Abstract
The use of novel oral anticoagulants (NOACs) has increased in recent times in an effort to overcome the shortcomings of warfarin. They are being used primarily for the prevention of thrombosis caused by atrial fibrillation and offer the advantages of having fewer drug interactions than warfarin, no dietary restrictions, and no requirement for regular blood tests. Although there is reportedly less postoperative bleeding even if the drug is not discontinued during procedures that can cause local bleeding, such as dental procedures, no well-designed clinical studies have assessed postoperative bleeding associated with the use of these drugs. This article reports a case of a 74-year-old male patient who was taking rivaroxaban. The patient underwent a dental implant procedure after discontinuing rivaroxaban for one day and subsequently suffered delayed bleeding on postoperative day 6. Accordingly, this article also reports that the use of NOACs may also lead to delayed bleeding.
Anticoagulants are used extensively for prophylactic prevention of embolism or stroke in patients with atrial fibrillation, those who have undergone mechanical heart valve surgery, and for therapeutic purposes in cases involving venous thromboembolic diseases. Although warfarin is the most common oral anticoagulant, it requires continued monitoring via international normalized ratio (INR) due to its interactions with other drugs and foods and dosage adjustment is difficult due to its narrow therapeutic range [1].
The use of NOACs such as dabigatran, rivaroxaban, apixaban and edoxaban has been increasing as an atrial fibrillation drug. Unlike warfarin, dabigatran is a direct thrombin inhibitor, whereas the others are oral direct factor Xa inhibitors. Moreover, because they have fewer interactions with other drugs and foods, they do not require dosage adjustment or regular blood tests, while their peak plasma levels at 2–5 hours and half-life of 7–20 hours are shorter than those of warfarin, meaning that the effects of taking or discontinuing the drug appear with 1–2 days (Table 1). However, an increased risk of bleeding from taking anticoagulants is also problematic for NOACs. The risk of bleeding for NOACs is reportedly similar to or less than that of warfarin. However, not having an adequate reversal agent is one of their shortcomings [2]. Although protocols and guidelines have been published for patients undergoing dental treatments, especially invasive dental procedures, while taking NOACs [34], systematic studies on the topic are still lacking [5].
This article reports a case of delayed bleeding after implant placement in a patient taking rivaroxaban for atrial fibrillation.
A 74-year-old male patient was admitted to the Department of Advanced General Dentistry at Yonsei University College of Dentistry on 2014, for a chief complaint of loosening of the restoration that was covering his teeth (Fig. 1). The patient had experienced a stroke in 2000 and was taking warfarin, 2.5 mg PO bid, due to atrial fibrillation. In addition, the patient was taking medications for hypertension (candesartan, atorvastatin, spironolactone, and carvedilol). At the time of admission, his INR value was 4.76. Clinical examination and radiological findings indicated the presence of residual root in the maxillary right second molar while existing restoration of the maxillary left canine, first premolar, and second premolar had fallen out. The Department of Cardiology at our hospital was consulted to determine whether the patient was operable and whether warfarin could be discontinued or changed. The response to the consultation was that the patient could receive dental treatments, and, in case of a high risk of bleeding, heparinization on an inpatient basis or use of low molecular weight heparins (LMWH) on an outpatient basis would be possible. Accordingly, extraction of the maxillary right residual root and prosthetic treatment following crown lengthening on the maxillary left canine, first premolar, and second premolar was planned. The treatment plan for the maxillary and mandibular missing posterior teeth (maxillary left first and second molars and mandibular right second molar) was to be reestablished after treating the area of chief complaint.
Warfarin was discontinued from three days prior to the treatment, and from two days prior to treatment, LMWH (Enoxaparin, Clexane, Sanofi-Aventis, France), 60 mg bid. was injected subcutaneously. On the day of treatment, LMWH injection was discontinued and full-mouth supragingival scaling and extraction of the maxillary right residual root were performed. Crown lengthening was performed by ostectomy of the alveolar bone after flap elevation on the area around the maxillary left canine and first and second premolars. In addition, dental pulp extirpation was performed on the maxillary left canine and second premolar. After suturing the area with 4–0 vicryl suture, hemostasis was confirmed by gauze biting for 1 hr. Starting from the evening of the day of treatment, subcutaneous injection of LMWH and warfarin administration was initiated. LMWH was continued for two more days. On the following day, hemostatic status was confirmed while dressing the area and the stitches were removed after one week. Subsequently, endodontic and prosthetic treatments were completed without discontinuing warfarin.
About one year after treatment completion, implant placement was planned on the left maxillary first and second molars (Fig. 1). Since medication was switched from warfarin to 20 mg of rivaroxaban (Xarelto, Bayer HealthCare AG, Germany) two months earlier, consultation was requested on whether surgery was feasible and whether the medication should be discontinued, to which the response was to discontinue rivaroxaban from the morning of the day before the procedure and to restart as soon as possible afterwards. The day of surgery, his systolic and diastolic blood pressures were 133 and 80 mmHg, respectively. After local anesthesia on the left maxillary first and second molars using 2 ampoules of 2% lidocaine containing 1:100,000 epinephrine, two implants (diameter 5.0 mm and length 8.0 mm) were placed with full thickness flap elevation (Fig. 2B) and a healing abutment (diameter 5.5 mm) was screwed onto the implants (Fig. 2A, C). After suturing with 4–0 vicryl suture, pressure was applied with gauze to stop the bleeding and the patient was discharged on the same day after confirming that the bleeding had stopped.
On the day after the procedure, since there were no signs of infection or bleeding, the patient was instructed to restart rivaroxaban. On post-operative day (POD) 6, the patient visited the dental emergency room at our hospital around 4 AM for a chief complaint of spontaneous bleeding at the surgical site. Oozing bleeding in the area was observed, and pressure was applied with a gauze to stop the bleeding for about one hour, after which the patient was discharged after confirming that the bleeding had stopped (Fig. 2C). On the same day, the patient visited our department again at about 5 PM for re-bleeding at the surgical site that had started about an hour earlier. However, the bleeding could not be stopped, despite applying pressure with gauze; therefore, oxidized regenerated cellulose (ORC) was applied to the bleeding area. After about an hour, the bleeding had stopped, but because of the possibility of continued bleeding, the decision was made to discontinue rivaroxaban for one day. On the next day (POD 7), the patient was admitted to the dental emergency room again at about 1 AM for bleeding in the same area. Slightly pulsating oozing bleeding was observed in the same area and the existing ORC was removed and new ORC was applied while simultaneously applying pressure with gauze to stop the bleeding. On POD 8, since no further bleeding was observed, the patient was instructed to restart rivaroxaban. One week thereafter (POD 14), the stitches were removed.
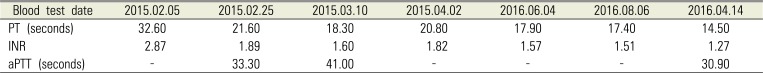
NOACs do not generally have a separate monitoring method and are not closely associated with INR or activated partial thromboplastin time (aPTT) that are widely used as indicators of bleeding trend; thus, determining the risk of bleeding is difficult when administering bleeding-related treatments to patients. The patient in the present case had an INR value of 1.2–1.5 while taking rivaroxaban, higher than normal level, but it was a lower than while taking warfarin (prior to August 2015). Moreover, the aPTT value was within the normal range while taking warfarin or rivaroxaban (Table 2). When treating patients who are taking NOACs, the following considerations are recommended [13567]. First, the risk of bleeding must be assessed. A switch-in medication may not be necessary for infiltrative anesthesia or supragingival periodontal treatment. Simple extraction of less than 4–5 teeth, biopsy within a limited range, or placement of a single implant may present moderate risk of bleeding, but local hemostasis without change in medication is recommended. For extraction of a greater number of teeth, complex extractions, and ostectomy involving dental root surgery, excision of torus or multiple implants, consultation with an internal medicine specialist and discontinuation of medication for over 24 hours are recommended. Secondly, assessment of the drug (s) currently taken is also necessary. As shown in Table 1, the discontinuation period for each drug may vary due to differences in the peak plasma level, half-life, and elimination method for each type of NOAC. Finally, confirmation of renal function is also necessary. Depending on the type of NOACs, due to differences in the degree of excretion into the kidneys, the duration of drug withdrawal may vary depending on the patient's renal function [2].
The patient in the present case had a high probability of bleeding since he was scheduled to undergo a procedure involving the placement of two implants accompanied by an ostectomy; as such, rivaroxaban was discontinued for one day. Moreover, since the patient had no previous experience with delayed bleeding from dental treatments while taking warfarin and did not show any problems with renal function, the discontinuation duration of one day was considered to be sufficient. However, unexpected delayed bleeding occurred on POD 6, and, despite applying local pressure with gauze and using hemostatic agent, bleeding recurred. Because of the risk of additional bleeding, rivaroxaban was discontinued for one day in addition to continued local hemostasis, which resolved the delayed bleeding issue.
NOACs offer the advantages of reduced risk of bleeding by discontinuation of treatment for a period of just 1–2 days; reduced risk of thrombosis since the drug effect can be seen within hours of taking the drug; and increased patient compliance for drug discontinuation and restarting. Even for implants that require the flap being pulled back, no significant instances of postoperative bleeding without discontinuation or dose adjustment of rivaroxaban have been reported [8]. Moreover, patients taking rivaroxaban undergoing dental treatments included ostectomy without dosage adjustment experienced a statistically significantly increased tendency for postoperative bleeding compared to patients who were not taking anticoagulant or antiplatelet drugs. However, it was possible to stop the bleeding by applying local pressure, additional suturing, or applying topical anticoagulants [9]. Postoperative bleeding is reported in 0.7% of cases in which an anticoagulant or antiplatelet drug was not being taken, with bleeding appearing immediately after the procedure. Postoperative bleeding was observed in 11.5% of cases in which the patient was taking rivaroxaban, with bleeding reported from POD 1 to 6. Even in such cases, the bleeding was stopped by local hemostatic methods, while some cases required the use of fibrin glue or additional suturing. Thus, most reports have indicated that bleeding was not a major issue even without adjustment to rivaroxaban. In the present case, rivaroxaban was discontinued for one day prior to the procedure. Although ORC was used in addition to local hemostatic measures for treatment of delayed bleeding that occurred on POD, rivaroxaban was discontinued for one day additionally. These results suggest the need to recognize that bleeding will always be an issue in patients taking anticoagulants.
Moreover, considering no adequate reversal agent is available, necessary preparations should be made for postoperative delayed bleeding when providing dental treatments to patients taking NOACs. This means that atraumatic procedures should be performed, local hemostasis using gauze should be applied, primary closure of soft tissues without dead space is required, and fibrin glue and absorbable agents such as ORC and gelatin sponge should be readied in case of bleeding [7]. Furthermore, in case of indication, it may also be helpful that surgical procedures that best minimize the factors involved in bleeding such as flapless implant using computer-assisted implant guides.
References
1. Jhonston S. An evidence summary of the management of patient taking direct oral anticoagulants (DOACs) undergoing dental surgery. Int J Oral Maxillofac Surg. 2016; 45:618–630. PMID: 26774397.
2. Elad S, Marshall K, Meyerowitz C, Connolly G. Novel anticoagulants: general overview and practical considerations for dental practitioners. Oral Dis. 2016; 22:23–32. PMID: 26386350.

3. Breik O, Cheng A, Sambrook P, Goss A. Protocol in managing oral surgical patients taking dabigatran. Aust Dent J. 2014; 59:296–301. PMID: 24889878.

4. Romond KK, Miller CS, Henry RG. Dental management considerations for a patient taking dabigatran etexilate: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:e191–e195. PMID: 23850368.

5. Constantinides F, Rizzo R, Pascazio L, Maglione M. Managing patients taking novel oral anticoagulants(NOAs) in dentistry: a discussion paper on clinical implications. BMC Oral Health. 2016; 16:5. PMID: 26822674.

6. Firriolo FJ, Hupp WS. Beyond warfarin: the new generation of oral anticoagulants and their implications for the management of dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:431–441. PMID: 22668425.

7. Hong CH, Islam I. Anti-thrombotic Therapy: Implications for Invasive Outpatient Procedures in Dentistry. J Blood Disorder Transfus. 2013; 4:166.
8. Gómez-Moreno G, Aguilar-Salvatierra A, Fernández-Cejas E, Delgado-Ruiz RA, Markovic A, Calvo-Guirado JL. Dental implant surgery in patients in treatment with the anticoagulant oral rivaroxaban. Clin Oral Implants Res. 2016; 27:730–733. PMID: 26073481.

Fig. 1
Panoramic image from the initial examination (red arrow: area of chief complaint during the initial examination; blue arrow: planned sites for implantation).
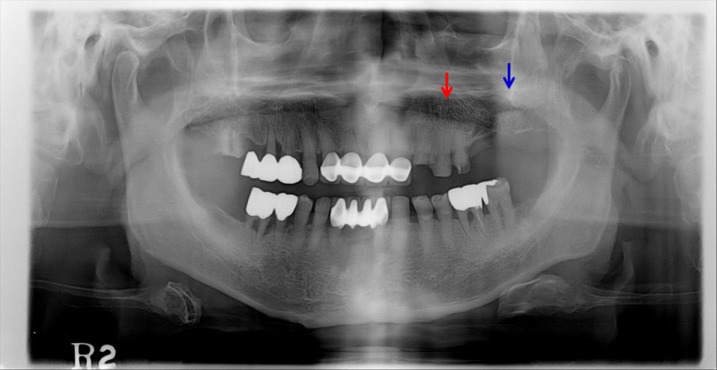
Fig. 2
(A) Panoramic image after the implant placement procedure (yellow arrow: implant placement sites), (B) Clinical photo during implant placement procedure (after flap elevation), (C) Clinical photo after implant placement and site of postoperative delayed bleeding (green arrow).
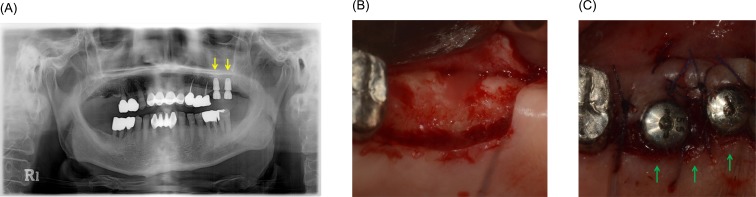
Table 1
List of NOACs and properties [1]
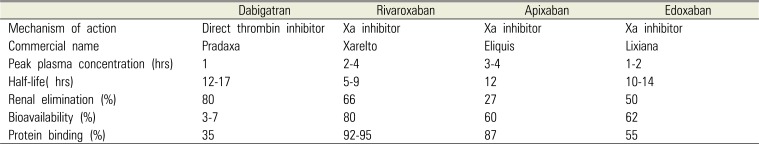
Table 2
Blood test results related to bleeding from before and after changes to anticoagulant in the patient




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download