Abstract
Long QT syndrome (LQTs) is a rare congenital disorder of the heart's electrical activity. Patients with LQTs are at increased risk of developing fatal ventricular arrhythmias. Elevated levels of sympathetic stimulation can exacerbate this risk. Successful behavior management is indispensable in the treatment of patients with LQTs. However, many drugs involved in pharmacologic behavior management are known to adversely affect the QT interval. Therefore, careful selection of a sedative drug is essential in avoiding such incidences. A 10-year-old boy with a known diagnosis of LQTs required restorative treatment due to dental caries at the permanent molar. He required sedation since treatment was painful and dental phobia can trigger sympathetic stimulation, creating a dangerous situation for patients with LQTs. Therefore, the treatment was performed over two sessions under moderate sedation involving propofol combined with nitrous oxide. Restorative treatment was successful without any complications under sedation with a target-controlled infusion (TCI) of propofol. There was no significant QT prolongation during pulpal treatment. Propofol TCI may be a good candidate for sedation in patients with LQTs.
Long QT syndrome (LQTs) is a congenital disorder caused by defective ion channels that result from genetic mutation. Patients present with an increased QT interval on electrocardiogram (ECG). This condition is related to delayed ventricular repolarization, which can lead to syncopal episodes and sudden death due to ventricular arrhythmia. Increased sympathetic stimulation results in further prolongation of ventricular repolarization, which in turn prolongs the QT interval [1]. An increased QT interval creates the possibility of ventricular depolarization when the ventricle is still in its repolarized state. This condition can lead to fatal arrhythmias, and cardiac arrest may occur in severe cases.
Anxiety related to dental procedures results in stimulation of sympathetic activity. Sympathetic activation can be further exacerbated by the administration of epinephrine in local anesthetic agents. Dental phobia, painful stimuli, and lengthy treatment times can all induce a stress response in patients, a response that may be more easily induced in pediatric patients. Theoretically, pediatric patient with a behavior management problem, sympathetic stimulation due to dental phobia, in addition to the use of a local anesthetic agent containing epinephrine, could prolong the QT interval, predisposing the patient to ventricular arrhythmias. In such patients, appropriate sedation techniques may help in achieving dental treatment, reducing the incidence of fatal complications.
In this case report, restorative dental treatment under moderate sedation with propofol target-controlled infusion (TCI) combined with nitrous oxide is presented. Propofol TCI provided an effective measure to titrate sedation level during the dental procedure, while nitrous oxide (N2O) gas controlled pain by through its relative analgesic effect. In our case, no significant prolongation of the QT interval was observed.
The patient was a 10-year-old boy when dental treatment under moderate sedation was first planned. He had a medical history of a sudden cardiac arrest during separation surgery for syndactyly, from which he had been rescued by immediate cardioversion. He had received a diagnosis of long QT syndrome. The QT interval of the patient was prolonged above the normal range in an electrocardiogram (ECG) (Fig. 1). He had been taking beta-blockers (Atenolol) as a routine medication.
At a regular visit, ICDAS 5-6/+ (www.icdas.org) mesial proximal dental caries at the right mandibular permanent first molar and ICDAS 4/+ caries at the right maxillary permanent first molar were observed. The right mandibular first molar tooth was thought to require endodontic treatment (Fig. 2). Profound local analgesia must be achieved before endodontic treatment because the treatment is often very painful and uncomfortable. Emotional stress can also induce arrhythmia in patients with long QT syndrome, therefore treatment under sedation was planned. On the day of the treatment, we first administered N2O at a concentration of 40 vol % before intravenous cannulation. We attached a bispectral index (BIS) sensor to his forehead. Propofol was infused with a computer-controlled drug delivery system after intravenous cannulation. We adjusted the propofol effect-site concentration to maintain a BIS value in the range of 70-80. The effect-site concentration of propofol was maintained in the range of 0.6-1.2 µg.ml-1 during the treatment period. There was no fatal arrhythmia during propofol sedation. Composite resin restoration of the right maxillary first permanent molar and an endodontic treatment on the right mandibular first permanent molar were successfully performed under propofol sedation. Local anesthesia was achieved with lidocaine without epinephrine.
About 10 months after the first sedation, new dental caries of ICDAS 2-3/+ (www.icdas.org) were observed on all second permanent molar, all of which required restorative dental treatment (Fig. 3). The lesions seemed to involve mostly the enamel and only minimally involved the dentin, making the procedure uncomfortable rather than painful to the patient. Considering his age, we assumed that the treatment would require minimal local anesthesia if we could gain the cooperation of the patient. However, he turned out to be very uncooperative when it came to opening his mouth large enough for a dental treatment to proceed. He was also unable to bear the height of the clamp that made his mouth open non-voluntarily. Therefore, due to the posterior position of the second molars and the uncooperative nature of patient when it came to mouth opening, dental treatment without sedation was very difficult. On the day of the treatment, we transferred him to the dental unit chair and administered N2O at a concentration of 40 vol %. A BIS sensor was attached to his forehead. After intravenous cannulation was achieved, TCI of propofol was performed. An effect-site concentration of propofol was The effect-site concentration of propofol was maintained in the range of 0.7-1.4 µg.ml-1 during the treatment period to maintain a BIS value of 70-80, close to that used in the previous sedation. Ventricular arrhythmia did not occur during the propofol infusion. Furthermore, there was no significant QT prolongation during pulpal treatment. All four second molars were successfully restored by PRR (preventive resin restoration) technique with the use of a rubber dam. The patient and his parents were all satisfied with the results of the treatment. There were no complications during the perioperative period.
Long QT syndrome is an inherited disorder of the heart characterized by delayed ventricular repolarization. The name of this syndrome was derived from the characteristic electrocardiogram feature: an abnormally increased QT interval. Several subtypes of the disorder are known, each with a mutation at a specific gene locus. The affected genes usually code for ion channels that are involved in depolarization and repolarization of the ventricle. The defective channels show altered function, resulting in abnormal electrical activity of the heart. Several ions, i.e. sodium, potassium and calcium, are crucial in generating a heart rhythm. The majority of patients with LQTs carry defective potassium channels, but sodium and calcium channels are involved in other subtypes [2]. The patient in this case was confirmed to have L type calcium gene mutation, which is categorized as LQTs type 8 or Timothy syndrome. This rare subtype of LQTs, inherited in an autosomal dominant fashion, is most well described by concurrent occurrence of long QT syndrome with syndactyly [3]. Patients are usually roundfaced and bald at birth, which was evident from the past medical record of the patient. In addition, they are known to possess relatively small teeth, but this was not apparent in this case. Patients are generally under increased risk for torsades de pointes, which can cause ventricular arrhythmias and lead to sudden cardiac death. Therefore, the treatment goal for LQTs is to control fatal arrhythmias.
Since the disorder arises from altered timing of ventricular repolarization, any drug that may interfere with ion channels could theoretically either prevent or exacerbate ventricular arrhythmias. In some cases, symptoms are not apparent before administration of certain drugs, and these patients are further categorized as having drug-induced LQTs [4]. However, genetic susceptibility is the main cause of LQTs. Epinephrine, one of the most common adrenergic drugs, is routinely used in dental clinics because it is contained in commercially available lidocaine preparations. Epinephrine increases the duration of local anesthesia and its analgesic effect by constricting blood vessels. This has led to lidocaine with epinephrine being a principle choice for local anesthesia as long as epinephrine is not contraindicated. However, in patients with LQTs, epinephrine is contraindicated due to its adrenergic activity, which may put the patient at increased risk of developing a potentially fatal ventricular arrhythmia. Therefore, other measures to relieve pain should be seriously considered in LQTs patients. The stress response can further act as an adrenergic stimulant. Stress management and care in using drugs, are both important in patients with LQTs. Consequently, sedation could be very useful in patients with LQTs when effective pain control and stress management are needed.
The selection of sedative medications for patients with LQTs should be given careful consideration, because prolongation of the QT interval induced by certain sedatives may cause life-threatening complications during operative procedures. Inhalational anesthetics, such as halothane, enflurane, and sevoflurane, are associated with prolongation of the QT interval. Therefore, clinicians should be cautious when inhaled anesthetics are used for sedation of LQTs patients. Among the inhaled anesthetics, N2O, widely used for dental sedation, is known to have very little effect on the QT interval [5]. Given that patients with LQTs may suffer from inadequate pain control during dental procedures, thus inducing a sympathetic stress response, N2O could be effective in sedating and providing pain control for patients with LQTs for dental procedures. As previously mentioned, it is advisable to use local anesthetics without epinephrine for local anesthesia because of the possibility of arrhythmia in LQTs patients. N2O has the further benefit of being less likely to induce fatal arrhythmias when used for sedation because its effect on QT prolongation is minimal.
In this case, we successfully sedated a patient with LQTs under moderate sedation with propofol. Propofol has been in use for procedural sedation in the field of pediatrics for some time. Its fast onset and offset make it a suitable agent for procedural sedation in outpatient settings. Moreover, propofol can be administered with the use of a computer-controlled syringe pump. Its pharmacokinetic and pharmacodynamic characteristics have been extensively investigated, making it possible to keep its effect at the desired level using its effect site concentration through inverse modeling technique. In this case, we administered propofol with an effect site concentration ranging from 0.6-1.4 µg.ml-1 depending on the patient's hypnotic state, as guided by the BIS values. His hypnotic state was easily and stably maintained at a moderate sedation level (BIS ranging from 70 to 80) by titrating the propofol effect site concentration. We maintained a moderate level of sedation with TCI of propofol without developing any subtype of complications. This may be explained by the TCI which enabled us to titrate the effect site concentration as a surrogate measure of the drug effect directly.
The literature regarding propofol and the QT interval is conflicting, with the effect of propofol on the QT interval appearing to be equivocal [67]. It has been shown both that propofol can prolong the QT interval,[8] and that propofol can decrease the QT interval [9]. In our case, we measured QT intervals with ad-hoc ECG analysis. However, the QT interval of the patient did not show any signs of prolongation during treatment under sedation. We administered propofol at a low concentration to maintain a moderate level of sedation rather than to induce an anesthetic state. Although no randomized clinical trial regarding the dose-dependent effects of propofol on QT prolongation exists, propofol may have little effect on the QT interval when used at low doses for sedation.
In this case, restorative dental treatment of a patient with long QT syndrome was successfully completed with TCI of propofol combined with N2O without any perior postoperative complications. In conclusion, use of this sedation technique in patients with long QT syndrome during restorative dental treatment may be considered as a beneficial treatment tool.
Figures and Tables
Fig. 1
Preoperative electrocardiogram. The corrected QT interval was 550 msec, significantly higher than the normal value in males (below 430 msec).
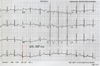
Fig. 2
Intraoral radiographs of the mandibular first permanent molar. The caries lesion is very extensive and close to the pulp. A periapical lesion has not yet developed, but it was still hard to exclude the possibility of an endodontic treatment.

Fig. 3
Intraoral photographs of the mandibular first permanent molars before and after treatment. Note that the mandibular first permanent molar, which had been endodontically treated, is restored with an adult stainless steel crown. (a) Occlusal caries of the lower right second molar are shown. (b) The carious lesion was restored with composite resin. (c) Occlusal caries of the lower left second molar are shown. (d) The lesion was also restored with composite resin.

References
1. Shimizu W, Ohe T, Kurita T, Shimomura K. Differential Response of QTU Interval to Exercise, Isoproterenol, and Atrial Pacing in Patients with Congenital Long QT syndrome. Pacing Clin Electrophysiol. 1991; 14:1966–1970.

2. Hedley PL, Jørgensen P, Schlamowitz S, Moolman-Smook J, Kanters JK, Corfield VA, Christiansen M. The genetic basis of long QT and short QT syndromes: a mutation update. Hum Mutat. 2009; 30:1486–1511.

3. Krause U, Gravenhorst V, Kriebel T, Ruschewski W, Paul T. A rare association of long QT syndrome and syndactyly: Timothy syndrome (LQT 8). Clin Res Cardiol. 2011; 100:1123–1127.

4. Curry TB, Gaver R, White RD. Acquired long QT syndrome and elective anesthesia in children. Paediatr Anaesth. 2006; 16:471–478.

5. Kies SJ, Pabelick CM, Hurley HA, White RD, Ackerman MJ. Anesthesia for Patients with Congenital Long QT Syndrome. Anesthesiology. 2005; 102:204–210.

6. Whyte SD, Booker PD, Buckley DG. The Effects of Propofol and Sevoflurane on the QT Interval and Transmural Dispersion of Repolarization in Children. Anesth Analg. 2005; 100:71–77.

7. Hume-Smith HV, Sanatani S, Lim J, Chau A, Whyte SD. The Effect of Propofol Concentration on Dispersion of Myocardial Repolarization in Children. Anesth Analg. 2008; 107:806–810.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download