Abstract
Background
Some patients with special needs exhibit intellectual disability, including deficits in cognitive skills and decreased quality of life. The purpose of this study was to retrospectively compare changes in body composition and hemodynamics during general anesthesia in patients with and without special needs.
Methods
The backgrounds of patients who underwent oral maxillofacial surgery under general anesthesia were recorded from medical records. Intracellular water (ICW), extracellular water (ECW), stroke volume variation (SVV), and heart rate (HR) were recorded for 3 h after the start of anesthesia. Categorical data were compared using an unpaired t-test, and a P-value of less than 0.05 was regarded as significant. Numerical data were compared using the Bonferroni correction, and a P-value of less than 0.0125 was regarded as significant.
Results
A total of 21 patients were included in the study: 10 patients without special needs (non-S-group) and 11 patients with special needs (S-group). There were no significant differences in patients' backgrounds, except with regard to height (P = 0.03). In both groups, ICW and ECW were maintained, although they were lower in the S-group compared to the non-S-group. SVV was maintained in both groups, although it was higher in the S-group than the non-S-group. HR was significantly lower in the S-group 1 h after induction of anesthesia (P < 0.003).
Approximately 5% of the population is handicapped in some manner [1]. As the average human lifespan has been lengthened by scientific progress, similarly, the life expectancy of patients with special needs, such as intellectual disability and cerebral palsy, has gradually increased due to improvements in medical care [2]. However, some of these patients still require total support in their daily lives due to health conditions, develop intellectual disability and/or physical disability [34].
At times, we observed hemodynamic instability during anesthesia induction in these patients and speculated that low food and water intake might contribute to this effect. We hypothesized that decreased body fluid might cause unexpected hypotension and arrhythmia during anesthesia induction.
In this study, we investigated the backgrounds of patients with and without special needs as well as changes in extracellular water (ECW), intracellular water (ICW), heart rate (HR), and stroke volume variation (SVV) during anesthesia.
This retrospective study was approved by The Ethics Review Board of Kyushu University Hospital (Approval No. 26-252). The study period was from October 1, 2013 until November 30, 2014. The subjects were patients who underwent oral maxillofacial or dental surgery in Kyushu University Hospital under general anesthesia. Patients with a history of cardiac, respiratory, or renal diseases or who used diuretic medications were excluded from the study. Information was extracted from medical and anesthesia records. Inclusion criteria were as follows: 5 h or less of anesthesia, 20 years of age or older, American Society of Anesthesiologists Physical Status Classification System score of ASA-PS I or II, and participated in elective surgery. The following patient background information was retrieved from medical records: diagnosis/type of special needs, gender, age, height, body weight, and body mass index (BMI). Additionally, the following information was retrieved from anesthesia records: anesthesia duration, fluid balance, and use of vasopressors. ECW, ICW, HR, and SVV data were collected for 3 h after the induction of anesthesia (induction of anesthesia = T0, 1 h after induction = T1, 2 h after induction = T2, and 3 h after induction = T3). We administered crystalloid at 8 ml/kg/h at the induction of anesthesia and at 4-6 ml/kg/h, as reference to hemodynamic changes and cardiac function during surgery, taking into consideration preoperative fluid loss and intraoperative blood loss. If excessive hypotension (systolic blood pressure < 70 mmHg) occurred, ephedrine and/or phenylephrine was intravenously administered.
The data were analyzed using JMP® 11 software (SAS Institute, Inc., Carry, NC, USA). In this study, both ECW and ICW were measured using a body composition analyzer (BioScan 920-II, MP Japan Co., Ltd., Tokyo, Japan), which can assess body fluid volume with minimal invasiveness [5]. Briefly, Bioscan obtains reproducible measurements using tetrapolar electrodes that include two current electrodes and two detection electrodes placed on the hands and feet. HR and SVV were measured using a multi-frequency impedance device (Aescuron mini®, Heiwa Bussan Co., Ltd., Tokyo, Japan), which can evaluate real-time cardiac function with minimal invasion [6].
For statistical analysis, demographic data were compared using unpaired t-tests, and a P-value of less than 0.05 was regarded as significant. ECW, ICW, HR, and SVV were compared using the Bonferroni correction, and a P-value of less than 0.0125 was regarded as significant. Results were expressed as the mean ± standard deviation (SD) or as the number of patients.
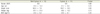
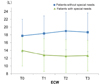
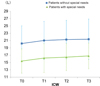
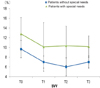
A total of 21 patients were included in the study: 10 patients without special needs (non-S-group; 5 males, 5 females) and 11 patients with special needs (S-group; 6 males, 5 females), with a mean age of 34 years old (range: 24–63 years old). There were a variety of types of special needs represented (Table 1). There were no significant differences in patients' backgrounds as noted on medical records, except that the non-S-group was significantly taller than the S-group (P = 0.03; Table 2). With regards to differences noted in anesthesia records, vasopressors (ephedrine, phenylephrine) were used by three patients in the S-group at the induction of anesthesia, but there were no significant differences in anesthesia duration or fluid balance between the groups (Table 3). In both groups, ICW and ECW was stably maintained, although they were lower in the S-group compared to the non-S-group (Figs. 1, 2). HR was significantly lower in the S-group 1 h after induction of anesthesia (T1: P < 0.003) but was unchanged in the non-S-group (Fig. 3). In both groups, SVV was maintained, although it was higher in the S-group compared to the non-S-group (Fig. 4). There were no cases of unexpected arrhythmia during anesthesia.
In this study, we hypothesized that decreased body fluid in patients with special needs might cause unexpected hypotension and arrhythmia at the induction of anesthesia. Our results showed that both ECW and ICW were lower in patients with special needs than those without for 3 h after the induction of anesthesia, although these differences were not significant. In addition, arrhythmia was not observed. With regards to body fluid volume after preoperative fasting, circulating blood volume is not decreased in healthy adults despite 10 h of fasting [7]. Body fluid was lower in patients with special needs, however. Special needs patient such as intellectual disability, autism and dementia had almost same disability in this study. They could speak a few words but could not communicate and needed support for daily activities. It is likely that they drink less water leading to chronic dehydration. They had various systemic complications, such as cerebral palsy, in addition to poor nutrition and inheritance. Therefore, they might be shorter compared to adults without special needs. SVV (9-16%) and HR (72-98 bpm) were higher in patients with special needs compared to those without, indicating a decrease in body fluid volume at the induction of anesthesia. SVV is a physiological phenomenon in which arterial pulse pressure falls during expiration and rises during inspiration due to changes in intrathoracic pressure. The normal range has been reported as 5–10 mmHg [8]. In 3 of the 11 patients with special needs, a vasopressor was administered to maintain hemodynamics at the induction of anesthesia, while vasopressors were not administered to patients without special needs. Since hemodynamics should be stably maintained throughout anesthesia, we should monitor decreases in body fluid volume, especially in patients with special needs, to avoid unexpected hypotension during anesthesia induction [9].
Devices that measure body composition, such as Doppler, are useful in many clinical situations, such as anticipated electrolyte abnormalities and hypovolemia. We used BioScan, a noninvasive, portable device that uses tetrapolar electrodes placed on the hands and feet [5]. It is also useful in severely ill patients to obtain measurements such as edema and nutritional status. Therefore, this device could help guide fluid management, resuscitation, and de-resuscitation [10]. However, it has not used for body composition monitoring during general anesthesia, and body fluid status is unknown in patients with special needs. Therefore, in this study we used this body composition analyzer during general anesthesia and postoperatively evaluated the change in body composition. We found that body fluid volume was decreased in patients with special needs compared to those without.
The limitations of this study were its retrospective design and small sample size. Further studies with larger sample sizes and monitoring of intraoperative changes in hemodynamics may be required.
In conclusion, it is important to monitor changes in hemodynamics due to body fluid imbalance especially in patients with special needs during general anesthesia.
Figures and Tables
Fig. 3
HR decreases after 1 h of anesthesia in patients with special needs. Values are mean ± SD. *P < 0.0125, Bonferroni correction. HR: heart rate; bpm: beats per minute.
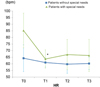
Table 1
Typesof special needs represented in this study

Table 2
Patients' backgrounds based on medical records
References
2. Messieha Z, Ananda RC, Hoffman I, Hoffman W. Five year outcomes study of dental rehabilitation conducted under general anesthesia for special needs patients. Anesth Prog. 2007; 54:170–174.

3. Lee HS, Jung HI, Kim SM, Kim J, Doh RM, Lee JH. Attitudes of Korean Dental students toward individuals with special health care needs. J Dent Educ. 2015; 79:1024–1030.

4. Dolan TA, Atchison K, Huynh TN. Access to dental care among older adults in the United States. J Dent Educ. 2005; 69:961–974.

5. Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to bed side review. Anaesthesiol Intensive Ther. 2014; 46:381–391.

6. Tomaske M, Knirsch W, Kretshmar O, Woitzek K, Balmer C, Schmitz A, et al. Cardiac output measurement in children: comparison of Aesculon® cardiac output monitor and thermodilution. Br J Anaesth. 2008; 100:517–520.

7. Jacob M, Chappell D, Conzen P, Finsterer U, Rehm M. Blood volume is normal after pre-operative overnight fasting. Acta Anaesthesiol Scand. 2008; 52:522–529.
8. Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001; 92:984–989.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download