Abstract
Infection that progresses to deep areas of the neck requires appropriate assessment of the airway, and securing of the airway is critical in patients with deep neck infection. In the patient in our case report, bilateral pneumothorax occurred while performing tracheostomy to the airways of a patient with deep neck infection, and therefore, this paper details the method used to secure the airway of patients with deep neck infection.
In patients with maxillofacial infection, an increase in severity of the infection near the airways can potentially cause airway obstruction. Infection that progresses to deep areas of the neck requires appropriate assessment of the airway, and securing of the airway is critical [1]. Therefore, for patients with deep neck infection, there are several methods for securing the airways, one of which is tracheostomy [2]. However, when tracheostomy is performed, various complications may arise [34]. In the patient in our case report, bilateral pneumothorax occurred while performing tracheostomy to the airways of a patient with deep neck infection, and therefore, this paper details the method used to secure the airway of patients with deep neck infection.
A 52-year-old man was admitted to the emergency room (ER) with a chief complaint of swelling in the right submandibular area, which was noticed a week earlier. Clinical examination revealed swelling in the right submandibular area and subglossal area. Computed tomography (CT) in the ER revealed abscesses in the right submandibular and subglossal areas (Fig. 1). At this time, the patient did not have any symptoms of breathing difficulty and did not show signs of upper airway obstruction on plain neck radiograph and neck CT imaging (Fig. 2). The patient was diagnosed the right submandibular abscess and right subglossal abscess, for which intraoral incision and drainage was performed after intravenous administration of antibiotics. The patient and his guardian were explained the possibility of airway obstruction, if symptoms deteriorated in the future, and the patient was transferred to the general ward for follow up observations for infection. The day after admission, the patient complained of mild swallowing and breathing difficulties, and his oxygen saturation level (SpO2) was 97%. Nasal cannular was used to administer 3 L/min of oxygen, and the process was monitored. However, the patient continued to experience breathing difficulties and the severity increased. After 2 hours, his vital signs were as follows: blood pressure of NIBP_SBP was 164 mmHg and NIBP_DBP 98 mmHg; pulse rate was 130 beats/min; respiratory rate was 28 breaths/min; body temperature 38. 4℃; and (SpO2) level was 97%.
The patient was consulted for airway evaluation. Partial airway obstruction was observed on endoscopic airway examination performed at the ENT department, and because the patient complained of severe breathing difficulties when lying flat in the supine position, he was instructed to maintain Semi-Fowler's position. For airway management, after discussion and consultation with the Departments of ENT and Anesthesiology, a decision was taken to secure the airway via intubation. The patient and his guardian were explained the tracheostomy procedure, possibility of an additional incision and drainage, and the patient care in the intensive care unit (ICU). After the obtaining the necessary consent, the patient was moved to the operation room (OR). During the pre-anesthetic evaluation in the OR, the anesthesiologist was of the opinion that the swelling in the oropharynx and hypopharynx regions were severe and stated that endotracheal intubation via the oral or nasal cavity would be difficult. Consequently, the ENT department was requested to perform a tracheostomy without preceding endotracheal intubation, which was to be performed under local anesthesia with oxygen being administered while the patient was in Semi-Fowler's position. In the OR, with the patient in Semi-Fowler's position and SpO2 level maintained at 99%, an ENT surgeon performed the tracheostomy. After 20 minutes from the initiation of tracheostomy, the patient suddenly showed difficulty in breathing and respiratory arrest, while his SpO2 level began to rapidly decrease, and even reaching 0%. That event took place during the lateral dissection of soft tissue including of muscles. The time taken from initiation of breathing difficulty to intubation after tracheal opening was 10 minutes after 30 minutes (min) from the incision of tracheostomy. The SpO2 level increased again once oxygen was supplied by placing a tracheal tube, but the maximum level reached was 80%, with no further increase. A right-sided pneumothorax was identified on the chest AP radiograph taken to assess the cause insufficient oxygen saturation following tracheostomy and intubation status (Fig. 3), whereas the findings on the preoperative chest radiograph were normal. The emergency thoracentesis was performed 30 minutes after identifying right-sided pneumothorax with the chest tube in the right lung region. A maxillofacial surgeon performed incision and drainage on the submandibular space through a neck and intraoral approach, after which the patient was moved to the ICU. An additional chest AP radiograph taken in the ICU, which showed a pneumothorax in the left lung region as well as right lung (Fig. 4). Thoracentesis was performed on the left lung region additionally (Fig. 5).
The patient was then in a state of stupor, and electroencephalography results indicated a mild to moderate diffused cerebral dysfunction, based on which hypoxic brain damage was diagnosed. The patient continued to show improvement and there, he underwent rehabilitative therapy with a diagnosis of quadriplegia from hypoxic brain damage. In the fifth month of hospitalization, the patient improved and was discharged. At the time of discharge, the patient showed a pattern of neural recovery, and it was recommended to the patient and his family that he actively needs to continue rehabilitation therapy to strengthen the muscles in his limbs and for his speech therapy.
In the present case, pneumothorax occurred bilaterally during tracheostomy in a patient with deep neck infection patients. During this process, hypoxic brain damage occurred, which caused quadriplegia and articulation disorder. The symptoms eventually improved, and the patient was discharged. Securing the airway must be considered first in patients with deep neck infections, and airway evaluation should be performed and the appropriate measures should be taken to secure the airway. First, it is critical to determine if the patient has any breathing difficulties in the supine position, and signs of respiratory failure should be assessed through measurements the SpO2 level as well as other vital signs. Even with a deep neck infection, conventional laryngoscopic intubation through the oral cavity should be considered first, and intubation through the nasal cavity can also be considered [5]. In cases where incision and drainage in the neck area and use of systemic antibiotics do not guarantee decrease in infection and edema in the deep neck area, tracheal intubation can be attempted during the early stages to secure the airway. However, if the patient's airway has narrowed to the point where normal intubation is not possible, then laryngoscopic intubation becomes difficult, in which case, a laryngoscopic video or fiber optic endoscopy can be used to identify the path to the bronchus and intubation can be attempted via this pathway [6]. In such cases, intubation can be performed through the nasal airways to ensure oxygen supply via this route, and the amount of carbon dioxide exhaled can be measured, while intubation can be attempted using fiber optic endoscopy through the other nasal airway while the patient is awake [7]. During the awaken intubation through the nasal cavity; tracheal intubation is attempted via the nasal airway and fiber optic endoscopy through the nasal cavity with the patient is in the sitting position, if the patient has breathing difficulties in the supine position [8]. During tracheostomy, ultrasound can be used to identify the anatomical locations of the airway and bronchus to attempt the intubation [9]. However, since infected edema can occur on the epiglottis, intubation may not be feasible. Moreover, if intubation by aforementioned methods is difficult, then oxygen can still be supplied to the patient using a laryngeal mask airway [10].
In the present case, the patient had difficulties breathing in the supine position, and consequently, tracheostomy was performed under local anesthesia with the patient in the sitting position. Various complications can occur during tracheostomy [34111213]. Pneumothorax, the complication that occurred in the present case, can affect the pulmonary function [311]. Therefore, tracheostomy should not be performed right away, but rather aforementioned tracheal intubation using ultrasonography or fiber optic endoscopy through the oral or nasal cavity should be considered and attempted first. If such attempts at intubation are unsuccessful, then tracheostomy is performed, which can lead to serious complications, as in the present case. Therefore, in such cases, the patient and patient's guardian must be explained the presenting symptoms, which necessitate tracheostomy and the possible complications that can occur. Also, above described contents should be included in the patient's consents. Considering the possibility of complications, the procedure must be performed by an experienced surgeon and surgery should prepare for tracheostomy, along with cricothyrotomy, while being ready for mandatory ventilation using oral and nasal masks [14].
Unlike the present case, if bleeding occurs inside the mouth or the neck from trauma or other emergencies, a clear field of vision in the oropharynx area cannot be secured, and therefore, the airway may be secured via emergency tracheostomy under local anesthesia with the patient in the sitting position [15]. However, the present case is that of a patient with infection, where tracheostomy was difficult due to deviation of the anatomic structures and swelling caused by the neck infection. In particular, edema in the neck area and patient in the sitting position can make tracheostomy even more difficult. Therefore, tracheal intubation via the oral or nasal cavity, which is non-invasive and has fewer complications, should be considered first and attempted.
In the present case, hypoxic brain damage occurred as a complication of tracheostomy. Although the infection in the neck area was resolved in the early stages, the patient required 5 months of in-patient care to recover from the brain damage sustained as a complication from tracheostomy. Moreover, considering that the patient was also left with a mild speech disorder and quadriplegia, it is believed that strict protocols and an experienced medical team are needed in a clinical setting to secure the airway of patients with a deep neck infection.
Figures and Tables
Fig. 1
Submandibular space abscess (star) on computed tomography (CT) imaging acquired in the emergency room. Neck CT coronal view.
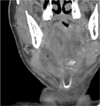
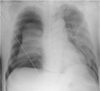
Fig. 3
The right-sided pneumothorax appearing on the chest anteroposterior (AP) radiograph acquired after tracheostomy.
References
1. Karkos PD, Leong SC, Beer H, Apostolidou MT, Panarese A. Challenging airways in deep neck space infections. Am J Otolaryngol. 2007; 28:415–418.

2. Chen SJ, Ji N, Chen YX, Zhao SJ, Xiao JR, Lin XM, et al. Management and maintenance of the airway in cervical necrotising fasciitis: a retrospective analysis of 15 cases. Br J Oral Maxillofac Surg. 2015; 53:642–646.
3. Kumar D, O'Hare B, Timon C, Mukhtar M, Kelly D. Bilateral pneumothoraces and pulmonary oedema following tracheostomy induced by acute tracheal obstruction. BMJ Case Rep. 2012; 2012.
4. Pappachan B. Acute airway distress secondary to iatrogenic injury during Tracheostomy. J Maxillofac Oral Surg. 2009; 8:91–93.

5. Yoo H, Choi JM, Jo JY, Lee S, Jeong SM. Blind nasal intubation as an alternative to difficult intubation approaches. J Dent Anesth Pain Med. 2015; 15:181.

6. Moon YJ, Kim J, Seo DW, Kim JW, Jung HW, Suk EH, et al. Endotracheal intubation by inexperienced trainees using the Clarus Video System: learning curve and orodental trauma perspectives. J Dent Anesth Pain Med. 2015; 1:207.

7. Giordano D, Panini A, Pernice C, Raso MG, Barbieri V. Neurologic toxicity of lidocaine during awake intubation in a patient with tongue base abscess. Case report. Am J Otolaryngol. 2014; 35:62–65.

8. Wolfe MM, Davis JW, Parks SN. Is surgical airway necessary for airway management in deep neck infections and Ludwig angina? J Crit Care. 2011; 26:11–14.

9. Fichtner A, Vrtny P, Schaarschmidt F. [Ultrasound-guided retrograde emergency intubation : Life-saving management of a bleeding airway emergency with unclear anatomical situation]. Anaesthesist. 2015; DOI: 10.1007/s00101-015-0102-y.

10. Kim JS, Seo DK, Lee CJ, Jung HS, Kim SS. Difficult intubation using intubating laryngeal mask airway in conjunction with a fiber optic bronchoscope. J Dent Anesth Pain Med. 2015; 15:167.
11. Kim WH, Kim BH. Bilateral pneumothoraces, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and subcutaneous emphysema after percutaneous tracheostomy -A case report. Korean J Anesthesiol. 2012; 62:488–492.
12. Lodhia JV, Ismail I, Christensen TD. Bilateral pneumothoraces in a patient with laryngeal carcinoma following tracheostomy for stridor. BMJ Case Rep. 2014; 2:2014.

13. Kundranda RM, Trochtenberg DS. Bilateral pneumothorax as a complication of changing tracheostomy tube. Tenn Med. 2003; 96:225–226.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download