Abstract
Background
We hypothesized that ketamine, when administered as the anesthetic induction agent, may prevent cardiovascular depression during high-dose remifentanil administration, unlike propofol. To test our hypothesis, we retrospectively compared the hemodynamic effects of ketamine, during high-dose remifentanil administration, with those of propofol.
Methods
Thirty-eight patients who underwent oral surgery at the Nagasaki University Hospital between April 2014 and June 2015 were included in this study. Anesthesia was induced by the following procedure: First, high-dose remifentanil (0.3-0.5 µg/kg/min) was administered 2-3 min before anesthesia induction; next, the anesthetic induction agent, either propofol (Group P) or ketamine (Group K), was administered. Mean arterial pressure (MAP) and the heart rate were recorded by the automated anesthesia recording system at four time points: immediately before the administration of high-dose remifentanil (T1); immediately before the administration of propofol or ketamine (T2); 2.5 min (T3), and 5 min (T4) after the administration of the anesthetic induction agent.
Results
In Group P, the MAP at T3 (75.7 ± 15.5 mmHg, P = 0.0015) and T4 (68.3 ± 12.5 mmHg, P < 0.001) were significantly lower than those at T1 (94.0 ± 12.4 mmHg). However, the MAP values in the K group were very similar (P = 0.133) at all time points. The heart rates in both Groups P (P = 0.254) and K (P = 0.859) remained unchanged over time.
Remifentanil is an ultra-short-acting µ-opioid for use not only during general anesthesia, but also during sedation. High-dose remifentanil administration during anesthesia induction is a popular technique to prevent the stimulation of the trachea during intubation [12], and the effect-site concentration of remifentanil required for achieving this is over 6.0 ng/ml [2]. In our clinical practice, following the administration of a high dose of remifentanil (0.3-0.5 µg/kg/min), anesthesia is induced with either propofol or ketamine, and a muscle relaxant. At the time of tracheal intubation, about four min after the commencement of remifentanil administration, the effect-site concentration of remifentanil is estimated, by pharmacokinetic simulation, to be over 6.0 ng/ml.
Propofol is used as one of the induction agents in this high-dose remifentanil administration technique [3]. Although this combination offers satisfactory induction conditions in a majority of the cases, it often causes cardiovascular depression during induction. This cardiovascular depression is probably caused by interaction between remifentanil and propofol [1]. Cardiovascular depression is unfavorable in patients with internal carotid artery stenosis. Moreover, during induction, especially until intubation is completed, cardiovascular depression is a cause for concern for anesthesiologists. Therefore, an anesthetic induction agent that does not cause cardiovascular depression upon combination with a high dose of remifentanil should be determined.
Ketamine is an N-methyl-D-aspartate (NMDA) receptor antagonist, and is categorized as a dissociative anesthetic. Ketamine is widely used to induce and maintain anesthesia, as is propofol. One of the several specific characteristics of ketamine is that it increases the heart rate and the blood pressure [45]. This characteristic may make ketamine useful as the anesthetic induction agent of choice to prevent cardiovascular depression during high-dose remifentanil administration. From this point of view, we often use ketamine, instead of propofol, when administering anesthesia by this technique. However, the suitability of ketamine as an alternative anesthetic induction agent to propofol for preventing cardiovascular depression during high-dose remifentanil administration has not been evaluated.
We hypothesized that ketamine, when administered as the anesthetic induction agent, may prevent cardiovascular depression during high-dose remifentanil administration, unlike propofol. To test our hypothesis, we retrospectively compared the hemodynamic effects of ketamine during high-dose remifentanil administration, with those of propofol.
This retrospective comparative study was approved by the Ethics Committee of the Nagasaki University Graduate School of Biomedical Sciences (No.1519). This study was performed using an automated anesthesia recording system (Prime Gaia, Nihon Kohden, Tokyo, Japan). Thirty-six patients who underwent oral surgery at the Nagasaki University Hospital between April 2014 and June 2015 were included in this study. Anesthesia, in all the cases, was induced by the following procedure: (1) High-dose remifentanil (0.3-0.5 µg/kg/min) was administered 2-3 min before anesthesia induction, (2) The anesthetic induction agent, either propofol (Group P) or ketamine (Group K) was administered, (3) After confirming the loss of consciousness, rocuronium (0.6-0.8 mg/kg) was administered for muscle relaxation, (4) The patient's lungs were ventilated with sevoflurane (2-3%), as a maintenance anesthetic agent, with 100% oxygen. (5) Finally, at least 4-5 min after the start of remifentanil administration, tracheal intubation was performed.
The mean arterial pressure (MAP) and heart rate data were collected at four time points by the automated anesthesia recording system: immediately before the administration of high-dose remifentanil (T1); immediately before the administration of the anesthetic induction agent (propofol or ketamine) (T2); and 2.5 min (T3), and 5 min (T4) after the administration of the anesthetic induction agent.
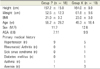
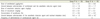
The patients' demographic data (age, sex, height, weight, body mass index, ASA physical status, type of primary medical history), anesthetic data (the dosages of remifentanil, anesthetic induction agent, and rocuronium; the concentration of sevoflurane; the interval between the administration of remifentanil and the anesthetic induction agent, and that between the administration of the anesthetic induction agent and tracheal intubation; the frequency of administration of the vasoactive agents), and the estimated effect-site concentration of remifentanil at T1-4, which was calculated by pharmacokinetic simulation (AnestAssist, Palma Healthcare Systems, Madison, Wisconsin, USA), were collected. All the data were collected by dental anesthesiologists who were blind to the purpose of this study.
Continuous and descriptive data were expressed as mean ± standard deviation (SD) or as a number. Continuous data between the groups were analyzed using the unpaired t-test. Descriptive data between the groups were analyzed using Fisher's exact test. Multiple intergroup comparisons of the MAP and the heart rate, and their relative values with respect to T1 were analyzed using repeated measures ANOVA, and the Bonferroni test was used for post hoc analysis. P < 0.01 was considered statistically significant.
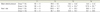
No significant differences were observed between the two groups in the patients' demographics, the anesthetic data, except for interval between the administration of the anesthetic induction agent and tracheal intubation, and the estimated effect-site concentration of remifentanil at T1-4 (Tables 1, 2, 3). The interval between the administration of the anesthetic induction agent and tracheal intubation was significantly longer in Group K (8.9 ± 4.2 min) than Group P (5.8 ± 1.2 min; P = 0.005).
In Group P, a comparison between the MAP and its relative value at T1 (94.0 ± 12.4 mmHg, 100 ± 0%) showed that the MAP values significantly decreased at T3 (75.7 ± 15.5 mmHg; P = 0.0015, 78.4 ± 13.8%; P < 0.001) and T4 (68.3 ± 12.5 mmHg; P < 0.001, 74.9 ± 31.0%; P < 0.001) (Fig. 1 and Table 4). However, the MAP (P = 0.133, Fig. 1) and its relative value (P = 0.130, Table 4) in Group K remained unchanged over time. Moreover, the MAP and its relative values at T3 (103.4 ± 21.3 mmHg; P < 0.001, 112.2 ± 23.4%; P < 0.001) and T4 (99.2 ± 19.8 mmHg; P < 0.001, 107.9 ± 25.1%; P < 0.001) in Group K were significantly higher than those in Group P (Fig. 1 and Table 4).
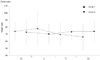
The heart rate and its relative value in both Group P (P = 0.254, P = 0.254) and Group K (P = 0.859, P = 0.468) were unchanged during the observation period (Fig. 2 and Table 4). There were no significant differences in the heart rate and its relative value between the two groups at any time point (T1: P = 0.783, P = 1, T2: P = 0.926, P = 0.421, T3: P = 0.424, P = 0.207, and T4: P = 0.175, P = 0.064) (Fig. 2 and Table 4).
The results of this retrospective comparative study showed that although propofol, when administered as the anesthetic induction agent during high-dose remifentanil administration, decreases the MAP, ketamine maintains it at control levels, and therefore, may prevent cardiovascular depression during high-dose remifentanil administration.
Ogletree et al. [6], in an in vitro study, reported that remifentanil has no negative inotropic effects. Moreover, they showed that the myocardial contractility remained fully responsive to beta-adrenergic stimulation at all remifentanil concentrations [6]. Duman et al. [7] also reported that remifentanil has no direct effect on myocardial contractility. The results of these previous reports suggest that the administration of a single dose of remifentanil, even at a high dose, does not cause cardiovascular depression. In the present study, there was no significant difference in the MAP and its relative value between T1 and T2, in the both groups. Our results are identical with those of the previous in vitro studies. Kurata [1] described that remifentanil exhibits strong interactions with other anesthetic agents, especially propofol. However, there has been no evidence to prove this suggestion. In our study, the MAP in Group P, at T3 and T4, decreased by over 20%, as compared to that at T1. As far as we know, this is the first report demonstrating the strong interaction of remifentanil with propofol. However, the heart rate and its relative value in Group P remained unchanged. Therefore, it seems that the interaction of remifentanil with propofol affects mainly the blood pressure, and not the heart rate.
Although it is well known that ketamine increases the heart rate, cardiac output, and blood pressure [45], the mechanism of these cardiovascular effects is still not completely understood [5]. Sprung et al. [8] reported that ketamine exerts a direct dose-dependent negative inotropic effect on human heart muscles. However, several lines of evidence indicate that ketamine activates the limbic system and increases the catecholamine concentration by inhibiting its neural reuptake [5]. It is presumed that these pharmacological changes override its negative inotropic effect. In the present study, however, both the MAP and the heart rate remained unchanged in Group K. This probably indicates that the interaction of ketamine and remifentanil may mask ketamine's cardiovascular stimulating effect, thus maintaining cardiovascular function.
In our study, the interval between the administration of the anesthetic induction agent and tracheal intubation in Group K was significantly longer than that in Group P. Although we wanted to compare the heart rate and the MAP in both the groups at the time of tracheal intubation, there was a significant difference in the estimated effect-site concentration of remifentanil at this point (Group P 8.2 ± 2.4 ng/ml vs. Group K 10.4 ± 2.0 ng/ml, P = 0.006). Therefore, we investigated the hemodynamic changes only until T4. We would like to examine the hemodynamic changes after T4 in a future prospective study.
In conclusion, we demonstrated that ketamine, used as the anesthetic induction agent during high-dose remifentanil administration, might prevent cardiovascular depression. The choice of ketamine as the induction agent during high-dose remifentanil administration might be a safer alternative to propofol in patients in whom cardiovascular depression needs to be avoided.
Figures and Tables
Fig. 1
Mean arterial pressure recorded in the propofol (P) and ketamine (K) groups at four time points: Immediately before the administration of high-dose remifentanil (T1); immediately before the administration of the anesthetic induction agent (T2); and 2.5 min (T3), and 5 min (T4) after the administration of the anesthetic induction agent. Data are expressed as mean ± standard deviation.
*P < 0.01 compared with T1. †P < 0.01 compared with Group P.
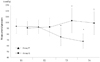
Fig. 2
Mean heart rate recorded in the propofol (P) and ketamine (K) groups at four time points: Immediately before the administration of high-dose remifentanil (T1); immediately before the administration of the anesthetic induction agent (T2); and 2.5 min (T3), and 5 min (T4) after the administration of the anesthetic induction agent. Data are expressed as mean ± standard deviation.
Acknowledgements
We thank Dr. Shoko Gamoh and Dr. Naotaka Kishimoto (Osaka Dental University) for improving this manuscript.
References
1. Kurata Y. High-dose remifentanil anesthesia. J Clin Anesth. 2008; 32:1692–1696.
2. Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, et al. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005; 101:125–130.

3. Kortelainen J, Koskinen M, Mustola S, Seppänen T. Effects of remifentanil on the spectrum and quantitative parameters of electroencephalogram in propofol anesthesia. Anesthesiology. 2009; 111:574–583.

4. Tweed WA, Minuck M, Mymin D. Circulatory responses to ketamine anesthesia. Anesthesiology. 1972; 37:613–619.

5. Haas DA, Harper DG. Ketamine: a review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog. 1992; 3:61–68.
6. Ogletree ML, Sprung J, Moravec CS. Effects of remifentanil on the contractility of failing human heart muscle. J Cardiothorac Vasc Anesth. 2005; 19:763–767.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download