Abstract
A 47-year-old woman was referred for surgical treatment of osteomyelitis of the mandible. She had already undergone three previous surgeries. Pre-anesthetic airway evaluation predicted a difficult airway, due to the thin, retro-positioned mandible, tongue, and atrophic changes in the lips and soft tissue. We inserted packing gauzes in the buccal mucosa for easier mask fitting and ventilation. During direct laryngoscopic intubation with a nasotracheal tube (NTT), fracture of a thin mandible can easily occur. Therefore, we used a fiberoptic bronchoscope to insert the NTT. After surgery, we performed a tongue-tie to protect against airway obstruction caused by the backward movement of the tongue during recovery. The patient recovered without any complications. We determined the status of the patient precisely and consequently performed thorough preparations for the surgery, allowing the patient to be anesthetized safely and recover after surgery. Careful assessment of the patient and airway prior to surgery is necessary.
Bone resorptive changes in the edentulous parts of the maxilla and mandible can occur due to many local and systemic factors, such as edentulousness, bite stress, tooth extraction, gender, age, hormone imbalance, and osteoporosis [1]. Resorption of the alveolar ridge influences the clinical height of the residual mandible, and the remaining tissue is insufficient for supporting denture function [2]. Conditions such as an edentulous state or a thin mandible with noncompliant soft tissue require management of a difficult airway during induction of general anesthesia [3]. We here reported our experience of difficult airway management due to a thin mandible, and atrophied muscle and soft tissue.
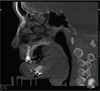
A 47-year-old female patient (158 cm, 47 kg) was admitted to the hospital with osteomyelitis of the left mandible and previous surgery for removal of a plate, and reconstruction with a plate and an iliac bone graft. The patient had undergone mandibulectomy and reconstruction with a plate and an iliac bone graft in 2000. Because of the osteomyelitis, a segment of mandibular bone from the chin to both mandibular angles had been removed. In 2005 and 2007, the same operation was repeated (Fig. 1). After these three surgeries, the patient's chin was scarred and the soft tissue was atrophied. The patient suffered from mental retardation (MR) I and hypothyroidism, and her American Society of Anesthesiologists physical status was II. There were no specific findings on preoperative laboratory tests, chest radiograph, and electrocardiogram. Her Mallampati classification score was class III. Neck mobility and mouth opening were unremarkable, because of her medical history (MR I). She denied symptoms related to obstructive sleep apnea, dysphagia, and respiratory difficulty. Based on pre-anesthetic airway evaluation, a difficult airway was predicted, due to the thin, retro-positioned mandible, tongue, and atrophic change of the lips and soft tissue (Fig. 2). Therefore, we prepared alternative devices for airway management, such as an oropharyngeal airway (OPA), laryngeal mask airway (LMA), and fiberoptic bronchoscope (FOB).
Baseline blood pressure, heart rate, and oxygen saturation were 95/40 mmHg, 75 beats/min, and 100%, respectively. The patient was pre-oxygenated with 100% oxygen before anesthesia induction. For induction, propofol 100 mg and rocuronium 40 mg were injected intravenously. After loss of consciousness and paralysis, conventional mask ventilation was difficult, due to insufficient support of the lower lip, soft tissue, and mandible, tongue depression. Thus, we used OPA for airway maintenance. Due to the repeated surgery, the patient's mandible was very thin, and we were concerned that the mandible would fracture when fitting the mask for ventilation. Additionally, there was a space between the mask and the soft tissue during mask fitting, because the soft tissue was curled into the oral cavity due to the thin mandible. Therefore, we inserted packing gauzes into the patient's buccal mucosa, which facilitated mask fitting. During direct laryngoscopic intubation with a nasotracheal tube (NTT), mandibular fracture could easily occur because of the thin mandible. Therefore, we used a FOB to insert the NTT.
After intubation, the operation was conducted without difficulty. The operation time was about 3 h. The patient recovered from general anesthesia and was extubated uneventfully. After maxillofacial surgery, we usually apply an elastic bandage around the patient's face to preventing swelling; however, in this case, we did not use an elastic bandage because of the possibility of upper airway compression, which could occur if the bandage did not have sufficient support on the OPA. In addition, a tongue-tie was performed using black silk on the tongue, to protect against airway obstruction caused by the backward curling movement of the tongue during the recovery.
The patient gave consent for this case presentation.
Change in the mandibular space and dentition caused by aging or mandibular surgery can produce airway obstruction. The aging process causes changes in oral anatomy, such as inferior movement of the hyoid bone, reduction of the pharyngeal airway space, and increase of the tongue volume [45]. An edentulous state of the mandible is troublesome due to an unfavorable tongue position. The tongue remains withdrawn into the back of the oral cavity, and the anterior part of the mouth floor is exposed, in a state considered “abnormal” [6]. Malpositioned or missing teeth, dentures, and malformation are present in cases with abnormal tongue position [7]. Patients with a small or receding mandible have a high risk for airway obstruction. Occasionally, it is accompanied by an enlarged tongue, which may cause severe airway obstruction, because the base of the tongue impinges on the airway immediately above the glottis [8]. Mandibular surgery, such as mandibulectomy, creates a similar change in the mandible, hyoid bone, and tongue position, which can cause airway obstruction.
The edentulous state of an elderly patient can complicate face mask ventilation as compared to that in young adults. A new, more flexible face mask, such as the “everseal” mask is available, which allows the mask to seal around the face [9]. However, in the absence of such a mask, there are alternative methods for sealing the face, include gauze packing into the buccal mucosa, as we did in our case, and the mandibular advancement splints used for treatment of sleep apnea [10].
We could use LMA immediately as an alternative airway management device, if the conventional mask ventilation failed in our case. Insertion of a supraglottic airway (SGA) is recommended for management of a difficult airway, according to the American Society of Anesthesiologists guidelines [11]. An observational study reported that the LMA provided successful rescue ventilation in 94.1% of patients who could not be maskventilated or intubated [12]. If both face mask and SGA ventilation become inadequate, emergency invasive airway access, such as surgical or percutaneous tracheostomy, should be considered [11]. Therefore, it is necessary to prepare laryngoscopes with a selection of blades, a variety of endotracheal tubes, stylets, flexible bougies, oral and nasal airways, a cricothyroid puncture kit, reliable suction equipment, SGA, video laryngoscopes, rigid optic laryngoscopes, and FOB, when it is anticipated that a patient will have a difficult airway [13].
In conclusion, we experienced difficult airway management due to a thin mandible and atrophied soft tissue caused by numerous surgeries. We successfully intubated the patient and completed the surgery. In order to prevent unexpected airway maintenance failure, we need to investigate the condition of the patient before surgery and consider various airway maintenance methods accordingly.
Figures and Tables
ACKNOWLEDGMENTS
This study was supported by 2015 Clinical Research Grant, Pusan National University Dental Hospital
References
1. Devlin H, Ferguson MW. Alveolar ridge resorption and mandibular atrophy. A review of the role of local and systemic factors. Br Dent J. 1991; 170:101–104.

2. Klemetti E, Vainio P. Effect of bone mineral density in skeleton and mandible on extraction of teeth and clinical alveolar height. J Prosthet Dent. 1993; 70:21–25.

3. Sunanda G, Rajesh S, Dimpel J. Airway Assessment: Predictors of Difficult Airway. Indian J Anaesth. 2005; 49:257–262.
4. Kollias I, Krogstad O. Adult craniocervical and pharyngeal changes- a longitudinal cephalometric study between 22 and 42 years of age. Part I: morphological craniocervical and hyoid bone changes. Eur J Orthod. 1999; 21:333–344.

5. Johnston CD, Richardson A. Cephlometric changes in adult pharyngeal morphology. Eur J Orthod. 1999; 21:357–362.
6. Beresin VE, Schiesser FJ. The neutral zone in complete dentures. J Prosthet Dent. 2006; 95:93–100.

7. Wright CR, Muyskens JH, Strong LH, Westerman KN, Kingery RH, Williams ST. A study of the tongue and its relation to denture stability. J Amer Dent Assoc. 1949; 39:269–275.

8. Victor LD. Obstructive sleep apnea. Am Fam Physician. 1999; 60:2279–2286.
9. Murray D, Dodds C. Perioperative care of the elderly. Contin Educ Anaesth Crit Care Pain. 2004; 4:193–196.

10. Nayar S, Knox J. Management of obstructive sleep apnea in an edentulous patient with a mandibular advancement splint: A clinical report. J Prosthet Dent. 2005; 94:108–111.

11. Apfelgaum JL, Haqberq CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013; 118:251–270.
12. Parmet JL, Colonna-Romano P, Horrow JC, Miller F, Gonzales J, Rosenberg H. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998; 87:661–665.

13. Novak-Jankovic V. Management of the difficult airway. Acta Clin Croat. 2012; 51:505–510.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download