Abstract
Background
Pediatric dentists face challenges when young patients require a mesiodens extraction. General anesthesia may be a burden to the child as well as the parent due to dental fears and costs. The aim of this study was to evaluate oral and intravenous sedation in the outpatient setting as a safe and effective means of managing patients who require a mesiodens extraction.
Methods
Records were reviewed retrospectively to find patients who underwent a mesiodens removal procedure from January 2013 to September 2014 in the Department of Pediatric Dentistry at Ajou University Hospital (Suwon, Gyeonggi-do, Republic of Korea). A total of 81 patients (62 male and 19 female) between 4 and 11 years of age (mean [± SD] 81.6 ± 14.1 months) were studied, with a mean weight of 22.9 ± 3.3 kg (16 kg to 30 kg). Vital signs, sedation drug dosage, and sedation time were studied.
Results
Mean doses of 63.7 ± 2.5 mg/kg chloral hydrate and 1.36 ± 0.22 mg/kg hydroxyzine were used for oral sedation. Nitrous oxide/oxygen was administrated for 40.0 ± 2.1 min. The mean dose of midazolam administered intravenously was 0.14 ± 0.06 mg/kg (2.38 ± 0.97 times). In all cases, the mesiodens was removed successfully.
Supernumerary teeth refer to the teeth in excess of the number that is normally present in both the permanent and primary dentitions [1]. The etiology of supernumerary teeth is not clearly known, although researchers hypothesize that supernumerary teeth are associated with the proliferation of dental follicular cells and a genetic predisposition [2]. Ethnically diverse studies have reported its prevalence between 0.45% and 2.2% [3]. Eighty percent to 90% of supernumerary teeth are found in the maxilla [4]. Mesiodentes (singular: mesiodens) occur more frequently in boys than in girls, with a ratio of about 2:1 [4]. Maxillary mesiodentes are present mainly in the palate [567]. In most instances, complications may occur, including disturbances in tooth eruption, diastema or axial rotation and inclination of permanent teeth, absorption of adjacent teeth, or the development of dentigerous cysts [8].
If such clinical findings are observed, the supernumerary teeth need to be extracted. However, because the surgical procedure can be a psychological burden for children, the timing of and method for extracting the teeth should be determined while considering the patient's cooperative ability and adjacent teeth development [9].
Because extracting supernumerary teeth can cause pain, a combination of intravenous midazolam plus oral and inhalation sedation for deep sedation with concomitant administration of sedative agents is being used at Ajou University Hospital (Suwon, Gyeonggi-do, Republic of Korea).
In this study, we retrospectively analyzed the records of patients who received intravenous midazolam plus oral and inhalation sedation in the Department of Pediatric Dentistry at Ajou University Hospital for mesiodens extraction. We analyzed the correlations between gender, age, type and dosage of sedative agents, administration frequency, duration of sedation, weight, and sedative agents.
The institutional review board at Ajou University Hospital approved this retrospective study. This study included 81 patients (62 male and 19 female) whose maxillary mesiodentes were removed between January 2013 and September 2014 while under sedation in the Department of Pediatric Dentistry at Ajou University Hospital.
Patients were sedated in accordance with the guidelines on sedation developed by the Korean Academy of Pediatric Dentistry [10]. After sedation was fully explained to the parents/guardians of the patients, written, informed and signed consent form was obtained as a precaution. Patients were limited to those with an American Society of Anesthesiologists physical status classification of 1 and a Mallampati airway classification of I or II. Sedation with concomitant administration of sedative agents was selected for use in pediatric patients with or without disabilities whose behavior could not be managed with conventional sedation, whose dental treatment time was expected to be shorter than 1 h, whose treatment procedure would be simple, who could breathe through the nasal cavity, and who did not have any difficulty maintaining their airway.
Chloral hydrate (Pocral®, Hanlim Pharm, Seoul, South Korea) and hydroxyzine (Ucerax®, Nextpharma SAS, France) were orally administered based on body weight. Thirty minutes after the agents were administered, patients were moved to the dentist's office. A mask and nose hood (Matrx MDM-D Digital Flowmeter, Parker, Hatfield, USA) were used for inhalation sedation. After 3 min of 100% oxygen (O2) administration, the O2 saturation was reduced by 10%/min until the nitrous oxide (N2O) concentration was 50%; that concentration was maintained. When anxiety and fear were observed in a patient, additional sedation with midazolam (Midazolam Bukwang inj®, Bukwang Pharm, Seoul, South Korea) was administered. To maintain the venous route, a 22 G or 24 G intravenous catheter was inserted in the patient's right foot and connected to a 0.9% sodium chloride solution. While monitoring the patient's condition, midazolam was slowly and intravenously administered. The clinical endpoints were when the patient's eyelids closed or the patient claimed subjective comfort and his/her speaking had gradually slowed [1112]. If additional sedation was required, it was administered at intervals of at least 5 min, after fully assessing the sedative effects.
The patients' vital signs during the treatment process were evaluated by nurses. The treatment process was evaluated before sedation and every 5 min after administration. The depth of sedation was evaluated in accordance with the relevant guidelines of Ajou University Hospital [13], and the heart rate and O2 saturation were measured using a pulse oximeter.
All analyses were conducted using SPSS statistics 22 (SPSS INC., Chicago, IL, USA). Analysis of Variance (ANOVA) was used to determine if there were any significant differences in body weight between groups according to chloral hydrate, hydroxyzine, and midazolam administration as well as N2O/O2 time. A Pearson correlation analysis was performed to test the correlations between body weight and chloral hydrate, hydroxyzine, midazolam, and N2O/O2 time. To examine the variables affecting midazolam administration, multiple linear regression analysis was performed, and statistical significance was set at P < 0.05.
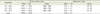
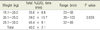
Of 81 patients, 62 were male (76.5%) and 19 were female (23.5%). Their age ranged from 4 to 11 years, with a mean age of 6.8 years (mean [± SD] 81.6 ± 14.7 months). The measured weights ranged from 16.0 kg to 29.6 kg (mean 22.9 ± 3.3 kg. In terms of the distribution by weight, 42 individuals weighed 20.1 kg to 25.0 kg, accounting for the largest proportion (51.9%). Seventeen subjects (21.0%) weighed 15.1 kg to 20.0 kg and 22 (27.1%) weighed 25.1 kg to 30.0 kg (Table 1).
The breathing pattern of subjects was regular, and a bloodstream O2 saturation (SPO2) of 98% to 100% was maintained. Midazolam was additionally administered as needed, considering the half-life of the drug and the patient response to the agent in order for the depth of sedation to be maintained at a sedation score of 4 or a level where the patient felt drowsy but could easily be aroused when speaking to him/her, tapping on his/her forehead, or making a loud sound.
The overall mean dosage of chloral hydrate was 1458 ± 244.9 mg, with 1194 ± 102.9 mg for those weighing 15.1 kg to 20.0 kg, 1438 ± 143.1 mg for those weighing 20.1 kg to 25.0 kg, and 1700 ± 248.80 mg for those weighing 25.1 kg to 30.0 kg. The overall mean dosage of hydroxyzine was found to be 31.0 ± 6.1 mg, with 24.8 ± 1.5 mg for those weighing 15.1 kg to 20.0 kg, 31.5 ± 2.69 mg for those weighing 20.1 kg to 25.0 kg, and 35 ± 2.63 mg for those weighing 25.1 kg to 30.0 kg. With increased weight, the total dosage tended to increase. No statistically significant difference between weight and oral sedative agents was found (P > 0.05) (Tables 2 and 3).
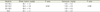
The overall mean midazolam dosage used in this study was 3.30 ± 1.34 mg, administered 2.38 ± 0.97 times, on average. Patients with a higher weight tended to require a higher number of dose administrations. No statistically significant difference between weight and mean dosage of midazolam was found (P > 0.05) (Tables 4 and 5).
N2O/O2 time was measured starting at the first titration of N2O via a mask and nose hood until the termination of titration. N2O/O2 was administered for at least 20 min up to 103 min; the mean administration time was 40.0 ± 2.1 min. Patients with a higher weight tended to have a longer total N2O/O2 time. There was a statistically significant difference between N2O/O2 time and weight (P < 0.05) (Table 6).
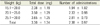
The results of correlation analyses between weight and chloral hydrate, hydroxyzine, and midazolam dosage, and N2O/O2 time showed that Pearson's coefficients for chloral hydrate, hydroxyzine, midazolam, and N2O/O2 time were 0.817, 0.574, 0.341, and 0.243, respectively (Table 7); chloral hydrate dosage had the highest correlation with weight.
When multiple linear regression analysis was performed on the 4 variables (weight, chloral hydrate, hydroxyzine, and N2O/O2 time) to analyze factors affecting midazolam administration, the results showed that hydroxyzine dosage and N2O/O2 time with a P-value of 0.05 or lower significantly affected midazolam administration, and that its explanatory power was 24.2% (Table 8).
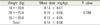
Snoring and crying were considered adverse effects if they lasted for more than 1 min. Snoring and crying were observed in 12 and 10 patients, respectively. Vomiting occurred in 1 patient during treatment, and 1 patient complained of intravenous site pain (Table 9). No patient experienced a complication after returning home.
The cause of supernumerary teeth is not definitively known, but it is clear that they are closely associated with heredity. A small number of supernumerary teeth may occur irrespective of heredity, but multiple ones are often associated with genetics [14]. In this study, intravenous sedation as an adjuvant method to oral and inhalation sedation was used to control the depth of sedation because of the invasiveness of supernumerary teeth extraction. For pediatric dental patients with or without disabilities who demonstrate low cooperation and are thus challenging to provide dental treatment to, non-pharmaceutical management may cause patients to experience a lot of stress and to resist their parents; thus, dental treatment for such patients has been performed under general anesthesia and deep sedation [15]. Allen and Sim [16] as well as Grytten et al. [17] reported patients' ages, their reasons for selecting general anesthesia, and the type of dental treatment performed for general anesthesia cases. In South Korea, Lee et al. [18] reported statistical data on dental treatments that were given under general anesthesia to 1,065 patients for 11 years.
Presently, oral sedation with chloral hydrate and hydroxyzine in combination with N2O inhalation is most commonly used for pediatric dental treatment in South Korea [19]. This method has restrictions based on the age and weight of candidates, and was reported to induce shallow sedation, which can cause patients to move frequently during the procedure, resulting in sedation failure [20]. Midazolam was reported to have a rapid onset of action and a short duration of action; its short half-life and the availability of its reversal agents made it possible to safely sedate patients [212223]. Midazolam has a very small toxicity rate, anticonvulsant, muscle-relaxant effects, and fewer effects on cardiovascular and respiratory systems [2425], and produces anterograde amnesic effects wherein patients do not remember facts such as the surgical procedure, surgical pain, or convertsations during the sustained efficacy period [2627]. To date, domestic pediatric dentists have mainly administered midazolam via submucosal, intranasal, and intramuscular routes [28]. Intravascular sedation has advantages in that it produces a rapid onset of action, offers fast recovery and easy density titration, and enables additional agents to be administered [29]. Midazolam is more water-soluble than barium; therefore, it causes less pain when given intravenously. Its elimination half-life is shorter, thus its administration may lead to faster patient discharge from the hospital following treatment [30]. Midazolam can be used as an alternative to general anesthesia in patients whose sedation with concomitant chloral hydrate and hydroxyzine is not expected to be optimal due to being overweight [31]. In this study, patients undergoing supernumerary teeth extraction who needed a sedation depth adjustment were administered intravenous midazolam in addition to the regular oral and inhalation sedation. Intravascular sedation does have disadvantages: it is necessary to secure the venous route by venipuncture, and phlebitis or hematoma may occur at the intravascular injection site [29]. In this study, 1 patient complained of pain when intravenously injected. A previous study [32] reported that Eutectic Mixture of Local Anesthetics (EMLA) 5% cream (AstraZeneca, Seoul, Korea) was applied on the skin to reduce pain when first securing a venous route and then when a venous route was secured during the procedure to successfully complete the treatment [32].
Paradoxical reactions to midazolam are the main cause of intravenous sedation failure: these reactions include hostility, anger, violence, agitation, restlessness, and violent behavior [2433]. The incidence rate of paradoxical reactions to midazolam varies from about 10.2% to 29%, and is reported to occur mainly in children and elderly people [20]. In this study, crying was observed in 10 patients (12.3%). Ten of 12 patients who snored were found to have a history of rhinitis. The observed adverse effects occurred during the entire treatment procedure, so we could not determine if all of them were associated with midazolam administration. However, it will be necessary to investigate correlations between the agent and adverse effects through further related studies.
In this study, body weight was found to have the highest correlation with chloral hydrate. For sedating patients, oral administration was the main treatment method, which conforms with the purpose of intravenous midazolam administration as an adjuvant option.
Hydroxyzine dosage and N2O/O2 time were found to have significant effects on midazolam administration. In this study, hydroxyzine was used to manage the synergistic effects of agents, nausea, and vomiting [34]. As the dosage of hydroxyzine is increased for patients with a tendency for vomiting or high anxiety levels, the dosage of midazolam can be increased at the same time. Studies about the effects of hydroxyzine dosage on midazolam administration are still lacking, so more studies need to be conducted. N2O/O2 time was prolonged as midazolam was increasingly and additionally administered to maintain the desired depth of sedation. As the difficulty of supernumerary teeth extraction increases, the time required for the related surgery may become longer. Therefore, to increase the time available for the treatment procedure, additional midazolam administration and a prolonged N2O/O2 time will be required. The explanatory power of the analysis was found to be 24.2%, so there are limitations to this interpretation. Furthermore, research on the exact procedure time and dosage of the agents is lacking, so related studies need to be conducted.
The currently recommended mean dosage of midazolam for intravenous sedation is 0.05 mg/kg to 0.1 mg/kg [31]. In this study, the depth of sedation was adjusted while midazolam was administered intravenously at a dose of 0.13 mg/kg to 0.15 mg/kg range; midazolam was titrated based on its elimination half-life, which is considered to be within the standard allowable dosage. Even though oral midazolam as an oral syrup preparation (Versed Syrup, Roche Laboratories, Inc., Nutley, USA) is available, it is not commercially available in South Korea; therefore, attempts have been made to administer intravenous midazolam with sugar syrup [35]. A study reported that when midazolam is given orally, the dose should be approximately 2 to 3 times higher than the intravenous dose [30]; thus, the administration of midazolam via the intravenous route, which enables titration, is thought to be safer.
Continuous efforts are required to enhance quality for safer sedation. Sedation requires intensive monitoring for early signs of hypoventilation or respiratory depression in children, and because respiratory depression is associated with midazolam dosage, the standard dosage should be administered [3536]. The personnel responsible for sedation as well as the sedation inspector at Ajou University Hospital are required to complete sedation training as well as cardiopulmonary resuscitation training every 2 years, which is consistent with the essential medical practitioner requirements for conducting sedation. Various agents were administered to the subjects of this study, making it difficult to distinguish the characteristics of a particular agent. In-depth studies of agents compared with a control group are necessary. Because midazolam can induce deep sedation in patients, the safety and efficacy of the agent should be investigated at every treatment phase and every administration by means of various monitoring devices. Training for coping with complications is also needed. After dental treatment, patient and parent/guardian satisfaction with sedation should be surveyed and the patients' psychological state analyzed. When the scope of sedation using intravenous midazolam in combination with oral and inhalation sedation is expanded to other dental treatment areas, we believe that it may provide patients with a high-quality treatment option and scope.
In this study, we analyzed the concomitant administration of oral and inhalation sedation along with intravenous sedation in 81 patients 4 to 11 years of age who underwent maxillary mesiodens removal. Chloral hydrate and hydroxyzine were administered as oral sedative agents, and midazolam was used as an intravenous sedative agent. The mean dosage of intravenous midazolam was 3.30 ± 1.34 mg (0.14 ± 0.06 mg/kg), and it was administered a mean of 2.38 ± 0.97 times. The mean N2O/O2 time was 40.0 ± 2.1 min. Hydroxyzine dosage and N2O/O2 time were found to significantly affect midazolam administration. Complications were observed in 24 subjects (29.6%), and all mesiodentes were successfully removed.
Intravenous sedation with midazolam can be used as an alternative to general anesthesia during mesiodens extraction and can also be used during treatment for dental caries. Because the intravenous route induces deep sedation, protocols for appropriate patient selection and monitoring as well as training on how to deal with complications are needed. Further studies investigating the optimal intravenous midazolam dosage for sedation in pediatric patients are necessary.
Figures and Tables
Table 7
Correlation of weight with chloral hydrate, hydroxyzine, midazolam, and nitrous oxide (N2O)/oxygen (O2) time

References
1. Casamassimo PS, Fields HW, McTigue DJ, Nowak A. Pediatric dentistry: infancy through adolescence. 5th ed. St Louis: Elsevier Health Sciences;2013. p. 54.
2. Kim SG, Lee SH. Mesiodens: a clinical and radiographic study. J Dent Child (Chic). 2003; 70:58–60.
3. Leco Berrocal MI, Martín Morales JF, Martínez Gonzlez JM. An observational study of the frequency of supernumerary teeth in a population of 2000 patients. Med Oral Patol Oral Cir Bucal. 2007; 12:E134–E138.
4. Gallas MM, Garcia A. Retention of permanent incisors by mesiodens: a family affair. Br Dent J. 2000; 188:63–64.

5. American Academy of Pediatric Dentistry. Guideline on management of the developing dentition and occlusion in pediatric dentistry. Pediatr Dent. 2014; 36:251–263.
6. Russell KA, Folwarczna MA. Mesiodens - diagnosis and management of a common supernumerary tooth. J Can Dent Assoc. 2003; 69:362–366.
7. Primosch RE. Anterior supernumerary teeth - assessment and surgical intervention in children. Pediatr Dent. 1981; 3:204–215.
8. Tyrologou S, Koch G, Kurol J. Location, complications and treatment a retrospective study of Mesiodentes in children. Swed Dent J. 2005; 29:1–9.
9. American Academy of Pediatric Dentistry. Guideline on Pediatric Oral Surgery. Pediatr Dent. 2014; 36:276–283.
10. Kim SO, Kim JS. Introduction of sedation guidelines and need for sedationist. J Korean Acad Pediatr Dent. 2012; 39:314–324.

11. Rodrigo MR, Rosenquist JB. Effect of conscious sedation with midazolam on oxygen saturation. J Oral Maxillofac Surg. 1988; 46:746–750.

12. Jung SH, Baik SH, Roh HK, Kang N, Im JJ, Lee BH, et al. A multicenter retrospective study of outpatient intravenous sedation for dental treatments. Maxillofac Plast Reconstr Surg. 2009; 31:394–340.
13. Jang HY, Jung JH, Kyong YY, Kim KH, Kim DK, Kim MR, et al. Korean guidelines for pediatric procedural sedation and analgesia. J Korean Soc Emerg Med. 2012; 23:303–314.
15. Nathan JE. Behavioral management strategies for young pediatric dental patients with disabilities. ASDC J Dent Child. 2001; 68:89–101.
16. Allen GD, Sim J. Full mouth restoration under general anesthesia in pedodontic practice. J Dent Child. 1967; 34:488–492.
17. Grytten J, Holst D, Dyrberg L, Faehn O. Some characteristics of patients given dental treatment under general anesthesia. Acta Odontol Scand. 1989; 47:1–5.

18. Lee DW, Song JS, Choi HJ, Kang JW, Lee JH. A survey of dental treatment under outpatient general anesthesia in department of pediatric dentistry and clinic for disabled at Yonsei university dental hospital. J Korean Acad Pediatr Dent. 2010; 37:65–72.
19. Houpt M. Project USAP 2000 - use of sedative agents by pediatric dentists: a 15-year follow-up survey. Pediatr Dent. 2002; 24:289–294.
20. Jeon JY, Jung SH, Lee BH, Im JJ, Hwang KG, Shim KS, et al. Paradoxical reaction to midazolam used in intravenous sedation for dental treatment - report of a case and review of the literature. J Korean Dent Soc Anesthesiol. 2009; 9:104–107.

21. Chi SI, Kim JS. Effects of midazolam with sevoflurane insufflation sedation on concomitant administration in pediatric patients: a preliminary study. J Korean Acad Pediatr Dent. 2014; 41:283–291.

22. Malamed SF. Sedation: a guide to patient management. 5th ed. St Louis: Mosby;2010. p. 52–54. p. 97–4421.
23. Payne K, Mattheyse FJ, Liebenberg D, Dawes T. The pharmacokinetics of midazolam in paediatric patients. Eur J Clin Pharmacol. 1989; 37:267–272.

24. O SR. Paradoxical reactions following intravenous midazolam in patients with severe anxiety for dental treatment, a case report. J Korean Dent Soc Anesthesiol. 2009; 9:30–35.

25. Khanderia U, Pandit SK. Use of midazolam hydrochloride in anesthesia. Clin Pharm. 1987; 6:533–547.
26. Ghoneim MM, Mewaldt SP. Benzodiazepines and human memory: a review. Anesthesiology. 1990; 72:926–938.

27. Clark WG, Brater DC, Johnson AR, Goth A. Goth's medical pharmacology. 13th ed. St. Louis: Mosby;1992. p. 233–284.
28. Yang YM, Shin TJ, Yoo SH, Choi SC, Kim JY, Jeong TS. Survey of sedation practices by pediatric dentists. J Korean Acad Pediatr Dent. 2014; 41:257–265.

30. Kupietzky A, Houpt MI. Midazolam: a review of its use for conscious sedation of children. Pediatr Dent. 1993; 15:237–241.
31. Lee JS, Kim JS, Kim SO. Intravenous sedation with midazolam. J Korean Assoc Disabil Oral Health. 2006; 2:142–146.
32. Lee EH, Kim SO, Kim JS, Yoo SH. Converting from oral sedation to intravenous sedation using topical anesthetics on skin after oral sedation failure. J Korean Acad Pediatr Dent. 2010; 37:213–217.
33. Manley MCG, Skelly AM, Hamilton AG. Dental treatment for people with challenging behaviour: general anaesthesia or sedation? Br Dent J. 2000; 188:358–360.

34. Ghajari MF, Golpayegani MV, Bargrizan M, Ansari G, Shayeghi S. Sedative effect of oral midazolam/hydroxyzine versus chloral hydrate/hydroxyzine on 2-6 year-old uncooperative dental patients: a randomized clinical trial. J Dent (Tehran). 2014; 11:93–99.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download