1. Lazarus RS, Folkman S. Stress, appraisal and coping. New York (NY): Springer;1984.
2. Kinney JM, Jeejeebhoy KN, Hill GL, Owen OE. Nutrition and metabolism in patient care. Philadelphia (PA): Saunders;1988.
3. Weijs PJ, Wischmeyer PE. Optimizing energy and protein balance in the ICU. Curr Opin Clin Nutr Metab Care. 2013; 16:194–201. PMID:
23334173.

4. Faisy C, Lerolle N, Dachraoui F, Savard JF, Abboud I, Tadie JM, Fagon JY. Impact of energy deficit calculated by a predictive method on outcome in medical patients requiring prolonged acute mechanical ventilation. Br J Nutr. 2009; 101:1079–1087. PMID:
18778528.

5. Giner M, Laviano A, Meguid MM, Gleason JR. In 1995 a correlation between malnutrition and poor outcome in critically ill patients still exists. Nutrition. 1996; 12:23–29. PMID:
8838832.

6. Weijs PJ, Looijaard WG, Beishuizen A, Girbes AR, Straaten HM. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients. Crit Care. 2014; 18:701. PMID:
25499096.

7. Klein CJ, Stanek GS, Wiles CE 3rd. Overfeeding macronutrients to critically ill adults: metabolic complications. J Am Diet Assoc. 1998; 98:795–806. PMID:
9664922.
8. Preiser JC, van Zanten AR, Berger MM, Biolo G, Casaer MP, Doig GS, Griffiths RD, Heyland DK, Hiesmayr M, Iapichino G, Laviano A, Pichard C, Singer P, den Berghe GV, Wernerman J, Wischmeyer P, Vincent JL. Metabolic and nutritional support of critically ill patients: consensus and controversies. Crit Care. 2015; 19:35. PMID:
25886997.

9. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016; 40:159–211. PMID:
26773077.
10. Cuesta JM, Singer M. The stress response and critical illness: a review. Crit Care Med. 2012; 40:3283–3289. PMID:
22975887.
11. Wilmore DW. From Cuthbertson to fast-track surgery: 70 years of progress in reducing stress in surgical patients. Ann Surg. 2002; 236:643–648. PMID:
12409671.

12. Rolfes SR, Pinna K, Whitney EN. Understanding normal and clinical nutrition. 9th ed. Belmont (CA): Wadsworth/Cengage Learning;2012.
13. Cuthbertson DP. Post-shock metabolic response. Lancet. 1942; 239:433–437.
14. Cuthbertson DP. The metabolic response to injury and other related explorations in the field of protein metabolism: an autobiographical account. Scott Med J. 1982; 27:158–171. PMID:
7046044.

15. Weledji EP. Cytokines and the metabolic response to surgery. J Clin Cell Immunol. 2014; 5:197.

16. Stahel PF, Flierl MA, Moore EE. “Metabolic staging” after major trauma - a guide for clinical decision making? Scand J Trauma Resusc Emerg Med. 2010; 18:34. PMID:
20565752.

17. Santos L. Stress response in critical illness. Curr Probl Pediatr Adolesc Health Care. 2013; 43:264–272. PMID:
24295607.

18. Marik PE, Bellomo R. Stress hyperglycemia: an essential survival response! Crit Care. 2013; 17:305. PMID:
23470218.

19. Cuthbertson DP. Second annual Jonathan E. Rhoads Lecture. The metabolic response to injury and its nutritional implications: retrospect and prospect. J Parenter Enteral Nutr. 1979; 3:108–129.

20. Nelms M, Sucher KP, Lacey K, Roth SL. Nutrition therapy and pathophysiology. 2nd ed. Belmont (CA): Wadsworth/Cengage Learning;2011.
21. Preiser JC, Ichai C, Orban JC, Groeneveld AB. Metabolic response to the stress of critical illness. Br J Anaesth. 2014; 113:945–954. PMID:
24970271.

22. Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009; 373:1798–1807. PMID:
19465235.

23. Soeters MR, Soeters PB. The evolutionary benefit of insulin resistance. Clin Nutr. 2012; 31:1002–1007. PMID:
22682085.

24. Poehlman ET, Scheffers J, Gottlieb SS, Fisher ML, Vaitekevicius P. Increased resting metabolic rate in patients with congestive heart failure. Ann Intern Med. 1994; 121:860–862. PMID:
7772113.

25. Kao CC, Hsu JW, Bandi V, Hanania NA, Kheradmand F, Jahoor F. Resting energy expenditure and protein turnover are increased in patients with severe chronic obstructive pulmonary disease. Metabolism. 2011; 60:1449–1455. PMID:
21550084.

26. Sammarco R, Marra M, Pagano MC, Alfonsi L, Santarpia L, Cioffi I, Contaldo F, Pasanisi F. Resting energy expenditure in adult patients with Crohn’s disease. Clin Nutr. 2017; 36:467–470. PMID:
26869381.

27. Monk DN, Plank LD, Franch-Arcas G, Finn PJ, Streat SJ, Hill GL. Sequential changes in the metabolic response in critically injured patients during the first 25 days after blunt trauma. Ann Surg. 1996; 223:395–405. PMID:
8633918.

28. Wang CY, Huang CT, Chen CH, Chen MF, Ching SL, Huang YC. Optimal energy delivery, rather than the implementation of a feeding protocol, may benefit clinical outcomes in critically ill patients. Nutrients. 2017; 9:E527. PMID:
28531142.

29. Taylor SJ, Fettes SB, Jewkes C, Nelson RJ. Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med. 1999; 27:2525–2531. PMID:
10579275.

30. Martin CM, Doig GS, Heyland DK, Morrison T, Sibbald WJ. Multicentre, cluster-randomized clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT). CMAJ. 2004; 170:197–204. PMID:
14734433.

31. van Schijndel RJ, Weijs PJ, Koopmans RH, Sauerwein HP, Beishuizen A, Girbes AR. Optimal nutrition during the period of mechanical ventilation decreases mortality in critically ill, long-term acute female patients: a prospective observational cohort study. Crit Care. 2009; 13:R132. PMID:
19671136.
32. Singer P, Hiesmayr M, Biolo G, Felbinger TW, Berger MM, Goeters C, Kondrup J, Wunder C, Pichard C. Pragmatic approach to nutrition in the ICU: expert opinion regarding which calorie protein target. Clin Nutr. 2014; 33:246–251. PMID:
24434033.

33. Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care. 2016; 20:367. PMID:
27832823.

34. Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R. Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr. 2011; 93:569–577. PMID:
21270385.

35. Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P. Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA. 2012; 307:795–803. PMID:
22307571.
36. Rice TW, Mogan S, Hays MA, Bernard GR, Jensen GL, Wheeler AP. A randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med. 2011; 39:967–974. PMID:
21242788.
37. Sanches AC, de Góes CR, Bufarah MN, Balbi AL, Ponce D. Resting energy expenditure in critically ill patients: evaluation methods and clinical applications. Rev Assoc Med Bras. 2016; 62:672–679. PMID:
27925048.

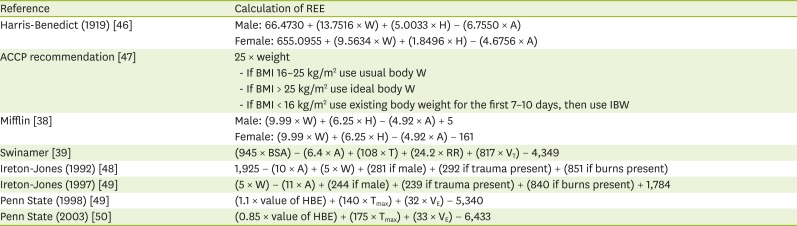
38. Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990; 51:241–247. PMID:
2305711.

39. Swinamer DL, Grace MG, Hamilton SM, Jones RL, Roberts P, King EG. Predictive equation for assessing energy expenditure in mechanically ventilated critically ill patients. Crit Care Med. 1990; 18:657–661. PMID:
2344758.

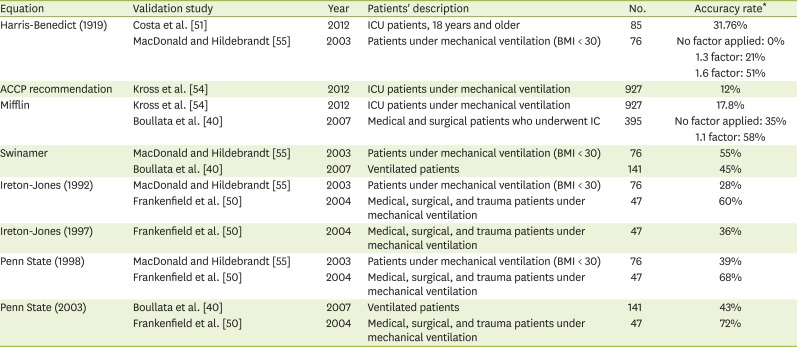
40. Boullata J, Williams J, Cottrell F, Hudson L, Compher C. Accurate determination of energy needs in hospitalized patients. J Am Diet Assoc. 2007; 107:393–401. PMID:
17324656.

41. de Waele E, Opsomer T, Honoré PM, Diltoer M, Mattens S, Huyghens L, Spapen H. Measured versus calculated resting energy expenditure in critically ill adult patients. Do mathematics match the gold standard? Minerva Anestesiol. 2015; 81:272–282. PMID:
25077603.
42. Picolo MF, Lago AF, Menegueti MG, Nicolini EA, Basile-Filho A, Nunes AA, Martins-Filho OA, Auxiliadora-Martins M. Harris-Benedict equation and resting energy expenditure estimates in critically ill ventilator patients. Am J Crit Care. 2016; 25:e21–e29. PMID:
26724304.

43. Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949; 109:1–9. PMID:
15394301.

44. Walker RN, Heuberger RA. Predictive equations for energy needs for the critically ill. Respir Care. 2009; 54:509–521. PMID:
19327188.
45. Schlein KM, Coulter SP. Best practices for determining resting energy expenditure in critically ill adults. Nutr Clin Pract. 2014; 29:44–55. PMID:
24336442.

46. Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci USA. 1918; 4:370–373. PMID:
16576330.

47. Cerra FB, Benitez MR, Blackburn GL, Irwin RS, Jeejeebhoy K, Katz DP, Pingleton SK, Pomposelli J, Rombeau JL, Shronts E, Wolfe RR, Zaloga GP. Applied nutrition in ICU patients. A consensus statement of the American College of Chest Physicians. Chest. 1997; 111:769–778. PMID:
9118718.
48. Ireton-Jones CS, Turner WW Jr, Liepa GU, Baxter CR. Equations for the estimation of energy expenditures in patients with burns with special reference to ventilatory status. J Burn Care Rehabil. 1992; 13:330–333. PMID:
1618877.

49. Ireton-Jones C, Jones JD. Why use predictive equations for energy expenditure assessment? J Acad Nutr Diet. 1997; 97(Suppl):A44.

50. Frankenfield D, Smith JS, Cooney RN. Validation of 2 approaches to predicting resting metabolic rate in critically ill patients. JPEN J Parenter Enteral Nutr. 2004; 28:259–264. PMID:
15291408.

51. Costa NA, Marinho AD, Cancado LR. Nutritional requirements of the critically ill patient. Rev Bras Ter Intensiva. 2012; 24:270–277. PMID:
23917829.
52. Koukiasa P, Bitzani M, Papaioannou V, Pnevmatikos I. Resting energy expenditure in critically ill patients with spontaneous intracranial hemorrhage. JPEN J Parenter Enteral Nutr. 2015; 39:917–921. PMID:
24928226.

53. Martins MA, Menegueti MG, Nicolini EA, Picolo MF, Lago AF, Filho OA, Filho AB. Energy expenditure in critically ill surgical patients. Comparative analysis of predictive equation and indirect calorimetry. Acta Cir Bras. 2011; 26(Suppl 2):51–56.

54. Kross EK, Sena M, Schmidt K, Stapleton RD. A comparison of predictive equations of energy expenditure and measured energy expenditure in critically ill patients. J Crit Care. 2012; 27:321.e5–321.12.

55. Macdonald A, Hildebrandt L. Comparison of formulaic equations to determine energy expenditure in the critically ill patient. Nutrition. 2003; 19:233–239. PMID:
12620525.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download