Abstract
Eisenmenger syndrome (ES) is characterized by pulmonary arterial hypertension and right-to-left shunting. The signs and symptoms of ES include cyanosis, shortness of breath, fatigue, hemoptysis, and sudden death. In patients with ES, it is important that the systemic and pulmonary circulations be properly distributed and maintained. General dental treatment is not known to be particularly dangerous. To control pain and anxiety, local anesthetics without epinephrine are usually recommended. However, in cases of difficulty of cooperation, general anesthesia for dental treatment makes the condition worse. In the present case, intravenous deep sedation with propofol and remifentanil was administered for behavioral management during dental treatment successfully.
Eisenmenger syndrome (ES) refers to pulmonary hypertension accompanied by right-to-left or bidirectional shunt. When the pulmonary vascular resistance (PVR) exceeds the systemic vascular resistance (SVR), the arterial flow converts into a right-to-left shunt, resulting in manifestation of symptoms such as cyanosis, shortness of breath, fatigue, and arrhythmia [1]. Behavioral management including general anesthesia are required when patients with Down syndrome with developmental disorders, such as mental retardation, have difficulties in cooperating with dental treatments. However, when such cases are accompanied by ES due to congenital heart malformation, general anesthesia is contraindicated since it can result in high mortality associated with aggravated hypoxia or right ventricular failure [2].
By applying a sedation technique, the powerful vasodilation effect and suppression of cardiac contraction caused by general anesthetics can be avoided, while also preventing elevated PVR from positive pressure breathing [3]. We hereby present a case report of a patient with ES with intellectual disability in the form of Down syndrome, who successfully underwent dental treatments under deep sedation using propofol and remifentanil.
A 12-year-old female patient with Down syndrome (weight 35 kg, height 135 cm) was referred to the department of dental anesthesia for behavioral management. Behavioral management was difficult because of her congenital heart condition, and uncooperativeness due to intellectual disability and dental phobia. Her chief complaints were pulp exposure, necrotic change, and pus discharge in the right mandibular first molar. Meanwhile, a root canal procedure was planned with a pediatric dentist.
The patient was given birth by normal spontaneous vaginal delivery with birth weight of 3.0 kg, and was diagnosed with chromosome 47XX + 21 Down syndrome. Immediately upon birth, she was also diagnosed with ventricular septal defect, for which she underwent regular examinations without any surgical intervention. At age 5, cardiac catheterization found severe pulmonary hypertension, based on which a diagnosis of ES was made (Fig. 1).
Echocardiography results indicated bidirectional shunt due to large perimembranous ventricular septal defect, resulting in severe pulmonary hypertension. A chest radiograph showed no significant interval changes, while laboratory test results showed hemoglobin and hematocrit level of 14.2 g/dl and 41.2%, respectively. Other laboratory findings were unremarkable.
Preoperative physical examination results showed blood pressure of 110/70 mmHg, heart rate of 100 beats/min, and oxygen saturation of 91%. Her physical activity was identified as NYHA (New York Heart Association) class II, meaning mild symptoms (mild shortness of breath and/or angina, and slight limitation during ordinary activity). A pediatric cardiologist recommended avoiding general anesthesia since it could threaten her life, and instead, recommended the use of antibiotics (bacterial endocarditis) and lidocaine without epinephrine, prevention of air embolism, and prevention of an increase in PVR during anesthesia and recovery period.
A pediatric dentist had planned to perform root canal treatment on one tooth with expected procedure time of no more than 1 hour. In order to lower the risk of anesthesia, sedation using co-administration of propofol and remifentanil was planned. Moreover, the plan was to awake the patient if emergency situations should arise. The patient was required to fast for 8 hour prior to the procedure, and amoxicillin 1.5 g PO was administered as the antibiotic. Informed consent was obtained from the patient's guardian and the consent for the case report was also obtained.
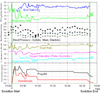
The patient was seated in a unit chair and intravenous line was accessed on her right arm. Monitoring was initiated after devices for monitoring blood pressure, oxygen saturation, heart rate, electrocardiography, and bispectral index (BIS) were attached. Oxygen was supplied through a nasal prong at a rate of 3 L/min, and capnography was performed, along with monitoring of respiratory rate and body temperature (Fig. 2).
The patient was sedated by using the target controlled infusion (TCI) method to administer propofol (Fresofol 2%, Fresenius Kabi) and remifentanil (Ultiva, GlaxoSmithKine) through an Orchestra syringe pump system.
The depth of sedation targeted deep sedation, placing the patient in a state of unconsciousness, and sedation was monitored by BIS. The effect-site concentration of propofol was maintained within a range of 1.0 µg/ml to 2.5 µg/ml, while that of remifentanil was initiated from 1.0 ng/ml and controlled not to exceed 2.0 ng/ml. The effect-site concentration of each agent was regulated according to the patient's movement and changes in oxygen saturation. Oxygen saturation was maintained at around 85% and the blood pressure was maintained between 120–90/60–40 mmHg (Fig. 3).
After 2.5 hours of sedation, she fully regained consciousness, and was discharged without any complication after 1-hour observation.
Patients with Down syndrome not only suffer from moderate mental retardation, but 40–50% of them are also born with congenital heart deformities, with congenital heart diseases such as ventricular septal defect, tetralogy of Fallot, and patent ductus arteriosus being common [4]. In addition, some patients may also present with other heart diseases, including mitral valve prolapse and aortic regurgitation, which in mild cases may go undetected since no specific symptoms can be found. In particular, even after undergoing corrective heart surgery, residual deformity may be found, which may lead to elevated pulmonary circulation and pulmonary hypertension over time, thereby increasing the risk of pulmonary congestion and heart failures during general anesthesia [5].
ES is distinguished by pulmonary hypertension with reverse right to left shunting of the blood flow. In a normal heart, the pulmonary circulation and systemic circulation are separated. Eisenmenger syndrome develops in patients with large systemic to pulmonary communications. The increased pulmonary blood flow causes progressive structural changes within the pulmonary microvasculature [6].
The reported mortality rate associated with general anesthesia for surgical purposes is 20-30% among patients with ES [7]. The most common complication during general anesthesia is hypotension [8].
According to a report by Bennett et al., hypotension occurs in approximately 26% of patients, but the prevalence of hypotension may be reduced by using vasoconstrictors [8]. Additionally, the second most common complication is reduced oxygen saturation. PVR may increase under circumstances involving hypothermia, hypoxia, hypercapnia, acidosis, positive pressure ventilation, and positive end expiratory pressure, and when PVR becomes elevated, pulmonary circulation decreases significantly, resulting in possible hypoxemia. Under such circumstances, the treatment approach should include correction of hypercarbia, hypoxia, and acidosis, along with alleviation of factors that affect pulmonary hypertension [9].
Moreover, in patients with heart deformation, such as ES, infective endocarditis can occur, and as such, administration of antibiotics is required prior to dental procedures [10], but most of all, sterile operations are needed during dental procedures.
It has been reported that repeated positive-pressure ventilation might increase the shunt flow due to a reduction in the pulmonary blood flow [11]. Therefore, the authors in this case attempted deep sedation with self-respiration by the patient instead of general anesthesia.
Among various sedation techniques, intravenous sedation has been widely used to provide deep sedation to patients with disability [12]. Especially, TCI has been widely used to titrate the intended sedative level [13]. Advances in the drug delivery techniques have permitted the development of the TCI system, with drugs delivered to reach and sustain specific target drug concentrations at the effect-site. With the assistance of the TCI system, it is possible to adjust and maintain the effect-site concentration (Ce) of drugs incorporated within the TCI system. Among the sedatives, the pharmacokinetic and pharmacodynamic (PK-PD) properties of propofol and remifentanil have been extensively investigated. With its favorable properties such as fast recovery, antiemetic effect, and fast titration, the use of propofol is increasing in the field of dentistry [14].
However, it has been frequently reported that propofol can lead to hypotension, which can be very severe due to a decrease in the systemic vascular resistance [8]. In addition, propofol suppresses the pharyngeal reflexes during sedation under spontaneous respiration [15].
Remifentanil is a powerful opioid, which is fast acting and has short active duration, and it was reported that co-administration of propofol along with remifentanil via a TCI system for the surgical extraction of impacted teeth may be safe and effective compared to propofol only administration [16].
In the case presented in this paper, the treatment of a patient with ES with severe pulmonary hypertension was scheduled for 1 hour, but exceeded 2 hours. However, by using intravenous sedation with co-administration of propofol and remifentanil, dental treatment was completed safely without any drop in blood pressure.
Figures and Tables
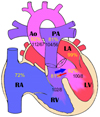 | Fig. 1After cardiac catheterization, a right-to-left shunt and severe pulmonary hypertension are observed. (Yellow numbers indicate oxygen saturation and black numbers indicate blood pressure). |
References
1. Hopkins WE. Severe pulmonary hypertension in congenital heart disease: A review of eisenmenger syndrome. Curr Opin Cardiol. 1995; 10:517–523.
2. Raines DE, Liberthson RR, Murray JR. Anesthetic management and outcome following noncardiac surgery in nonparturients with eisenmenger's physiology. J Clin Anesth. 1996; 8:341–347.

3. Kunimatsu T, Greenan S, Yamashita A, Yamamoto T, Ikeda M. Use of moderate sedation for a patient with down syndrome, intellectual disability, and eisenmenger syndrome: A case report. Spec Care Dentist. 2011; 31:41–43.

4. Pastore E, Marino B, Calzolari A, Digilio MC, Giannotti A, Turchetta A. Clinical and cardiorespiratory assessment in children with down syndrome without congenital heart disease. Arch Pediatr Adolesc Med. 2000; 154:408–410.

5. Oechslin E, Mebus S, Schulze-Neick I, Niwa K, Trindade PT, Eicken A, et al. The adult patient with eisenmenger syndrome: A medical update after dana point part iii: Specific management and surgical aspects. Curr Cardiol Rev. 2010; 6:363–372.

7. Daliento L, Somerville J, Presbitero P, Menti L, Brach-Prever S, Rizzoli G, et al. Eisenmenger syndrome. Factors relating to deterioration and death. Eur Heart J. 1998; 19:1845–1855.

8. Bennett JM, Ehrenfeld JM, Markham L, Eagle SS. Anesthetic management and outcomes for patients with pulmonary hypertension and intracardiac shunts and eisenmenger syndrome: A review of institutional experience. J Clin Anesth. 2014; 26:286–293.

9. Galie N, Manes A, Palazzini M, Negro L, Marinelli A, Gambetti S, et al. Management of pulmonary arterial hypertension associated with congenital systemic-to-pulmonary shunts and eisenmenger's syndrome. Drugs. 2008; 68:1049–1066.

10. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. Guidelines from the american heart association: A guideline from the american heart association rheumatic fever, endocarditis and kawasaki disease committee, council on cardiovascular disease in the young, and the council on clinical cardiology, council on cardiovascular surgery and anesthesia, and the quality of care and outcomes research interdisciplinary working group. J Am Dent Assoc. 2007; 138:739–745. 747–760.
11. Lumley J, Whitwam JG, Morgan M. General anesthesia in the presence of eisenmenger's syndrome. Anesth Analg. 1977; 56:543–547.

12. Manley MC, Skelly AM, Hamilton AG. Dental treatment for people with challenging behaviour: General anaesthesia or sedation? Br Dent J. 2000; 188:358–360.

13. Schwilden H, Schuttler J. Target controlled anaesthetic drug dosing. Handb Exp Pharmacol. 2008; 425–450.

14. Lee BS, Shin TJ, Kim HJ, Choi YJ, Lee SE, Chang JH, et al. Effect site concentrations of propofol for dental treatment under deep sedation in intellectually disabled patients. J Korean Dent Soc Anesthesiol. 2014; 14:167–172.

15. Kiyama S, Yoshikawa T. Target-controlled infusion of propofol for the difficult airway. Anaesth Intensive Care. 1998; 26:591–592.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download