Abstract
Purpose
Postoperative hypocalcemia is a common complication of thyroidectomy. This study evaluated the incidence and predisposing risk factors for postoperative permanent hypocalcemia after total thyroidectomy.
Methods
There were 1,247 consecutive patients undergoing total thyroidectomy and complete treatment and observation for differentiated thyroid cancer between January 2012 to December 2012 who were enrolled in this study. Patients were divided into two groups, those remaining normalcalcemic (Group I-824 pts) and those who had hypocalcemia requiring treatment (Groups II-423 pts). Group II was subdivided into a transient hypocalcemic group (Group IIA-409 pts) and a permanent hypocalcemic group (Group IIB-14 pts).
Results
Female gender, thyroiditis, preserved parathyroid number, lateral lymph node metastasis, RAI treatment, preoperative parathyroid hormone and preoperative vitamin D were significantly associated with the development of postoperative hypocalcemia by multivariate analysis. Comparing patients with transient versus permanent hypocalcemia, tumor size and multiplicity were significantly related to the development of permanent hypocalcemia by multivariate analysis. RAI treatment and parathyroid hormone level on the postoperative third day were significantly related to recovery from transient hypocalcemia to normo-calcemia.
Conclusion
Risk factors of postoperative hypocalcemia were associated with preoperative patient factors and advanced thyroid cancer. Advanced thyroid cancer was a risk factor for permanent hypocalcemia. To prevent postoperative hypocalcemia, we should focus on patient condition and need to preserve parathyroid gland more carefully in thyroid surgery.
Figures and Tables
Table 1
Clinicopathologic characteristics of the patients (1)

Table 2
Clinicopathologic characteristics of the patients (2)
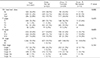
Table 3
Univariate & multivariate analysis: risk factors for postoperative hypocalcemia

Table 4
Univariate & multivariate analysis: risk factors for postoperative permanent hypocalcemia

Table 5
Univariate & multivariate analysis of factors affect to recovery from transient hypocalcemia to normal

References
1. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer Statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–450.

2. Sung MW, Park B, An SY, Hah JH, Jung YH, Choi HG. Increasing thyroid cancer rate and the extent of thyroid surgery in Korea. PLoS One. 2014; 9:e113464.

3. Ahn HS, Welch HG. South Korea's Thyroid-Cancer "Epidemic" --turning the tide. N Engl J Med. 2015; 373:2389–2390.

4. Bourrel C, Uzzan B, Tison P, Despreaux G, Frachet B, Modigliani E, et al. Transient hypocalcemia after thyroidectomy. Ann Otol Rhinol Laryngol. 1993; 102:496–501.

5. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998; 176:71–75.

6. Asari R, Passler C, Kaczirek K, Scheuba C, Niederle B. Hypoparathyroidism after total thyroidectomy: a prospective study. Arch Surg. 2008; 143:132–137. discussion 138.
7. Schwartz AE, Clark OH, Ituarte P, Lo Gerfo P. Therapeutic controversy: Thyroid surgery--the choice. J Clin Endocrinol Metab. 1998; 83:1097–1105.
8. Shiryazdi SM, Kargar S, Afkhami-Ardekani M, Neamatzadeh H. Risk of postoperative hypocalcemia in patients underwent total thyroidectomy, subtotal thyroidectomy and lobectomy surgeries. Acta Med Iran. 2014; 52:206–209.
9. Bove A, Di Renzo RM, Palone G, D'Addetta V, Percario R, Panaccio P, et al. Early biomarkers of hypocalcemia following total thyroidectomy. Int J Surg. 2014; 12:Suppl 1. S202–S204.

10. Cmilansky P, Mrozova L. Hypocalcemia - the most common complication after total thyroidectomy. Bratisl Lek Listy. 2014; 115:175–178.

11. Herranz González-Botas J, Lourido Piedrahita D. Hypocalcaemia after total thyroidectomy: incidence, control and treatment. Acta Otorrinolaringol Esp. 2013; 64:102–107.

12. Merchavy S, Marom T, Forest VI, Hier M, Mlynarek A, McHugh T, et al. Comparison of the incidence of postoperative hypocalcemia following total thyroidectomy vs completion thyroidectomy. Otolaryngol Head Neck Surg. 2015; 152:53–56.

13. Gac EP, Cabané TP, Amat VJ, Huidobro GF, Rossi FR, Rodríguez FF, et al. Incidence of hypocalcemia after total thyroidectomy. Rev Med Chil. 2007; 135:26–30.
14. Turanli S, Karaman N, Ozgen K. Permanent hypocalcemia in patients operated for thyroid carcinoma. Indian J Otolaryngol Head Neck Surg. 2009; 61:280–285.

15. Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014; 101:307–320.

16. Kim WW, Chung SH, Ban EJ, Lee CR, Kang SW, Jeong JJ, et al. Is preoperative Vitamin D deficiency a risk factor for postoperative symptomatic hypocalcemia in thyroid cancer patients undergoing total thyroidectomy plus central compartment neck dissection? Thyroid. 2015; 25:911–918.

17. Hallgrimsson P, Nordenström E, Almquist M, Bergenfelz AO. Risk factors for medically treated hypocalcemia after surgery for Graves' disease: a Swedish multicenter study of 1,157 patients. World J Surg. 2012; 36:1933–1942.

18. Kamer E, Unalp HR, Erbil Y, Akguner T, Issever H, Tarcan E. Early prediction of hypocalcemia after thyroidectomy by parathormone measurement in surgical site irrigation fluid. Int J Surg. 2009; 7:466–471.

19. Sands NB, Payne RJ, Côté V, Hier MP, Black MJ, Tamilia M. Female gender as a risk factor for transient post-thyroidectomy hypocalcemia. Otolaryngol Head Neck Surg. 2011; 145:561–564.

20. Moriyama T, Yamashita H, Noguchi S, Takamatsu Y, Ogawa T, Watanabe S, et al. Intraoperative parathyroid hormone assay in patients with Graves' disease for prediction of postoperative tetany. World J Surg. 2005; 29:1282–1287.

21. Al-Khatib T, Althubaiti AM, Althubaiti A, Mosli HH, Alwasiah RO, Badawood LM. Severe vitamin D deficiency: a significant predictor of early hypocalcemia after total thyroidectomy. Otolaryngol Head Neck Surg. 2015; 152:424–431.
22. Falcone TE, Stein DJ, Jumaily JS, Pearce EN, Holick MF, McAneny DB, et al. Correlating pre-operative vitamin D status with post-thyroidectomy hypocalcemia. Endocr Pract. 2015; 21:348–354.

23. Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist. 2013; 18:533–542.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download