with a fracture of the right side mandibular angle was scheduled for emergency open reduction with internal fixation (Fig. 2). The patient had a history of diabetes and hypertension and was on medications. The patient had no history of prior surgery. Preoperative evaluations including laboratory tests, electrocardiography, and chest radiography was normal. The patient was transferred to the operating room with endotracheal intubation because of an unstable airway caused by sublingual and submandibular swelling. The surgeon, however, opted for nasal intubation of the ETT during the mandibular surgery.
General anesthesia was induced with sevoflurane and intravenous injection of 60 mg rocuronium, with a standard monitoring. After the induction of anesthesia, we tried direct laryngoscopy with a conventional Macintosh blade and FOB to change the tube but failed because of massive airway edema and bleeding. The tube exchange procedure was then postponed and the surgical procedure was performed under oral intubation. The open reduction and internal fixation of the mandible was performed successfully within an operating time of 2 hours and 15 minutes. The surgeon again opted for a change to nasal intubation for arch bar wiring. An attempt to intubate the patient via the nasal route using FOB, was made. We inserted a 6.5-mm Polar™ Preformed Tracheal Tube via left nostril and tried to intubate the trachea under the guidance of the FOB. However, bleeding and secretions blocked the FOB view despite repeated suctioning as in the first trial. Next, we attempted to use a C-MAC® video laryngoscope which showed a clear view of the glottis; the FOB view was blurred with secretions and blood. Using a C-MAC® video laryngoscope we guided the FOB into the trachea. After confirmation of the tracheal ring on the FOB view, we removed the oral ETT and followed with the railroading of the nasal ETT via the FOB. After confirming the EtCO2 curve, mechanical ventilation was resumed. After the arch bar wiring of the maxilla and mandible, the patient was transferred to the intensive care unit. The postoperative period was uneventful.
Go to : 
Tube exchange between the nasal– oral route has two potential risks: first, the cessation of ventilation during the procedure and second, the accidental loss of airway or airway conduit. There were several important observations, with this respect to this, in these two cases.
First, the use of an FOB, though a novel method of difficult airway management, has difficulty overcoming airway bleeding or secretions. Moreover, a large tongue can block the route of the FOB [2]. These problems can be resolved using a C-MAC video laryngoscope. A video laryngoscope can shows a much better view of the oral cavity than that shown by an FOB, in the presence of secretion and bleeding. Furthermore, a video laryngoscope offers a good view of the FOB route. In our cases, we were able to see the FOB route using only the video laryngoscope view. Sharma et al reported that they used an FOB as a ‘stylet’ [6]. However, an FOB view is important to gauge the depth of the tip and to decrease accidental dislodgement of the FOB from the trachea.
Second, using FOB as an intubation conduit or ‘flexible stylet’ under the guidance of a video laryngoscope can induce less airway trauma and provide for better outcomes. Sharma et al reported that they used a Glidescope® video laryngoscope in a patient who had Cowden syndrome. They had tried to intubate the patient with an endotracheal tube loaded on the Glidescope® rigid stylet [6]. Despite satisfactory visualization of vocal cord, it was difficult to direct the tube toward the vocal cord and the procedure induced bleeding in the airway. They then used an FOB instead of the rigid stylet and were able to gently insert the FOB into the vocal cord, successfully intubating the patient [6]. Video laryngoscopes have their specific curvature and they can show a good view of glottis even in difficult airways, but despite the use of a stylet, directing the ETT to the vocal cords can be difficult and can induce injury to airway structures [6789].
Third, the method we used to exchange the tube position using both a C-MAC video laryngoscope and a FOB can minimize non-ventilation time results by decreasing the risk of desaturation. And the risk of dislodgement of the intubation conduit or loss of airway is very low. In our case, it took only 14 seconds from extubation to re-intubation. Thus, using a FOB with a video laryngoscope can be a good technique for tube exchange and difficult airway management. We did not use a nasogastric tube or tube exchange catheter, which, when inserted blindly can cause airway trauma. Also, this method can be used in case of oral to oral tube exchange when difficult airway management is expected.
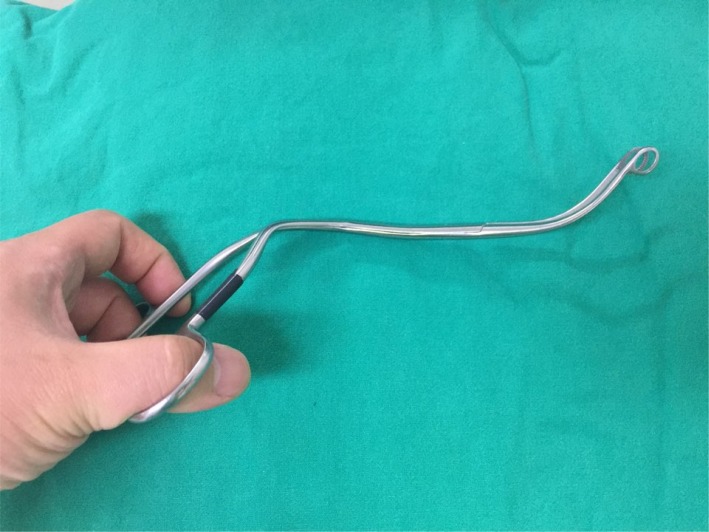
The problem related to the difficulty in passing the ETT threaded on the FOB has been previously described. To overcome this problem many techniques and tube designs have been invented [6]. However, with the aid of video laryngoscopy view we can see the FOB route and the ETT which can be manipulated using a curved Magil forcep (Fig. 3).
In conclusion, we described two cases of successful tube exchange procedures both a FOB and a C-MAC video laryngoscope in patients with facial bone fractures. We recommend this method for difficult airway management especially when FOB use alone may be difficult.
Go to : 
ACKNOWLEDGEMENTS
This article was financially supported by Dankook University, Cheonan, South Korea.
Go to : 
References
1. Nakata Y, Niimi Y. Oral-to-nasal endotracheal tube exchange in patients with bleeding esophageal varices. Anesthesiology. 1995; 83:1380–1381. PMID: 8533944.

2. Dutta A, Chari P, Mohan RA, Manhas Y. Oral to nasal endotracheal tube exchange in a difficult airway: a novel method. Anesthesiology. 2002; 97:1324–1325. PMID: 12411827.

3. Hoffman J, Matthews JM, Reese AR. Oral endotracheal tube exchange to the nasal route in a patient with facial trauma. J Clin Anesth. 2011; 23:342. PMID: 21524900.

4. Muldowney BL, Eastburn EC, Nargozian CD. Oral to nasal endotracheal tube exchange using an airway exchange catheter in a neonate with Pierre Robin Sequence. J Clin Anesth. 2015; 27:80–81. PMID: 25468589.

5. Lee SH, Kim JE, Kang JM. Alternative technique for changing from nasal to oral endotracheal tube for orthognathic and nasal surgery by using an airway exchange catheter: a case report. Korean J Anesthesiol. 2014; 67:48–51. PMID: 25097739.

6. Sharma D, Kim LJ, Ghodke B. Successful airway management with combined use of Glidescope videolaryngoscope and fiberoptic bronchoscope in a patient with Cowden syndrome. Anesthesiology. 2010; 113:253–255. PMID: 20526181.

7. Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007; 54:54–57. PMID: 17197469.

8. Hsu WT, Tsao SL, Chen KY, Chou WK. Penetrating injury of the palatoglossal arch associated with use of the GlideScope videolaryngoscope in a flame burn patient. Acta Anaesthesiol Taiwan. 2008; 46:39–41. PMID: 18390400.

9. Pham Q, Lentner M, Hu A. Soft Palate Injuries During Orotracheal Intubation With the Videolaryngoscope. Ann Otol Rhinol Laryngol. 2017; 126:132–137. PMID: 27831515.

Go to : 
Supplementary Materials
Video 1
The view of the tube exchange procedure of the first case. Note that we could not see a clear view on the FOB screen until we entered the trachea, but we could guide the FOB under the view of the C-MAC video laryngoscope (https://jdapm.org/src/sm/jdapm-17-219-s001.avi).
Video 2
The view of the C-MAC video laryngoscopy during the tube exchange procedure (https://jdapm.org/src/sm/jdapm-17-219-s002.mp4).




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download