INTRODUCTION
With the expansion of the use of national healthcare insurance in Korea, two implants are now allowed for patients over 65 years of age in 2017. Elderly patients have various systemic diseases and often take many medications. Given the possibility of deficiency of the residual alveolar ridge due to alveolar ridge resorption, complications such as intraoperative or postoperative bleeding, infection, osteonecrosis of the jaw, and nerve damage are likely during implant surgery. In order to prevent this situation, it is essential to know in advance about the patient's systemic diseases, medical status, and current medications.
Since July 2014, national healthcare insurance has been applied to implant treatment in patients over 75 years of age. In the partial rehabilitation of the edentulous alveolar ridge of elderly patients, an implant has been chosen as the main treatment method to restore the masticatory function. Dental visits that have been delayed due to economic problems are increasing in elderly patients with the emergence of insurance coverage. The demand for implant therapy is expected to continue to increase as the number of elderly people aged 65 or older increases. Implant treatment can be divided into surgical and prosthetic steps. The surgery is accompanied by surgical trauma. In young and healthy patients, surgical trauma that occurs during implant surgery is not common, as the patient's capacity to heal is mostly normal in this population. However, in order to successfully perform implant surgery in elderly patients, many considerations must be taken into account, particularly the patient's systemic disease and the medications that are being taken.
A recent retrospective study of implant surgery in the elderly reported that the success rate of implants in patients with systemic disease was not significantly different from that in healthy patients, but that adequate systemic evaluation before surgery can reduce complications [
1]. After coverage of national healthcare insurance for implants began in 2014, no studies have investigated the complications of implant treatment, and in particular, surgery, and there have been no reports about the general state of the patient. The purpose of this study was to investigate the clinical characteristics of patients who underwent implant surgery from October 2013 to October 2016 in the Department of Advanced General Dentistry at Yonsei University, Seoul, Korea, and to determine information that dental clinicians should review to prevent emergencies during surgery, including the presence or absence of systemic diseases, the use of medications, and the control of these medications for implant surgery.
MATERIALS AND METHODS
Participants in this study comprised 126 patients aged 65 years or older who underwent primary implant surgery at Yonsei University College of Dentistry Hospital From October 1, 2013 to October 30, 2016.
An institutional review board granted approval for this retrospective study. Electronic chart review was conducted to obtain medical records, which included sex, age, systemic diseases, medication(s) being taken, and control of the medications. The systemic disease of the patient was confirmed in an interview at the first visit and at a consultation. Medications being taken were identified via an electronic medical record (EMR), if available, at the Severance Hospital. Prescriptions of medications by an outside hospital were confirmed via reply to a consultation request letter from the hospital. Disease classification was conducted in accordance with WHO International Classification of Disease-10 (ICD-10). Complications during and after implant surgery were also investigated.
The medications that were examined at the time of surgery include anticoagulant and antiplatelet agents that can cause bleeding, bisphosphonate drugs that can cause jaw necrosis, and immunosuppressant and corticosteroid agents.
DISCUSSION
According to application of the national healthcare insurance in Korea for implant treatment since July 2014, it is expected that the treatment of elderly patients over 65 years of age with edentulous alveolar ridge implant surgery will increase. According to statistics from the National Statistical Office for the Elderly in 2016, the number of people aged 65 years or older is 6.57 million as of 2015, which is steadily increasing at 13.2% of the total population. It is expected that the demand for this surgery will gradually increase with the aging society. The most important outcome of our study was that 88.9% of the patients in the study group were taking a medication and had more than one disease. A thorough evaluation of pre-operative systemic disease is therefore important for safe complication-free procedure without complications.
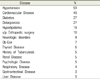
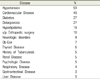
Although not investigating implant surgery, a 2014 study on the use of outpatient drugs in elderly patients in a university hospital analyzed the frequency of major diagnoses in patients older than 65 years of age and found that the 10 most common diseases were diabetes, angina, hypertension, cerebrovascular accident, idiopathic pain, asthma, benign prostate hypertrophy, atrial fibrillation, Parkinson's disease, and cataract. The average number of medications prescribed was 5.2, and the number of medications tended to increase as age increased beyond 60 years of age [
2]. When trends in drug use among elderly patients were examined, the results indicated that it was most common to take drugs for the cardiovascular system (30.7%), followed by drugs for the gastrointestinal system and endocrine system (22.6%) and drugs for the neurologic system (16%). Although this study showed a similar pattern to our study, it was not common for the patients in our study to be taking drugs for severe neurological diseases (e.g. Parkinson's). The reason for this difference could be that patients visiting dental clinics have fewer problems with communication and movement in their daily lives and therefore they are willing to be treated for their dental problems.
Complications that may occur after implant placement include bleeding, infection, and nerve damage [
3]. In older patients, complications from systemic disease should also be considered [
4]. For example, during dental treatment, surgery in the oral cavity is accompanied by local bleeding, and patients with cardiovascular disease are often taking anticoagulant medications for therapeutic or prophylactic purposes or have a dysfunctional hemostatic process due to congenital diseases.
In our study, 35.7% of the patients in the study group were taking anticoagulants. Of these patients, 75.6% received dental treatment after discontinuing their medications, 11.1% received treatment while still on medication, and 6.7% were treated after changing their drug from Coumadin to heparin. In cases in which patients were taking a drug associated with a risk of bleeding, more than half of the patients were not considered to be at high risk for cardiovascular disease, even if the drug was to be temporarily stopped.
The most commonly used drug was aspirin, which is prescribed for patients with coronary artery occlusive disease, hypertension, and diabetes. To prevent complications in patients with hypertension and diabetes, which is often treated with an antiplatelet agent, aspirin or other antiplatelet drugs are often taken for therapeutic purposes. This is done to prevent re-stenosis after treatment in patients with vascular disease, especially those with a previous history of PTCA (percutaneous transluminal coronary angioplasty), CABG (coronary artery bypass graft), and stroke. Prophylactic antiplatelet agents may be temporarily discontinued, but in patients who are more at risk for blocked blood vessels, heart attack and stroke are more likely to occur when the antiplatelet agent is discontinued. These patients should thus continue to maintain the drug. It is recommended that hemorrhage due to dental surgery be controlled by a local hemostatic method, such as collagen plug use or continuous pressurized hemostasis [
5].
Warfarin (coumadin) is an example of an anticoagulant drug that is more powerful than antiplatelet agents. The diseases for which it is most commonly prescribed are myocardial infarction, cerebrovascular accident, thrombophlebitis, severe cerebrovascular disease, open heart surgery, which includes heart valve surgery, and atrial fibrillation for the prevention of thrombosis [
6]. Therefore, the use of anticoagulants should always be considered when obtaining the medical history of patients with a history of these diseases. When deciding to discontinue warfarin, the doctor should consult with the physician about the risks of the occurrence of cardiovascular disease and of hemorrhage at the time of dental surgery, and the final decision should be that which is likely to yield the greatest benefit to the patient.
There are five ways to control drug administration when patients are taking anticoagulants. These include the following: 1) Discontinuing anticoagulant 2) Bridging therapy with hospitalization, or stopping the anticoagulant and replacing it with intravenous heparin 3) Discontinuing anticoagulant on an outpatient basis with subcutaneous administration of low molecular weight heparin (LMWH) 4) Decreasing the dose of anticoagulant 5) Retaining anticoagulant [
6]. Although bridging therapy has the drawback of requiring hospitalization, it is commonly used in patients with heart valve replacement surgery, and especially in those with mechanical valves that must remain anticoagulated. Heparin acts as a catalytic agent and plasma antithrombin III acts as an anticoagulant. Standard heparin that is used in bridging therapy has an average molecular weight of 12,000 to 16,000. Intravenous administration of heparin is performed in the hospital and activated partial thromboplastin time monitoring is performed. In addition, it has a half-life of 1-2 hours, and thus is discontinued 4-8 hours before surgery, after which the operation can proceed. In recent years, LMWH has been used instead of conventional heparin to reduce hospitalization hassles. LMWH produces heparin fragments with an average molecular weight of 4,000 to 6,000 and is administered subcutaneously in the abdomen. The dose is based on body weight and no laboratory monitoring is required. The half-life is 2 to 4 hours and can be provided externally [
7]. If a patient does not control his/her medication, the risk of bleeding can potentially be resolved with a change in dental treatment plan, such as computer guided surgery or flapless implant surgery using a surgical stent. These measures can be helpful, and thus their aggressive use is recommended if the patient is unable to discontinue anticoagulant medication.
Osteoporosis is a skeletal disease that weakens the strength of the bone. While osteoporosis itself is not known to be a contraindication to implant placement, poor bone quality may require that appropriate surgical techniques, such as undersize of bone preparation and bone compaction are used, and an implant design is chosen that maximizes nitial stability [
8].
In patients taking bisphosphonate for the treatment of osteoporosis, however, long-term failure during follow-up, rather than early failure, may occur, which is due to the possible development of bisphosphonate-associated osteonecrosis of the jaw (BRONJ). It is thus important to accurately determine the patient's osteoporosis status and history of drug use even after implant placement. The results of this study showed that drug use could be confirmed in all but one osteoporosis patient, and that patients with a history of bisphosphonate drug use were treated with implant therapy after an average of 3 months of drug withdrawal.
Bisphosphonate is a major osteoporosis drug that inhibits osteoclast function, which then inhibits bone resorption and is therefore used to treat and prevent complications of osteoporosis in the skeletal system [
9]. When evaluating a history of osteoporosis drug use, it is necessary to examine the specific osteoporosis medication, the ingredients in the medication, and the period of time over which the medication has been taken. This can be confirmed through collaboration with relevant internal medical physicians. There is some controversy over the drug holiday at which patients who have a history of taking anti-resorptive agents should undergo implant placement and extractions. According to the AAOMS position paper revised in 2009, we recommend stopping the drug three months before and after surgery, as long as the systemic condition permits [
10]. However, there is no clear evidence that drug withdrawal reduces the likelihood of osteonecrosis when taking bisphosphonate medications. In 2011, The ADA council provided a recommendation period for drug withdrawal based on the fact that a history of more than 4 years of bisphosphonate use increases the likelihood of osteonecrosis after invasive dental treatment. Thus, in this case, it is recommended to discontinue drug use [
11]. The main reservoir in the serum of bisphosphonate is osteoclast, which survives for two weeks. Since bisphosphonate remaining in the serum is mostly depleted after 2 months, a drug holiday of more than 2-month time is recommended [
10].
A recently developed osteoporosis drug, denosumab, acts as a RANK ligand (RANK-L) inhibitor, which inhibits bone resorption. Bisphosphonate is deposited to the bone at the site of bone resorption, and when osteoclasts absorb bisphosphonate, they lose osteoclast function. In contrast, denosumab binds to RANK-L similar to an antibody, which impairs osteoclast function. Denosumab differs from bisphosphonate in that it does not directly attach to the bone to modulate the effects of the skeletal disease associated with bone metabolism. An advantage to this is that after 6 months of discontinuation, most of its effects are resolved. However, the occurrence of osteonecrosis of jaw was also reported after taking denosumab [
9]. No patients in this study were taking denosumab, perhaps because it was recently developed. As the number of patients to be treated is expected to increase, this medication should be considered and examined in the future.
If a patient has a severe end-stage disease of the kidney, liver, or bone marrow, organ transplantation is often considered. The main complication in organ transplantation is graft rejection. It is therefore necessary to prepare for surgery with immunosuppression and continue long-term immunosuppressive therapy after surgery. Immunosuppression increases a patient's vulnerability to infection and can lead to poor wound healing. It is thus necessary to confirm whether this type of treatment can cause oral infection before and immediately after surgery, which are the most vulnerable and susceptible times for infection. This should be carefully examined and patients should be treated for any complications due to infection [
12]. The most commonly used immunosuppressants after transplantation are cyclosporine, azathioprine, prednisone, and antilymphocyte agent. In addition, a high dose of corticosteroid-induced immunosuppressive agents is initially administered after organ transplantation. In this case, vulnerability to infection related to dental treatment is a possibility, but the relationships among oral bacterial, viral, and fungal infection as a side effect after organ transplantation is not well understood. However, there has been a rare case of bacterial infection caused by aspiration in periodontal bacteria and lung transplant patients [
12]. Therefore, pre-operative and follow-up screening and treatment of patients who are undergoing organ transplant surgery is needed. All 4 of the organ transplant patients in this study were stable after organ transplantation, and there were no major problems associated with the operation. A periodic evaluation is needed, however, to confirm long-term success.
In conclusion, in this study, we investigated the general medical history and drug use of patients over 65 years of age that received implant treatment. A large number of patients had systemic diseases, and most were taking medications related to their treatment. In order to reduce the complications associated with implant surgery, patients should be examined for systemic diseases, and the patient's condition should be determined through consultation with the physician.