Abstract
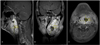
A 47-year-old man was referred to the operating room to treat a dentigenous cyst of the mandibular bone. Initial assessment of the airway was considered normal. However, after the induction of anesthesia, we could not intubate the patient due to severe distortion of the glottis. Fiberoptic bronchoscopy and video laryngoscopy were not effective. Intubation using a retrograde wire technique was successful. After the conclusion of surgery, the patient recovered without any complications. Subsequent magnetic resonance imaging of the patient's neck showed a 6 × 4 × 8.6 cm heterogeneous T2 hyperintense, T1 isointense well-enhancing mass in the prestyloid parapharyngeal space. The patient was scheduled for excision of the mass. We planned awake intubation with fiberoptic bronchoscopy. The procedure was successful and the patient recovered without complications. Anesthetic induction can decrease the muscle tone of the airway and increase airway distortion. Therefore, careful airway assessment is necessary.
Parapharyngeal space tumors account for 0.5% of all head and neck neoplasms and schwannoma is the most common type [1]. These tumors can present as either a bulging mass of the oropharynx or a cervical mass with symptoms such as pharyngeal discomfort, foreign body sensation, dysphagia, hoarseness, obstructive sleep apnea, and hypernasality [1]. Patients may be difficult to ventilate and/or intubate, but sometimes the symptoms and signs of such tumors are subtle and go unnoticed before the induction of anesthesia. We experienced difficult airway management due to a parapharyngeal mass and would like to report this case with a review of the relevant literature.
A 47-year-old male patient weighing 70 kg with a height of 173 cm was scheduled for enucleation of a dentigenous cyst of the mandibular bone (Fig. 1). The patient's medical and surgical history was unremarkable, with an American Society of Anesthesiologists (ASA) physical status of I. His laboratory findings were routine and his Mallampati classification score was class 2. His neck mobility and mouth opening were also unremarkable. He had a roughly 3 × 3 cm sized elevation in the left submandibular area; however, this was not taken seriously. He denied symptoms related to obstructive sleep apnea, dysphagia, and respiratory difficulty.
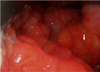
After applying standard monitoring, anesthesia was induced with intravenous fentanyl (100 µg), lidocaine (60 mg), propofol (120 mg), and rocuronium (50 mg). After mask ventilation, a lubricated right angle endotracheal tube was inserted via the right nostril and direct laryngoscopy was attempted, which showed a severely distorted glottis (Fig. 2). We then tried direct laryngoscopy with a C-MAC® videolaryngoscope (KARL STORZ Endoscopy-America, Inc., El Segundo, CA, USA), but we could only see the tip of the epiglottis without the vocal cords and a severely distorted larynx. Next, we tried to guide a fiberoptic bronchoscopy tube under the aid of the C-MAC® videolaryngoscope, but this was not effective because of the distortion of the glottis as well as bleeding from the oral cavity and epistaxis. We then attempted retrograde wire intubation with the guide wire of a central venous catheter set. We punctured the cricothyroid membrane with an 18 G intravenous needle and inserted an 18 G Teflon catheter after confirming the aspiration of air. We inserted the guide wire via the catheter under the aid of video laryngoscopy and were able to guide the wire to the right nostril. Then, we intubated using a 6.5 mm internal diameter right angle endotracheal tube over the guide wire. However, the length of the right angle endotracheal tube was too long and we could not grab the tip of the guide wire at the end of the tube. Thus, we had to guide the tube with the guide wire and fiberoptic bronchoscope until we could see the vocal cords with the fiberoptic bronchoscope at the tip of the endotracheal tube in order to insert the tube successfully. After confirming the proper position of the endotracheal tube with fiberoptic bronchoscopy, the guide wire was removed. Anesthesia was maintained with oxygen, medical air, sevoflurane, and intermittent boluses of rocuronium. After surgery, the patient recovered uneventfully.
On the first postoperative day, magnetic resonance imaging of the head and neck area showed a mass of about 6 × 4 × 8.6 cm in size in the left prestyloid parapharyngeal space (Fig. 3). One month later, the patient was scheduled for tumor excision under general anesthesia. We planned awake fiberoptic bronchoscopy with guided intubation. The patient was premedicated with an intravenous injection of 0.2 mg glycopyrrolate 10 minutes before anesthetic induction. Before the intubation procedure, the patient was mildly sedated with an intravenous infusion of dexmedetomidine. After topical anesthesia with 4% lidocaine spray, nasal packing was performed with a cotton swab soaked with 4% lidocaine and 1:10,000 phenylephrine solution. Superior laryngeal nerve block was performed with a 2% lidocaine injection and translaryngeal anesthesia was administered with 4 ml of 4% lidocaine injection through the cricothyroid membrane. Awake fiberoptic bronchoscopy was performed and a 6.5-mm internal diameter reinforced endotracheal tube was successfully intubated without specific event. After intubation, general anesthesia was induced with an intravenous injection of propofol (120 mg) and rocuronium (50 mg) and continued with 7 vol% of desflurane. Surgery time was about 2 hours and the patient recovered from general anesthesia and was extubated uneventfully. The tumor was diagnosed as a schwannoma. The patient was discharged on the fourth postoperative day without any complications.
The present case highlights several issues. First, evaluation of a patient's airway should always be performed thoroughly and carefully. In this case, we did not expect a difficult airway. The result of airway assessment was not specific and bag-mask ventilation was adequate. We did not notice any bulging mass in the oropharynx during airway assessment, and there was no distortion of the larynx at neck level when the outside of the neck was evaluated. However, if we had palpated the mass in the submandibular area thoroughly and considered computed tomography of the head and neck, we would have expected the possibility of airway difficulty.
Second, surgeons should be well trained in airway management techniques in order to cope with unexpected difficult airways. In the current case, techniques that access the airway from the mouth failed but retrograde wire intubation was successful [2]. Even fiberoptic bronchoscopy under the guidance of a video laryngoscope was unsuccessful. If we had not considered the retrograde technique, we would have needed to create a surgical airway or wake up the patient. Fortunately, bag-mask ventilation was adequate and we had more options in this case. If bag-mask ventilation had failed, then a surgical airway would have been the only option. Shina et al. reported successful intubation in an 11-year-old pediatric patient [3]. In an initial surgery, they failed to intubate the patient with a GlideScope® videolaryngoscope (Saturn Biomedical Systems, Burnaby, BC, Canada) and used direct laryngoscopy assisted by fiberoptic bronchoscopy. However, in a second surgery, they successfully intubated the patient with a C-MAC® videolaryngoscope. They considered that the differences between the surgeries were caused by differences in blade design between the two types of videolaryngoscope used. This suggests that alternative, less common, equipment should always be available to surgeons.
The retrograde technique has advantages over other airway management methods [2]. It is less invasive than a tracheostomy or other surgical airway methods. It can be performed with minimal equipment; we used a regular central venous catheterization set. It can be used in awake, sedated, obtunded, or apneic patients when other methods have failed [2,4]. In addition, this technique can facilitate fiberoptic bronchoscopy without increasing complications. The guide wire can be inserted through the working channel of a fiberoptic bronchoscope and guide the bronchoscope directly to the vocal cords [2]. A 150 cm long guide wire can be used with this method. In our case, the guide wire for central line insertion was 60 cm long and we did not insert it through the working channel. However, the guide wire still guided the endotracheal tube to the vocal cords effectively.
Third, awake intubation is indicated when assessment of airway management considers there to be a risk of 'cannot ventilate' and/or 'cannot intubate'. In the present case, fiberoptic bronchoscopy assisted intubation failed in the first surgery, but during the second surgery, we tried awake fiberoptic bronchoscopy and successfully intubated the patient without any difficulty. The distortion of the larynx was not as severe during the second surgery as during the first intubation. We believe that the muscle tone of the airway was intact during the second intubation, and so the airway distortion was less severe.
In conclusion, we experienced difficult airway management due to severe airway distortion caused by a parapharyngeal schwannoma and successfully intubated the patient with retrograde intubation and awake fiberoptic intubation. Proper airway assessment and the practice of various airway management methods are very important in order to prevent unexpected failure of airway management.
Figures and Tables
References
1. Varoquaux A, Fakhry N, Gabriel S, Garcia S, Ferretti A, Chondrogiannis S, et al. Retrostyloid parapharyngeal space tumors: a clinician and imaging perspective. Eur J Radiol. 2013; 82:773–782.

2. Bissinger U, Guggenberger H, Lenz G. Retrograde-guided fiberoptic intubation in patients with laryngeal carcinoma. Anesthesia and analgesia. 1995; 81:408–410.

3. Sinha R, Rewari V, Varma P, Kumar A. Successful use of C-Mac video laryngoscope in a child with large parapharyngeal mass. Paediatr Anaesth. 2014; 24:531–533.

4. Gonzalez Enguita R, Obon Monforte H, Romagosa i, Gomez Agraz JL. [Heart arrest during fibrobronchoscopic intubation in a patient with parapharyngeal space neoplasia]. Revista espanola de anestesiologia y reanimacion. 2003; 50:409–413.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download