1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386. PMID:
25220842.

2. Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, Bray F. International variation in prostate cancer incidence and mortality rates. Eur Urol. 2012; 61:1079–1092. PMID:
22424666.

3. Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, Fossati N, Gross T, Henry AM, Joniau S, Lam TB, Mason MD, Matveev VB, Moldovan PC, van den Bergh RC, Van den Broeck T, van der Poel HG, van der Kwast TH, Rouvière O, Schoots IG, Wiegel T, Cornford P. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017; 71:618–629. PMID:
27568654.

4. Leitzmann MF, Rohrmann S. Risk factors for the onset of prostatic cancer: age, location, and behavioral correlates. Clin Epidemiol. 2012; 4:1–11.

5. Lin PH, Aronson W, Freedland SJ. Nutrition, dietary interventions and prostate cancer: the latest evidence. BMC Med. 2015; 13:3. PMID:
25573005.

7. World Cancer Research Fund. American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, D.C.: American Institute for Cancer Research;2007.
8. Shivappa N, Jackson MD, Bennett F, Hébert JR. Increased Dietary Inflammatory Index (DII) is associated with increased risk of prostate cancer in Jamaican men. Nutr Cancer. 2015; 67:941–948. PMID:
26226289.

9. Schulze MB, Hoffmann K. Methodological approaches to study dietary patterns in relation to risk of coronary heart disease and stroke. Br J Nutr. 2006; 95:860–869. PMID:
16611375.

10. Yusof AS, Isa ZM, Shah SA. Dietary patterns and risk of colorectal cancer: a systematic review of cohort studies (2000–2011). Asian Pac J Cancer Prev. 2012; 13:4713–4717. PMID:
23167408.

11. Reedy J, Wirfält E, Flood A, Mitrou PN, Krebs-Smith SM, Kipnis V, Midthune D, Leitzmann M, Hollenbeck A, Schatzkin A, Subar AF. Comparing 3 dietary pattern methods--cluster analysis, factor analysis, and index analysis--with colorectal cancer risk: The NIH-AARP Diet and Health Study. Am J Epidemiol. 2010; 171:479–487. PMID:
20026579.

12. Fabiani R, Minelli L, Bertarelli G, Bacci S. A western dietary pattern increases prostate cancer risk: a systematic review and meta-analysis. Nutrients. 2016; 8:E626. PMID:
27754328.

13. López-Guarnido O, Álvarez-Cubero MJ, Saiz M, Lozano D, Rodrigo L, Pascual M, Cozar JM, Rivas A. Mediterranean diet adherence and prostate cancer risk. Nutr Hosp. 2014; 31:1012–1019. PMID:
25726188.
14. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003; 348:2599–2608. PMID:
12826634.

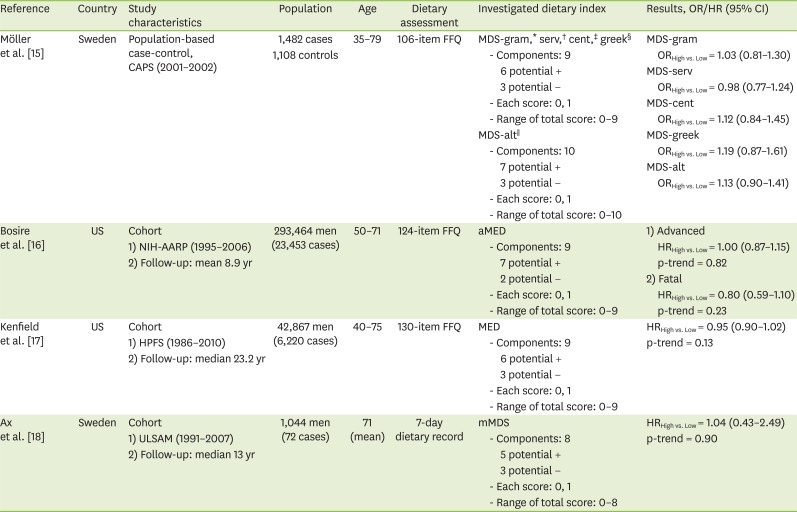
15. Möller E, Galeone C, Andersson TM, Bellocco R, Adami HO, Andrén O, Grönberg H, La Vecchia C, Mucci LA, Bälter K. Mediterranean Diet Score and prostate cancer risk in a Swedish population-based case-control study. J Nutr Sci. 2013; 2:e15. PMID:
25191563.

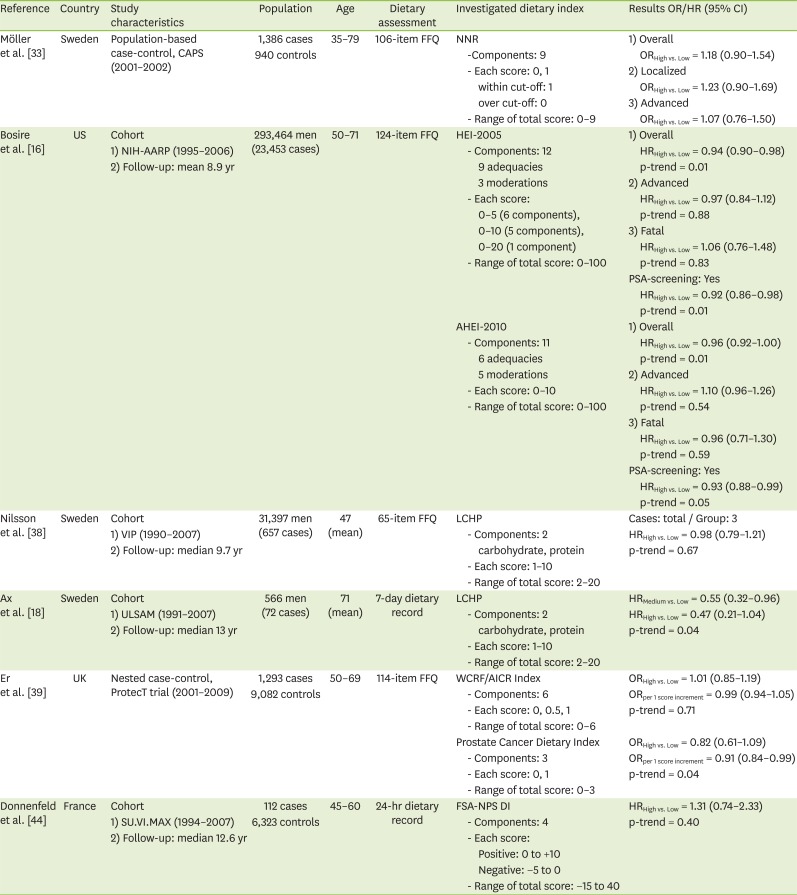
16. Bosire C, Stampfer MJ, Subar AF, Park Y, Kirkpatrick SI, Chiuve SE, Hollenbeck AR, Reedy J. Index-based dietary patterns and the risk of prostate cancer in the NIH-AARP diet and health study. Am J Epidemiol. 2013; 177:504–513. PMID:
23408548.

17. Kenfield SA, DuPre N, Richman EL, Stampfer MJ, Chan JM, Giovannucci EL. Mediterranean diet and prostate cancer risk and mortality in the Health Professionals Follow-up Study. Eur Urol. 2014; 65:887–894. PMID:
23962747.

18. Ax E, Garmo H, Grundmark B, Bill-Axelson A, Holmberg L, Becker W, Zethelius B, Cederholm T, Sjögren P. Dietary patterns and prostate cancer risk: report from the population based ULSAM cohort study of Swedish men. Nutr Cancer. 2014; 66:77–87. PMID:
24325263.

19. Cavicchia PP, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, Hébert JR. A new dietary inflammatory index predicts interval changes in serum high-sensitivity C-reactive protein. J Nutr. 2009; 139:2365–2372. PMID:
19864399.

20. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014; 17:1689–1696. PMID:
23941862.

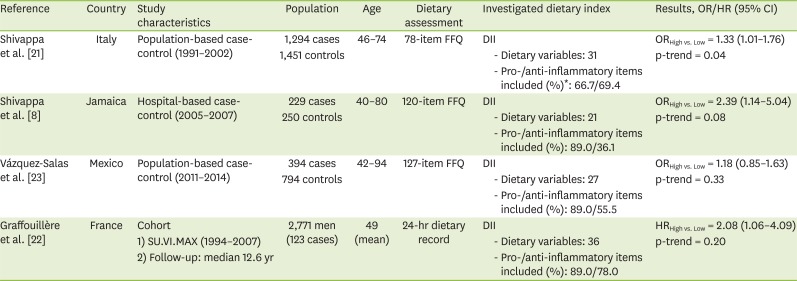
21. Shivappa N, Bosetti C, Zucchetto A, Montella M, Serraino D, La Vecchia C, Hébert JR. Association between dietary inflammatory index and prostate cancer among Italian men. Br J Nutr. 2015; 113:278–283. PMID:
25400225.

22. Graffouillère L, Deschasaux M, Mariotti F, Neufcourt L, Shivappa N, Hébert JR, Wirth MD, Latino-Martel P, Hercberg S, Galan P, Julia C, Kesse-Guyot E, Touvier M. The dietary inflammatory index is associated with prostate cancer risk in French middle-aged adults in a prospective study. J Nutr. 2016; 146:785–791.

23. Vázquez-Salas RA, Shivappa N, Galván-Portillo M, López-Carrillo L, Hébert JR, Torres-Sánchez L. Dietary inflammatory index and prostate cancer risk in a case-control study in Mexico. Br J Nutr. 2016; 116:1945–1953. PMID:
27927252.

24. Poljsak B, Šuput D, Milisav I. Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxid Med Cell Longev. 2013; 2013:956792. PMID:
23738047.

25. Khandrika L, Kumar B, Koul S, Maroni P, Koul HK. Oxidative stress in prostate cancer. Cancer Lett. 2009; 282:125–136. PMID:
19185987.

26. Halliwell B. Free radicals, antioxidants, and human disease: curiosity, cause, or consequence? Lancet. 1994; 344:721–724. PMID:
7915779.

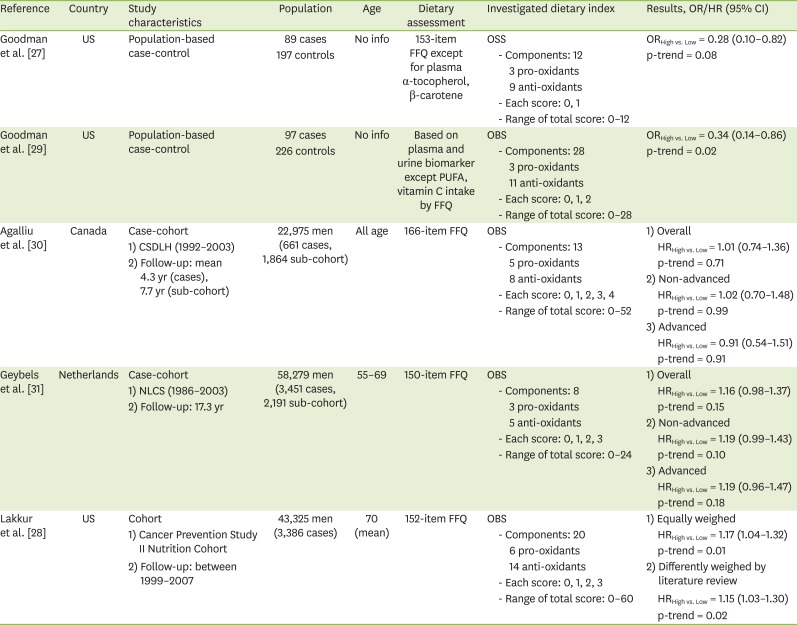
27. Goodman M, Bostick RM, Dash C, Flanders WD, Mandel JS. Hypothesis: oxidative stress score as a combined measure of pro-oxidant and antioxidant exposures. Ann Epidemiol. 2007; 17:394–399. PMID:
17462547.

28. Lakkur S, Goodman M, Bostick RM, Citronberg J, McClellan W, Flanders WD, Judd S, Stevens VL. Oxidative balance score and risk for incident prostate cancer in a prospective U.S. cohort study. Ann Epidemiol. 2014; 24:475–478.e4. PMID:
24731700.

29. Goodman M, Bostick RM, Gross M, Thyagarajan B, Dash C, Flanders WD. Combined measure of pro- and anti-oxidant exposures in relation to prostate cancer and colorectal adenoma risk: an update. Ann Epidemiol. 2010; 20:955–957. PMID:
21074110.

30. Agalliu I, Kirsh VA, Kreiger N, Soskolne CL, Rohan TE. Oxidative balance score and risk of prostate cancer: results from a case-cohort study. Cancer Epidemiol. 2011; 35:353–361. PMID:
21145797.

31. Geybels MS, Verhage BA, van Schooten FJ, van den Brandt PA. Measures of combined antioxidant and pro-oxidant exposures and risk of overall and advanced stage prostate cancer. Ann Epidemiol. 2012; 22:814–820. PMID:
22986088.

32. Becker W, Lyhne N, Pedersen AN, Aro A, Fogelholm M, Phorsdottir I, Alexander J, Anderssen SA, Meltzer HM, Pedersen JI. Nordic Nutrition Recommendations 2004-integrating nutrition and physical activity. Scand J Nutr. 2004; 48:178–187.
33. Möller E, Galeone C, Adami HO, Adolfsson J, Andersson TM, Bellocco R, Grönberg H, Mucci LA, Bälter K. The Nordic Nutrition Recommendations and prostate cancer risk in the Cancer of the Prostate in Sweden (CAPS) study. Public Health Nutr. 2012; 15:1897–1908. PMID:
22463871.

34. Fondell E, Christensen SE, Bälter O, Bälter K. Adherence to the Nordic Nutrition Recommendations as a measure of a healthy diet and upper respiratory tract infection. Public Health Nutr. 2011; 14:860–869. PMID:
20854722.

35. Britten P, Marcoe K, Yamini S, Davis C. Development of food intake patterns for the My Pyramid Food Guidance System. J Nutr Educ Behav. 2006; 38:S78–S92. PMID:
17116598.
36. Guenther PM, Reedy J, Krebs-Smith SM. Development of the healthy eating index-2005. J Am Diet Assoc. 2008; 108:1896–1901. PMID:
18954580.

37. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012; 142:1009–1018. PMID:
22513989.

38. Nilsson LM, Winkvist A, Johansson I, Lindahl B, Hallmans G, Lenner P, Van Guelpen B. Low-carbohydrate, high-protein diet score and risk of incident cancer; a prospective cohort study. Nutr J. 2013; 12:58. PMID:
23651548.

39. Er V, Lane JA, Martin RM, Emmett P, Gilbert R, Avery KN, Walsh E, Donovan JL, Neal DE, Hamdy FC, Jeffreys M. Adherence to dietary and lifestyle recommendations and prostate cancer risk in the prostate testing for cancer and treatment (ProtecT) trial. Cancer Epidemiol Biomarkers Prev. 2014; 23:2066–2077. PMID:
25017249.

40. Rayner M, Scarborough P, Boxer A, Stockley L. Nutrient profiles: development of final model. London: Food Standards Agency;2005.
41. Rayner M, Scarborough P, Stockley L. Nutrient profiles: applicability of currently proposed model for uses in relation to promotion of foods in children aged 5??0 and adults. London: Food Standards Agency;2005.
42. Julia C, Touvier M, Méjean C, Ducrot P, Péneau S, Hercberg S, Kesse-Guyot E. Development and validation of an individual dietary index based on the British Food Standard Agency nutrient profiling system in a French context. J Nutr. 2014; 144:2009–2017. PMID:
25411035.

43. Julia C, Kesse-Guyot E, Touvier M, Méjean C, Fezeu L, Hercberg S. Application of the British Food Standards Agency nutrient profiling system in a French food composition database. Br J Nutr. 2014; 112:1699–1705. PMID:
25277084.

44. Donnenfeld M, Julia C, Kesse-Guyot E, Méjean C, Ducrot P, Péneau S, Deschasaux M, Latino-Martel P, Fezeu L, Hercberg S, Touvier M. Prospective association between cancer risk and an individual dietary index based on the British Food Standards Agency Nutrient Profiling System. Br J Nutr. 2015; 114:1702–1710. PMID:
26393396.

45. Schwingshackl L, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: a systematic review and meta-analysis of observational studies. Int J Cancer. 2014; 135:1884–1897. PMID:
24599882.

46. Grosso G, Mistretta A, Frigiola A, Gruttadauria S, Biondi A, Basile F, Vitaglione P, D'Orazio N, Galvano F. Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr. 2014; 54:593–610. PMID:
24261534.

47. Schwingshackl L, Missbach B, König J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr. 2015; 18:1292–1299. PMID:
25145972.

48. Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des. 2009; 15:1949–1955. PMID:
19519435.

49. Shivappa N, Prizment AE, Blair CK, Jacobs DR Jr, Steck SE, Hébert JR. Dietary inflammatory index and risk of colorectal cancer in the Iowa Women’s Health Study. Cancer Epidemiol Biomarkers Prev. 2014; 23:2383–2392. PMID:
25155761.

50. Tabung FK, Steck SE, Ma Y, Liese AD, Zhang J, Caan B, Hou L, Johnson KC, Mossavar-Rahmani Y, Shivappa N, Wactawski-Wende J, Ockene JK, Hebert JR. The association between dietary inflammatory index and risk of colorectal cancer among postmenopausal women: results from the Women’s Health Initiative. Cancer Causes Control. 2015; 26:399–408. PMID:
25549833.

51. Wirth MD, Shivappa N, Steck SE, Hurley TG, Hébert JR. The dietary inflammatory index is associated with colorectal cancer in the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Br J Nutr. 2015; 113:1819–1827. PMID:
25871645.

52. Shivappa N, Zucchetto A, Montella M, Serraino D, Steck SE, La Vecchia C, Hébert JR. Inflammatory potential of diet and risk of colorectal cancer: a case-control study from Italy. Br J Nutr. 2015; 114:152–158. PMID:
26050563.

53. Zamora-Ros R, Shivappa N, Steck SE, Canzian F, Landi S, Alonso MH, Hébert JR, Moreno V. Dietary inflammatory index and inflammatory gene interactions in relation to colorectal cancer risk in the Bellvitge colorectal cancer case-control study. Genes Nutr. 2015; 10:447. PMID:
25488145.

54. Shivappa N, Hébert JR, Ferraroni M, La Vecchia C, Rossi M. Association between dietary inflammatory index and gastric cancer risk in an Italian case-control study. Nutr Cancer. 2016; 68:1262–1268. PMID:
27636679.

55. Shivappa N, Bosetti C, Zucchetto A, Serraino D, La Vecchia C, Hébert JR. Dietary inflammatory index and risk of pancreatic cancer in an Italian case-control study. Br J Nutr. 2015; 113:292–298. PMID:
25515552.

56. Shivappa N, Zucchetto A, Serraino D, Rossi M, La Vecchia C, Hébert JR. Dietary inflammatory index and risk of esophageal squamous cell cancer in a case-control study from Italy. Cancer Causes Control. 2015; 26:1439–1447. PMID:
26208592.

57. Shivappa N, Hébert JR, Rashidkhani B. Dietary inflammatory index and risk of esophageal squamous cell cancer in a case-control study from Iran. Nutr Cancer. 2015; 67:1253–1259. PMID:
26400625.

58. Shivappa N, Hébert JR, Zucchetto A, Montella M, Serraino D, La Vecchia C, Rossi M. Dietary inflammatory index and endometrial cancer risk in an Italian case-control study. Br J Nutr. 2016; 115:138–146. PMID:
26507451.

59. Shivappa N, Hébert JR, Polesel J, Zucchetto A, Crispo A, Montella M, Franceschi S, Rossi M, La Vecchia C, Serraino D. Inflammatory potential of diet and risk for hepatocellular cancer in a case-control study from Italy. Br J Nutr. 2016; 115:324–331. PMID:
26556602.

60. Shivappa N, Sandin S, Löf M, Hébert JR, Adami HO, Weiderpass E. Prospective study of dietary inflammatory index and risk of breast cancer in Swedish women. Br J Cancer. 2015; 113:1099–1103. PMID:
26335605.

61. Ge I, Rudolph A, Shivappa N, Flesch-Janys D, Hébert JR, Chang-Claude J. Dietary inflammation potential and postmenopausal breast cancer risk in a German case-control study. Breast. 2015; 24:491–496. PMID:
25987487.

62. Maisonneuve P, Shivappa N, Hébert JR, Bellomi M, Rampinelli C, Bertolotti R, Spaggiari L, Palli D, Veronesi G, Gnagnarella P. Dietary inflammatory index and risk of lung cancer and other respiratory conditions among heavy smokers in the COSMOS screening study. Eur J Nutr. 2016; 55:1069–1079. PMID:
25953452.

63. Wood LG, Shivappa N, Berthon BS, Gibson PG, Hebert JR. Dietary inflammatory index is related to asthma risk, lung function and systemic inflammation in asthma. Clin Exp Allergy. 2015; 45:177–183. PMID:
24708388.

64. Wirth MD, Burch J, Shivappa N, Violanti JM, Burchfiel CM, Fekedulegn D, Andrew ME, Hartley TA, Miller DB, Mnatsakanova A, Charles LE, Steck SE, Hurley TG, Vena JE, Hébert JR. Association of a dietary inflammatory index with inflammatory indices and metabolic syndrome among police officers. J Occup Environ Med. 2014; 56:986–989. PMID:
25046320.

65. Goodman M, Bostick RM, Dash C, Terry P, Flanders WD, Mandel J. A summary measure of pro- and anti-oxidant exposures and risk of incident, sporadic, colorectal adenomas. Cancer Causes Control. 2008; 19:1051–1064. PMID:
18543072.

66. Kong SY, Bostick RM, Flanders WD, McClellan WM, Thyagarajan B, Gross MD, Judd S, Goodman M. Oxidative balance score, colorectal adenoma, and markers of oxidative stress and inflammation. Cancer Epidemiol Biomarkers Prev. 2014; 23:545–554. PMID:
24443405.

67. Dash C, Goodman M, Flanders WD, Mink PJ, McCullough ML, Bostick RM. Using pathway-specific comprehensive exposure scores in epidemiology: application to oxidative balance in a pooled case-control study of incident, sporadic colorectal adenomas. Am J Epidemiol. 2013; 178:610–624. PMID:
23639935.

68. Slattery ML, John EM, Torres-Mejia G, Lundgreen A, Lewinger JP, Stern MC, Hines L, Baumgartner KB, Giuliano AR, Wolff RK. Angiogenesis genes, dietary oxidative balance and breast cancer risk and progression: the Breast Cancer Health Disparities Study. Int J Cancer. 2014; 134:629–644. PMID:
23832257.

69. Annor FB, Goodman M, Okosun IS, Wilmot DW, Il’yasova D, Ndirangu M, Lakkur S. Oxidative stress, oxidative balance score, and hypertension among a racially diverse population. J Am Soc Hypertens. 2015; 9:592–599. PMID:
26160262.

70. Kong SY, Goodman M, Judd S, Bostick RM, Flanders WD, McClellan W. Oxidative balance score as predictor of all-cause, cancer, and noncancer mortality in a biracial US cohort. Ann Epidemiol. 2015; 25:256–262.e1. PMID:
25682727.

71. Kyrø C, Skeie G, Loft S, Overvad K, Christensen J, Tjønneland A, Olsen A. Adherence to a healthy Nordic food index is associated with a lower incidence of colorectal cancer in women: the Diet, Cancer and Health cohort study. Br J Nutr. 2013; 109:920–927. PMID:
22874538.

72. Roswall N, Li Y, Kyrø C, Sandin S, Löf M, Adami HO, Weiderpass E. No association between adherence to a healthy Nordic food index and colorectal cancer: results from a Swedish Cohort Study. Cancer Epidemiol Biomarkers Prev. 2015; 24:755–757. PMID:
25628334.

73. Miller PE, Lazarus P, Lesko SM, Muscat JE, Harper G, Cross AJ, Sinha R, Ryczak K, Escobar G, Mauger DT, Hartman TJ. Diet index-based and empirically derived dietary patterns are associated with colorectal cancer risk. J Nutr. 2010; 140:1267–1273. PMID:
20444952.

74. Reedy J, Mitrou PN, Krebs-Smith SM, Wirfält E, Flood A, Kipnis V, Leitzmann M, Mouw T, Hollenbeck A, Schatzkin A, Subar AF. Index-based dietary patterns and risk of colorectal cancer: the NIH-AARP Diet and Health Study. Am J Epidemiol. 2008; 168:38–48. PMID:
18525082.
75. Arem H, Reedy J, Sampson J, Jiao L, Hollenbeck AR, Risch H, Mayne ST, Stolzenberg-Solomon RZ. The Healthy Eating Index 2005 and risk for pancreatic cancer in the NIH-AARP study. J Natl Cancer Inst. 2013; 105:1298–1305. PMID:
23949329.

76. Chandran U, Bandera EV, Williams-King MG, Paddock LE, Rodriguez-Rodriguez L, Lu SE, Faulkner S, Pulick K, Olson SH. Healthy eating index and ovarian cancer risk. Cancer Causes Control. 2011; 22:563–571. PMID:
21286802.

77. Varraso R, Chiuve SE, Fung TT, Barr RG, Hu FB, Willett WC, Camargo CA. Alternate Healthy Eating Index 2010 and risk of chronic obstructive pulmonary disease among US women and men: prospective study. BMJ. 2015; 350:h286. PMID:
25649042.

78. Jacobs S, Harmon BE, Boushey CJ, Morimoto Y, Wilkens LR, Le Marchand L, Kröger J, Schulze MB, Kolonel LN, Maskarinec G. A priori-defined diet quality indexes and risk of type 2 diabetes: the Multiethnic Cohort. Diabetologia. 2015; 58:98–112. PMID:
25319012.

79. Lagiou P, Sandin S, Lof M, Trichopoulos D, Adami HO, Weiderpass E. Low carbohydrate-high protein diet and incidence of cardiovascular diseases in Swedish women: prospective cohort study. BMJ. 2012; 344:e4026. PMID:
22735105.

80. Nilsson LM, Winkvist A, Eliasson M, Jansson JH, Hallmans G, Johansson I, Lindahl B, Lenner P, Van Guelpen B. Low-carbohydrate, high-protein score and mortality in a Northern Swedish population-based cohort. Eur J Clin Nutr. 2012; 66:694–700. PMID:
22333874.

81. Hastert TA, Beresford SA, Patterson RE, Kristal AR, White E. Adherence to WCRF/AICR cancer prevention recommendations and risk of postmenopausal breast cancer. Cancer Epidemiol Biomarkers Prev. 2013; 22:1498–1508. PMID:
23780838.

82. Nomura SJ, Inoue-Choi M, Lazovich D, Robien K. WCRF/AICR recommendation adherence and breast cancer incidence among postmenopausal women with and without non-modifiable risk factors. Int J Cancer. 2016; 138:2602–2615. PMID:
26756307.

83. Lucas AL, Bravi F, Boffetta P, Polesel J, Serraino D, La Vecchia C, Bosetti C. Adherence to World Cancer Research Fund/American Institute for Cancer Research recommendations and pancreatic cancer risk. Cancer Epidemiol. 2016; 40:15–21. PMID:
26605429.

84. Bravi F, Polesel J, Garavello W, Serraino D, Negri E, Franchin G, La Vecchia C, Bosetti C. Adherence to the World Cancer Research Fund/American Institute for Cancer Research recommendations and head and neck cancers risk. Oral Oncol. 2017; 64:59–64. PMID:
28024725.

85. Hastert TA, Beresford SA, Sheppard L, White E. Adherence to the WCRF/AICR cancer prevention recommendations and cancer-specific mortality: results from the Vitamins and Lifestyle (VITAL) Study. Cancer Causes Control. 2014; 25:541–552. PMID:
24557428.

86. Julia C, Fézeu LK, Ducrot P, Méjean C, Péneau S, Touvier M, Hercberg S, Kesse-Guyot E. The nutrient profile of foods consumed using the British Food Standards Agency nutrient profiling system is associated with metabolic syndrome in the SU.VI.MAX cohort. J Nutr. 2015; 145:2355–2361. PMID:
26290007.

87. Adriouch S, Julia C, Kesse-Guyot E, Méjean C, Ducrot P, Péneau S, Donnenfeld M, Deschasaux M, Menai M, Hercberg S, Touvier M, Fezeu LK. Prospective association between a dietary quality index based on a nutrient profiling system and cardiovascular disease risk. Eur J Prev Cardiol. 2016; 23:1669–1676. PMID:
27000099.

88. Adriouch S, Julia C, Kesse-Guyot E, Ducrot P, Péneau S, Méjean C, Assmann KE, Deschasaux M, Hercberg S, Touvier M, Fezeu LK. Association between a dietary quality index based on the food standard agency nutrient profiling system and cardiovascular disease risk among French adults. Int J Cardiol. 2017; 234:22–27. PMID:
28258849.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download