This article has been
cited by other articles in ScienceCentral.
Abstract
Cerebral palsy is a non-progressive disorder resulting from central nervous system damage caused by multiple factors. Almost all cerebral palsy patients have a movement disorder that makes dental treatment difficult. Oral hygiene management is difficult and the risks for periodontitis, dental caries and loss of multiple teeth are high. Placement of dental implants for multiple missing teeth in cerebral palsy patients needs multiple rounds of general anesthesia, and the prognosis is poor despite the expense. Therefore, making the decision to perform multiple dental implant treatments on cerebral palsy patients is difficult. A 33-year-old female patient with cerebral palsy and mental retardation was scheduled for multiple implant treatments. She underwent computed tomography (CT) under sedation and the operation of nine dental implants under general anesthesia. Implant-supported fixed prosthesis treatment was completed. During follow-up, she had the anterior incisors extracted and underwent the surgery of 3 additional dental implants, completing the prosthetic treatment. Although oral parafunctions existed due to cerebral palsy, no implant failure was observed 9 years after the first implant surgery.
Go to :

Keywords: Cerebral Palsy, Dental Implants, Disabled Persons, General Anesthesia, Prognosis
Cerebral palsy is a non-progressive disorder characterized by clinically observed motor and postural disabilities with multiple etiologies. It can result from damage to the central nerve system before, during, or after birth [
1]. Cerebral palsy is a major cause of motor disability, with a reported incidence of 2 cases per 1000 persons. Despite the developments in perinatal care, the incidence has not changed in the recent years [
2]. Almost all patients with cerebral palsy have a disability caused by damage to the central nervous system, resulting in cognitive impairment, blindness, deafness, seizure, communication, and behavioral disturbances [
3]. For this reason, oral health management is difficult for patients with cerebral palsy, most of whom have a loss of multiple teeth and mobility of the remaining teeth due to periodontitis and dental caries.
Dental implant treatment under local anesthesia improves the masticatory function in healthy patients; however, it is difficult to maintain the mandible at a stationary position in patients with cerebral palsy due to involuntary movements of the patients. It is difficult to place implants and other prosthodontic treatment on patients with cerebral palsy. Even if treatment is successful, long-term maintenance of the implant fixture and prosthesis is difficult since force is consistently applied to them due to repetitive oral parafunction.
In addition, patients with mental retardation cannot cooperate during dental treatments, thus multiple rounds of intravenous sedation or general anesthesia must be administered. However, several rounds of general anesthesia cause extreme fatigue and thus are a large added cost to the price of the implant treatment. For this reason, it is difficult to choose implant treatment for a patient when it is hard to predict how difficult self-oral hygiene care would be and for how long they can manage self-oral hygiene.
In the present case, per the guardian's request, multiple implant surgeries and prosthodontic treatments were performed with several rounds of sedation and general anesthesia on a mentally retarded patient with cerebral palsy. Oral function rehabilitation was successfully achieved without long-term loss of the loaded implants.
CASE
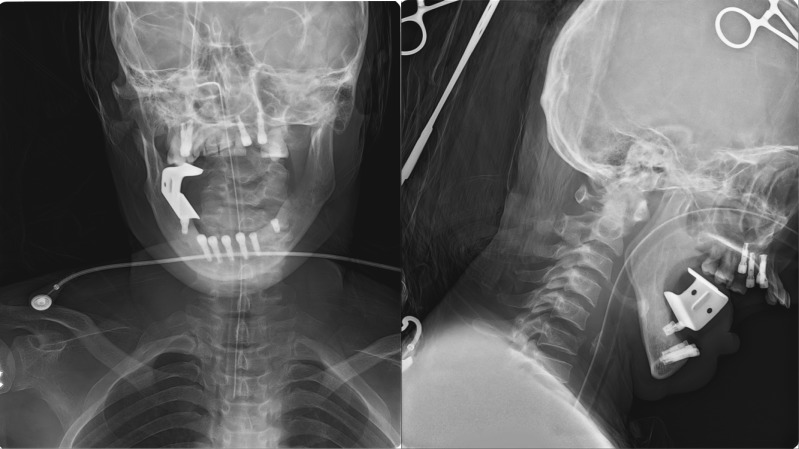
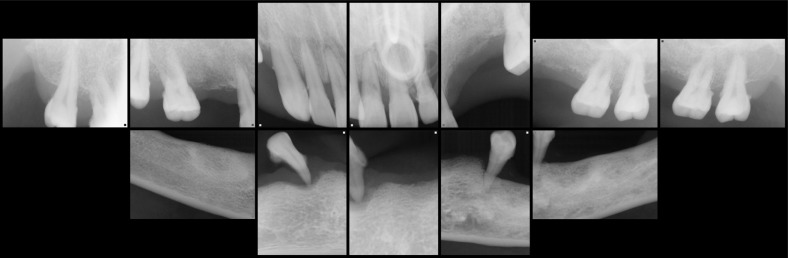
A 33-year-old female patient with cerebral palsy and mental retardation visited our clinic for dental implant treatment with the chief complaint of missing multiple teeth and mobility of the remaining teeth. Alveolar bone resorption due to chronic periodontitis was found in most teeth during the initial examination. The extraction of hopeless teeth and the rehabilitation with multiple dental implants were required. She was diagnosed with cerebral palsy at 15 months after birth. She also had difficulty communicating due to severe mental retardation. In addition, it was difficult to take intraoral radiographs because the patient made involuntary movements. At an outpatient anesthesia dental clinic, periapical radiography and extraction of #35 and #44 teeth were performed while the patient was anesthetized with 200 mg of thiopental and nasotracheally intubated using a 6.5-mm Ring-Adair-Elwyn (RAE) tube, followed by a N
2O-O
2-desflurane infusion (
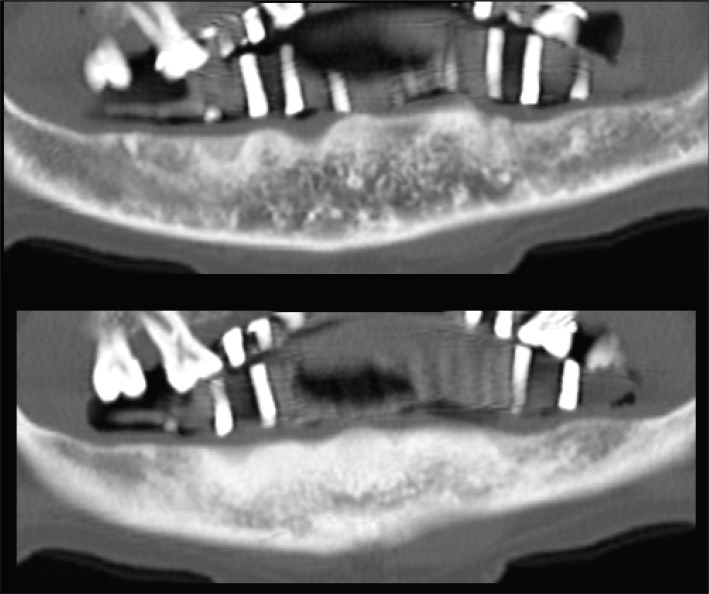
Fig. 1). It was difficult to check the bone volume, density, and location of the inferior alveolar nerve by using periapical radiographs alone. Accordingly, treatment with implants in the edentulous areas, excluding the right posterior maxillary teeth (# 17, 16, 26 and 27) and the anterior maxillary teeth (#13-22), was planned. An intraoral surgical stent was inserted for implant surgery after deep sedation was induced via target controlled infusion (TCI) of propofol at 2-3 µ/ml. Computed tomography (CT) scans were successfully obtained (
Fig. 2) [
4].
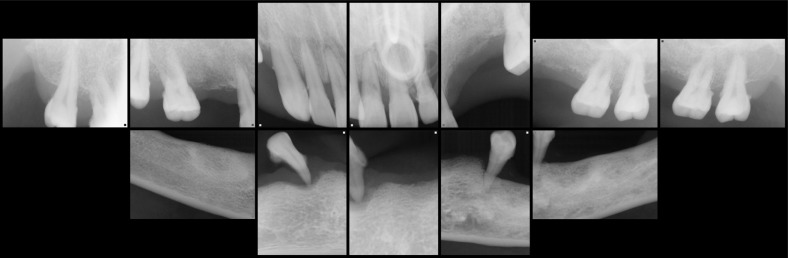 | Fig. 1The pre-operative full mouth intraoral radiograph obtained under general anesthesia.
|
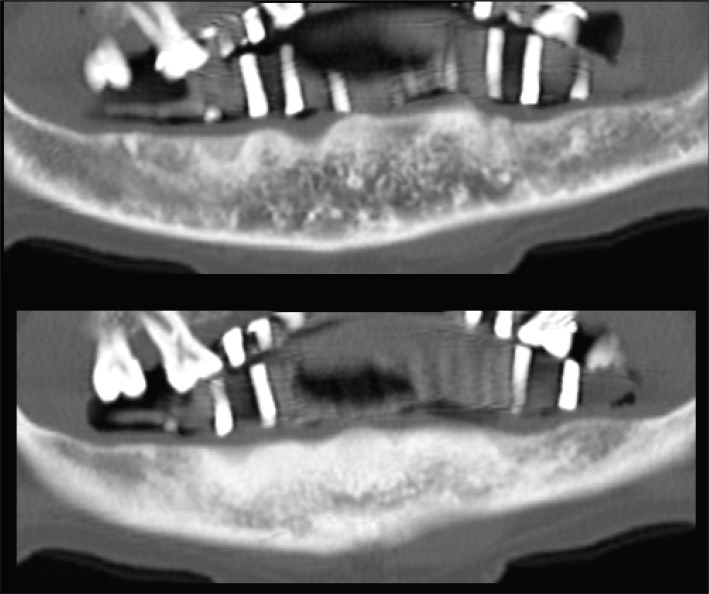 | Fig. 2Implant CT images obtained with a stent under intravenous sedation.
|
One month after the CT taking, the first implant surgery was performed. After injection of 200 mg of thiopental, followed by nasotracheal intubation using a 6.5 mm RAE tube, general anesthesia was induced by using N
2O-O
2-desflurane. To avoid inferior alveolar nerve injury, 7 mm-long fixtures were installed to the areas of teeth #36 and #46. 13-mm and 15-mm long fixtures were installed into the remaining regions (
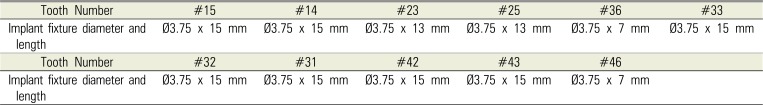
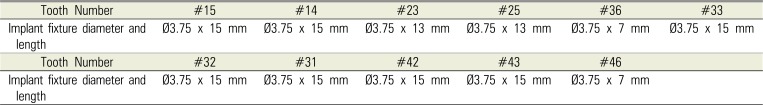
Table 1). Following implant installation, the cover screws were fixed and bone grafting was not performed. The total anesthesia time was 6 hours and the patient was discharged without any unusual complications.
Table 1
The location, diameter and length of 9-fixtures used for 1st implant operation
|
Tooth Number |
#15 |
#14 |
#23 |
#25 |
#36 |
#33 |
|
Implant fixture diameter and length |
Ø3.75 × 15 mm |
Ø3.75 × 15 mm |
Ø3.75 × 13 mm |
Ø3.75 × 13 mm |
Ø3.75 × 7 mm |
Ø3.75 × 15 mm |
|
Tooth Number |
#32 |
#31 |
#42 |
#43 |
#46 |
|
|
Implant fixture diameter and length |
Ø3.75 × 15 mm |
Ø3.75 × 15 mm |
Ø3.75 × 15 mm |
Ø3.75 × 15 mm |
Ø3.75 × 7 mm |
|

Four months after the first implant surgery, CT scans were obtained after performing TCI intravenous sedation using propofol. The obtained CT scans showed osseointegration of the all implants without bone resorption. Fixture mobility was not observed (
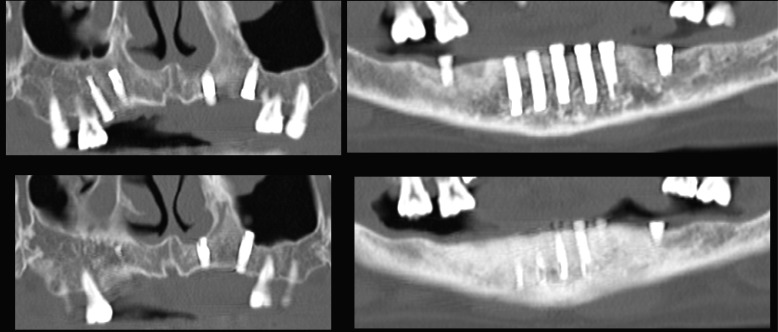
Fig. 3).
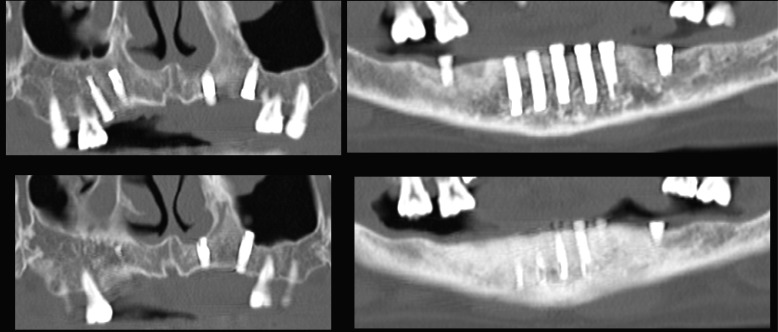 | Fig. 3Post-operative CT images (4 months after the 1st implant surgery).
|
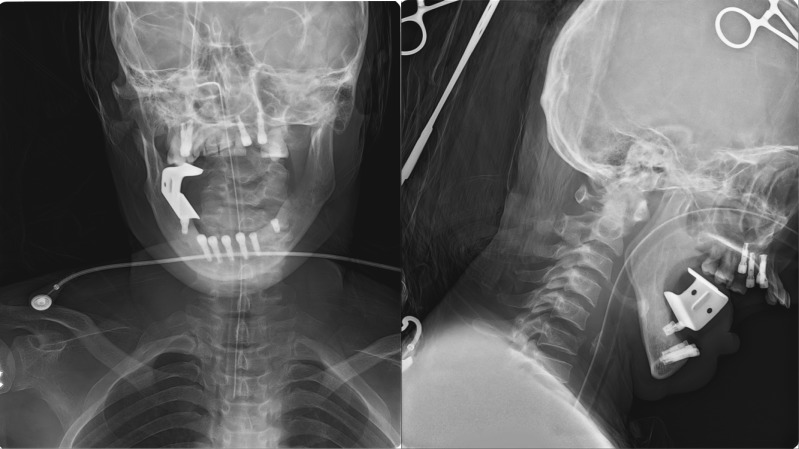
Seven months after the first implant surgery, the second implant surgery was performed. Following IV injection of 80 mg of propofol, nasotracheal intubation was performed. Then, general anesthesia was performed using N
2O-O
2-desflurane for 2.5 hours. After the cover screws were removed from 11 implants, the healing abutments were fixed. Postoperative anteroposterior and lateral cephalograms were obtained using mobile radiography equipment in the operating room (
Fig. 4).
 | Fig. 4Post-operative cephalograms after 2nd implant operation.
|
During her outpatient clinic visit after the second operation, the patient complained of pain in the area of #43 while eating. Gingival overgrowth and loosening of the healing abutments were observed around the aforementioned area. Accordingly, intravenous propofol was administered for sedation and a gingivectomy was performed at an outpatient anesthesia dental clinic.
Two months after the second implant surgery, the patient was referred to a clinic in the department of prosthodontics for restoration with a temporary implant prosthesis. Involuntary movement of the mandible led to persistent loading of the implant prostheses. As a result, some of the temporary implant prostheses fractured during the 4 years after the second implant surgery, but were regularly repaired. During the period in which the patient was treated at the department of prosthodontics clinic, only the temporary implant prostheses for teeth #23-25 were replaced with final prostheses (porcelainfused-to-gold bridge).
The patient stopped receiving treatment at our hospital thereafter and subsequently went to a local dental clinic with the chief complaint of pain of the anterior maxillary teeth. Endodontic treatment was performed on teeth #11, 21, and 22. However, consistent parafunctional activities of the anterior maxillary teeth caused by the involuntary movements of the mandible led to teeth mobility. After extraction of the anterior maxillary teeth, implant installation and implant prosthesis treatment in the areas of #11, 21, 22 were performed under local anesthesia. Maxillary incisors were ground not to contact with the opposite dentition. During the treatment period, other temporary implant prostheses were replaced with final prostheses. Although treatment was difficult due to involuntary movements made by the patient, prosthodontic treatment and implant installation on the anterior maxillary teeth could be successfully performed under local anesthesia with the aid of assistants and through communication with the patient.
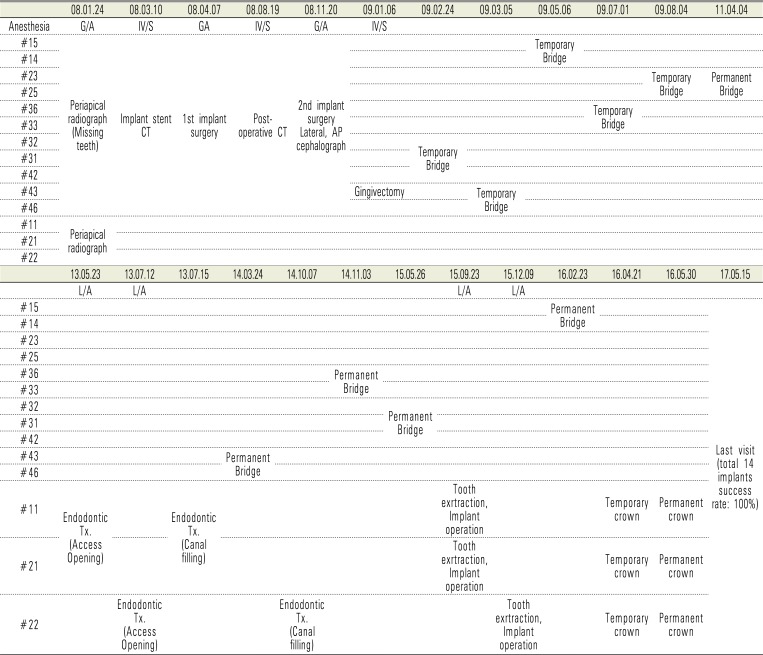
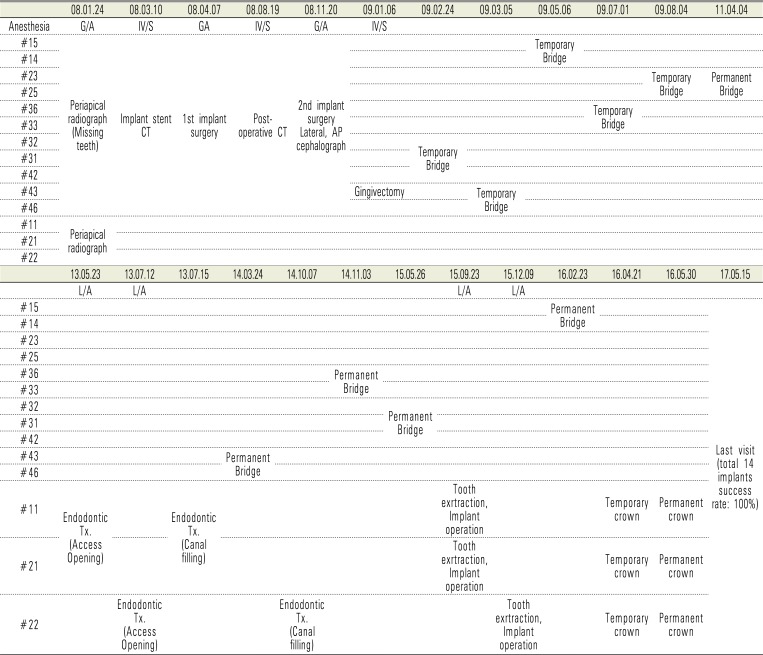
The patient's involuntary movements led to repeated parafunctional activities around the implants and the lack of attached gingiva around the implants created unfavorable conditions for implant survival. However, she maintained good oral hygiene with the help of her caregivers and masticatory function without any fixture loss of the 11 implants installed during the first operation under general anesthesia for 9 years. The treatment process for each tooth is summarized in
Table 2.
Table 2
Total treatment flow
|
08.01.24 |
08.03.10 |
08.04.07 |
08.08.19 |
08.11.20 |
09.01.06 |
09.02.24 |
09.03.05 |
09.05.06 |
09.07.01 |
09.08.04 |
11.04.04 |
|
Anesthesia |
G/A |
IV/S |
GA |
IV/S |
G/A |
IV/S |
|
|
|
|
|
|
|
#15 |
Periapical radiograph (Missing teeth) |
Implant stent CT |
1st implant surgery |
Postoperative CT |
2nd implant surgery Lateral, AP cephalograph |
|
|
|
Temporary Bridge |
|
|
|
|
#14 |
|
|
|
|
|
|
|
#23 |
|
|
|
|
|
Temporary Bridge |
Permanent Bridge |
|
#25 |
|
|
|
|
|
|
#36 |
|
|
|
|
Temporary Bridge |
|
|
|
#33 |
|
|
|
|
|
|
|
#32 |
|
Temporary Bridge |
|
|
|
|
|
|
#31 |
|
|
|
|
|
|
|
#42 |
|
|
|
|
|
|
|
#43 |
Gingivectomy |
|
Temporary Bridge |
|
|
|
|
|
#46 |
|
|
|
|
|
|
|
#11 |
Periapical radiograph |
|
|
|
|
|
|
|
|
|
|
|
|
#21 |
|
|
|
|
|
|
|
|
|
|
|
|
#22 |
|
|
|
|
|
|
|
|
|
|
|
|
13.05.23 |
13.07.12 |
13.07.15 |
14.03.24 |
14.10.07 |
14.11.03 |
15.05.26 |
15.09.23 |
15.12.09 |
16.02.23 |
16.04.21 |
16.05.30 |
17.05.15 |
|
L/A |
L/A |
|
|
|
|
|
L/A |
L/A |
|
|
|
|
|
#15 |
|
|
|
|
|
|
|
|
|
Permanent Bridge |
|
|
Last visit (total 14 implants success rate: 100%) |
|
#14 |
|
|
|
|
|
|
|
|
|
|
|
|
#23 |
|
|
|
|
|
|
|
|
|
|
|
|
|
#25 |
|
|
|
|
|
|
|
|
|
|
|
|
|
#36 |
|
|
|
|
|
Permanent Bridge |
|
|
|
|
|
|
|
#33 |
|
|
|
|
|
|
|
|
|
|
|
|
#32 |
|
|
|
|
|
|
Permanent Bridge |
|
|
|
|
|
|
#31 |
|
|
|
|
|
|
|
|
|
|
|
|
#42 |
|
|
|
|
|
|
|
|
|
|
|
|
|
#43 |
|
|
|
Permanent Bridge |
|
|
|
|
|
|
|
|
|
#46 |
|
|
|
|
|
|
|
|
|
|
|
|
#11 |
Endodontic Tx. (Access Opening) |
|
Endodontic Tx. (Canal filling) |
|
|
|
|
Tooth exrtraction, Implant operation |
|
|
Temporary crown |
Permanent crown |
|
#21 |
|
|
|
|
|
Tooth exrtraction, Implant operation |
|
|
Temporary crown |
Permanent crown |
|
#22 |
|
Endodontic Tx. (Access Opening) |
|
|
Endodontic Tx. (Canal filling) |
|
|
|
Tooth exrtraction, Implant operation |
|
Temporary crown |
Permanent crown |

Go to :

DISCUSSION
Cerebral palsy is a non-progressive disorder characterized by behavioral and postural disabilities. It is caused by environmental and various other factors. Intrauterine hypoxia is the main cause. Spastic quadriplegia is reported to be the most common type of cerebral palsy [
5]. Periventricular hemorrhage can cause cerebral palsy in premature infants. Fetal infection, thyroid disease, neuronal migration disorder, and genetic disorders, aside from hypoxia, can all cause cerebral palsy in term infants. Causes of cerebral palsy after birth include meningitis, viral encephalitis, hydrocephalus, and brain damage [
6]. Most patients with cerebral palsy have impaired reflexes and involuntary movements, in addition to muscle spasms and limb paralysis, which are most often accompanied with cognitive impairment, blindness, deafness, seizure, and communication and behavioral disturbances [
7].
Patients with cerebral palsy have poor oral hygiene due to motor disabilities and other disorders. And this leads to high incidences of dental caries, periodontitis, and malocclusion of these patients [
8]. Although most patients with cerebral palsy do not have severe mental retardation and have no difficulties with communication, patients with impaired motor and reflex functions and involuntary movements are reluctantly unable to cooperate during treatment. Furthermore, patients with cognitive disorders, such as mental retardation, experience anxiety and fear during dental treatment. It is even more difficult to perform dental treatment on patients who have serious medical disorders such as epilepsy. Therefore, it is impossible to treat these patients without sedation or general anesthesia [
9].
With the recent economic advancement, the demand for dental treatment has diversified. Whereas simple dental procedures, such as tooth extraction or amalgam filling for dental caries, were performed in the past, complex and diversified dental treatments such as endodontic and prosthodontic treatment, and even orthodontic treatment and dental implant surgery are currently being performed, despite involving multiple rounds of general anesthesia or sedation [
10]. Generally, CT is necessary for implant installation. However, in order to obtain clean CT images without noise caused by the patient's movement, sedation or general anesthesia may be needed [
4].
Loyola-Rodriquez et al. report cases of successful restorative and endodontic treatment, tooth extraction, and orthodontic treatment using sedation and general anesthesia in patients with cerebral palsy classified as ASA II-III or Frankl's scale stage I-III [
11]. They performed dental treatment on 38 patients with cerebral palsy after performing ambulatory anesthesia using sevoflurane-propofol and general anesthesia on pediatric patients (70 min) and adults (120 min). After a short recovery period of 20 to 40 min, the patients were discharged without any complications. In the present case, the patient's oral function was successfully recovered through an implant surgery and prosthodontic treatment with multiple rounds of sedation and general anesthesia.
Numerous cases of dental implant treatment on patients with various neurological disorders such as cerebral palsy, Down syndrome, Parkinson's disease, and severe epilepsy have been reported. However, the previous literature has been limited to the installation of a small number of implants or implant installation for implantsupported overdenture [
12131415161718]. Ekfeldt [
15] investigated implant survival rates among 14 patients with neurological disorders. Fourteen patients with 35 implants were treated. Three implants were lost before or at the time of second-stage surgery. Two implants were lost after loading. Cune et al. [
17] report a high implant survival rate of 97.6% in their long-term retrospective study of 61 patients affected by severe, refractory epilepsy and multiple disabilities in whom a combined total of 134 implants were installed. However, their study did not include patients who underwent multiple-implant installations. Feijoo et al. [
18] investigated the survival rates of a total of 18 implants installed in 8 patients with intellectual disability. However, the follow-up period in their study was only 1 to 3 years and the number of implants installed for each patient was low.
The patient in this case report, who had mental retardation and cerebral palsy, recovered her masticatory function through multiple-implant installations and fixed prosthesis treatment of the maxillary anterior and, bilateral premolars, and the mandibular area. She showed a good prognosis without implant loss after a long period of follow-up, and she was the first patient to be reported. The patient's involuntary movements caused parafunctional activities around the implants, which led to fracture of implant prostheses. Although it was difficult to maintain the implants for a long period of time due to the lack of attached gingiva; peri-implantitis was prevented through appropriate oral hygiene care by her caregiver.
General anesthesia or sedation was needed for the preoperative CT scan and multiple-implant installations in the edentulous area, but prosthodontic and endodontic treatments and implant surgery on the anterior maxillary area, which were performed later, only required local anesthesia. A trusting relationship developed between her and medical staff during treatment period made this possible. The level of patient's anxiety was alleviated, and medical staff got well prepared for her involuntary movements. As observed in this case, successful rehabilitation and long-term management of oral function could be achieved through surgery using sedation and general anesthesia (including multiple-implant installation) and omanagement of oral hygiene, even in patients with poor oral habits due to neurological disorders.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download