Abstract
Although it has been proposed that trace minerals have anti-oxidative functions and are related to the control of blood pressure, only a limited number of studies directly address the issue. Thus, the purpose of our study was to assess the intake of copper and manganese, which are trace minerals, and to clarify their relation to blood pressure. In a cross-sectional study, the blood pressure of 640 normotensive adults, from 19 to 69 year-old (320 males and 320 females), was measured, and its correlation with the intake of copper and manganese was assessed using a 24-hour dietary recall method. The average value of the blood pressure was 126.4/80.2 mmHg for the males and 117.8/75.8 mmHg for the females. The daily copper intake was 1.3 mg/day for the males and 1.2 mg/day for the females. For manganese, the daily intake was 4.2 mg/day for the males and 4.1 mg/day for the females. Although the copper intake of all subjects showed a positive correlation with the systolic and diastolic blood pressures, there was no significant correlation when the potential confounding factors were adjusted. The manganese intake of the male subjects had a significantly negative correlation with the systolic blood pressure after adjusting for gender, age, body mass index, and energy intake. In conclusion, the daily manganese intake of the normotensitve adults showed a significantly negative correlation with the systolic blood pressure indicating a possibility of a positive effect of manganese on blood pressure.
Worldwide, the prevalence of hypertension is high, and it is one of the major health risk factors that cause various diseases. According to the 2011-2012 National Health and Nutrition Examination Survey (NHANES) in the United States of America (USA), the hypertension prevalence in adults over 18 years of age was 29.7% for the males and 28.5% for the females [1]. In the 2012 Korea NHANES, the hypertension prevalence was 33.3% and 29.8% for the males and females in the age of over 30 year-old, respectively, which was an increase from 24.6% (average value of male and female) in 2007 [2]. The hypertension risk factors include the uncontrollable factors, such as genetics, race, and aging, and controllable factors, which can be corrected by living habit or diet. To prevent and control hypertension, proper living habits are required. Furthermore, it is necessary to conduct a study to determine various controllable factors related to blood pressure.
Because dietary factors are related to blood pressure, studies focusing on major minerals such as sodium, potassium, calcium, magnesium, and others have been conducted. While a high sodium intake increases the blood pressure, a low intake of potassium, calcium, and magnesium increases the blood pressure [3456]. Therefore, to manage the blood pressure using proper diet, a reduction in sodium intake and a sufficient intake of potassium, calcium, and magnesium are emphasized [7].
Among the diverse dietary factors, minerals with an anti-oxidative function play a vital role in preventing cardiovascular disorders [8910]. It has been reported in an epidemiologic study that a low serum level of iron, zinc, and copper is related to coronary artery disease, and the mechanism is related to a vascular cell dysfunction or an inflammatory response [111213]. It has been reported that a shortage of manganese, which has an anti-oxidative function, causes glucose intolerance, inhibition of carbohydrate and lipid metabolism, and reduces blood high-density lipoprotein cholesterol [1415]. However, it is necessary to conduct a study to determine whether these minerals are related to blood pressure.
The aims of the present study were as follows: first, to evaluate the daily intakes of copper and manganese in the normotensive adults according to age groups; and second, to investigate the correlation between dietary copper and manganese intakes and blood pressure in the normotensive adults.
Because the age range of adults was broad, it was classified into 19-29, 30-39, 40-49, 50-59, and 60-69 years of age groups. In total, 640 study subjects were selected, and 64 males and females were included in each age group. Additionally, considering the differences in dietary intake of each region, 160 study subjects were selected from each of the following regions: the metropolitan, Chungcheong, Gyeongsang, and Jeolla regions of Korea. The volunteers were recruited by posting a study subject recruitment announcement on the websites of self-governing organizations of each region. Using the conformity assessment of study subjects, those diagnosed with or taking medications for hypertension, cardiac failure, diabetes, renal disease, cancer, or pregnant/breastfeeding women, and those under dietary control were excluded from the study. This study was approved by the Institutional Review Board of Kyungpook National University (IRB 2014-0053), and it was conducted after receiving written consent from study participants.
The height, weight, and blood pressure of the study subjects were measured. Briefly, the height of the subjects (with shoes removed) was measured using a stadiometer. The weight (with minimal clothing) was measured using a body composition analyzer (X-SCAN PLUS II, Biospace, Seoul, Korea). The body mass index (BMI) was calculated as the weight (in kilograms) divided by the squared height (in meters). The blood pressure was measured using an electronic automatic inflation sphygmomanometer (Microlife WatchBP Home 3MX1-1, Widnau, Switzerland) after the study subjects rested in a sitting position for 10 min. For smokers, the measurement was conducted at least 30 minutes after smoking. The blood pressure was measured once for most subjects, if the initial systolic blood pressure was greater than 140 mmHg or if the diastolic blood pressure was greater than 90 mmHg, it was re-measured again using the same method after resting. The study subjects with a blood pressure that did not fall within the normal blood pressure ranges, even after the second measurement, were excluded from the study.
The dietary intake of the study subjects was examined using the 24-hour dietary recall method. To expedite a recall interview, a diet record sheet was provided to the study subjects beforehand. Thus, the diet record was recorded exactly on the day of the dietary intake. Furthermore, the dietary examination was conducted during the working hours and excluded weekends and holidays. The 24-hour dietary recall interview was conducted using a direct interview with a dietitian based on a diet record sheet. To enhance the intake accuracy, supplementary tools, such as photo data of the meal, tapeline, and food replica, were used. The subjects were informed to take a photo of the meal during the dietary intake. Thus, the photos were used to produce a diet record sheet and during a 24-hour dietary recall interview. During the 24-hour dietary recall interview, the dietitian recorded the food name and intake quantity (approximate "by eye" measurement, volume, weight), the name and quantity of ingredients in the meal (approximate "by eye" measurement, volume, weight), and the product name and manufacturer were recorded for the processed food. Additionally, the dietary supplements and other functional health food intakes were recorded. The quantity of food intake on the same day was examined in comparison with an average food intake (selected from the following options: greater than usual intake, average intake, and less than usual intake). Moreover, the beverage intake quantities were examined for coffee and tea, and for other beverages, such as the bottled water and the caffeine-free beverages (barley tea, Gyeolmyeongja tea, and Dunggle tea). The nutrition intake was analyzed using a nutrition assessment program CAN-Pro 4.0 (Computer Aided Nutritional Analysis program version 4.0, Korea Nutrition Society, 2010) based on a 24-hour dietary recall examination result. The main database of the nutrition assessment program CAN-Pro 4.0 was created based on the National Standard Food Composition Table 7th edition [16]. Thus, it was recalculated to reflect the mineral content of the National Standard Food Composition Table 8th edition [17]. The subjects of this study consumed 1591 foods based on 24-hour dietary recall data. Regarding food intake, 59.2% and 44.5% of the items had information on copper and manganese contents in the database. The mineral content of foods not included in the mineral content database were calculated by replacing them with similar foods in the database.
The statistical analysis for the study was conducted using the SAS program (Ver. 9.4, SAS Institute Inc., Cary, NC, USA). Regarding the difference of variables for each age group, the post hoc analysis was conducted using Duncan's test when the significance was present after conducting the one-way ANOVA. The correlation between each variable was verified to determine its significance using Pearson's correlation test. Then, the partial correlation was conducted after adjusting for gender, age, BMI, and energy intake as potential confounding factors. The significance verification of all statistical analyses was conducted at a level of p < 0.05.
The general characteristics of the subjects are shown in Table 1. The average height was significantly getting lower with an increase of age both for men and women. The average weight of men was significantly getting higher before the age of 50 year-old and getting lower with aging in the age of above 50 year-old. However, the average weight of women was not significantly different among the age groups. However, there was a difference between women in their 20's and 60's (54.2 kg vs. 58.2 kg, p < 0.05). The average BMI was the highest for the men in their 40's, and it was significantly higher for women with an increase in age. The average systolic/diastolic blood pressure was 126.4/80.2 mmHg for men and 117.8/75.8 mmHg for women, and it was significantly higher with an increase in age both for men and women.
The daily energy, copper, and manganese intakes of the subjects are shown in Table 2. The daily energy intake was significantly lower with an increase in age both for men and women. The daily trace mineral intakes of the men and women were 1.3 mg (0.6 mg/1000 kcal, 156.7% of recommended intake) and 1.2 mg (0.7 mg/1000 kcal, 149.6% of recommended intake) for copper, and 4.2 mg (2.1 mg/1000 kcal, 105.2% of adequate intake) and 4.1 mg (2.3 mg/1000 kcal, 116.4% of adequate intake) for manganese, respectively. The daily intakes of copper and manganese were significantly high with an increase of age for men and women.
Table 3 shows the relation of the copper and manganese intake of the subjects to blood pressure. The copper intake was significantly and positively correlated with the systolic blood pressure in women and with the systolic and diastolic blood pressures in all subjects. However, the significant correlation between copper and the blood pressure disappeared after adjusting for potential confounding factors. Manganese intake was significantly and negatively correlated with the systolic blood pressure in men after adjusting for gender, age, BMI, and energy intake.
In this study, the daily copper and manganese intake was assessed in normotensive adults, and the correlation with blood pressure was analyzed. As a major result, the manganese intake of male subjects had a significantly negative correlation with the systolic blood pressure after adjusting for gender, age, BMI, and energy intake.
Recently, studies of the relation between oxidative stress and hypertension have been conducted. Oxidative stress accelerates proliferation of the vascular cells and causes blood vessel thickening and narrowing of their internal diameter. Additionally, oxidative stress damages the endothelium and increases vasoconstriction [181920]. These changes in blood vessels explains how oxidative stress causes hypertension. It is noted that an increase in blood pressure combined with obesity is related to oxidative stress such as the increase in lipid peroxidation, protein carbonylation, and the oxidative damage index of amino acids [21]. Therefore, it is proposed that an anti-oxidative prescription of medicine or nutrients lowers the oxidative stress and blood pressure. Although blood pressure lowering effects of the anti-oxidative vitamin supplements, such as vitamin C, vitamin E, and β-carotene, have been conducted [222324], the study of the anti-oxidative minerals is very limited.
Copper is a component of various enzymes. It is known as a co-enzyme of the anti-oxidant enzyme, superoxide dismutase (SOD) [25]. In addition, because copper is essential for normal cardiovascular functions, it has been reported that copper deficiency causes a heart abnormality and increases the blood pressure and serum lipids [2627]. In a study on the relation between copper and blood pressure, Klevay and Halas [28] reported that there was a blood pressure increase in copper deficient rats. In addition, Li et al. [29] reported a high oxidation index, a low anti-oxidant index and anti-oxidative nutrition intake among metabolic syndrome patients from 18 to 65 years of age. Specifically, the copper intake of the metabolic syndrome patients was 1.4 mg/day, which was significantly lower than 1.6 mg/day for a normal person. Although the risk of metabolic syndrome was significantly lower with a high copper intake, there was no significant correlation when adjusting for the age and sex. The copper intake had a significantly positive correlation with the blood pressure in this study, but the significant correlation disappeared after adjusting for sex, age, BMI, and energy intake. This result implies that the daily copper intake has no correlation with the blood pressure. It may be due to the fact that the subjects in this study were taking enough amounts of copper daily. Additional research including subjects with various intake levels of copper is required.
Manganese is necessary for the normal metabolism of amino acids, proteins, fats, and carbohydrates. Additionally, it is necessary for the normal function of enzymes, such as SOD. Furthermore, manganese is known to have anti-oxidative function [1430]. Although an excessive manganese intake is rare, it is known to cause toxicity in a case of excessive exposure by ingestion [31]. Most studies on the relation between manganese and blood pressure have been conducted from the perspective of manganese toxicity. Those studies reported that a high blood level of manganese, due to an excessive exposure to manganese, increased the blood pressure [323334]. Kostial et al. [35] reported that manganese increased blood pressure in an animal study. However, Šarić and Hrustić [36] reported that the blood pressure was low in manganese-exposed workers. Thus, the studies regarding the relation between manganese and blood pressure present conflicting results.
There are a limited number of studies on the relation between the manganese intake, as a nutrient or a trace mineral, and blood pressure. In our study, manganese intake, particularly in the male subjects, had a significantly negative correlation with the systolic blood pressure after adjusting for sex, age, BMI, and energy intake. Because our study is a cross-sectional study, it has a limitation. Specifically, it is difficult to explain the mechanism behind the correlation between manganese intake and blood pressure. However, it has been reported in several studies that an abnormal manganese level lowers the activation of manganese-SOD, which impedes anti-oxidative function of this enzyme and lowers the defense capacity of vascular endothelium dysfunction, and causes hypertension. Particularly this result was observed only in the males, which demonstrates a difference based on gender [3437]. Previous studies reported that an excessive exposure to manganese causes an abnormal change in the blood pressure. The results of our study presented a negative correlation between the daily manganese intake and blood pressure, and implicate that the anti-oxidative and vascular protective functions of manganese. Taken together, we suggest that the proper intake of manganese is essential to maintain a normal blood pressure.
In Korea, an adequate intake of manganese is set at 4.0 mg/day and 3.5 mg/day for the adult males and females, respectively [38]. The manganese intake of subjects in this study exceeded an adequate intake. In the present study, it was 4.2 mg/day and 4.1 mg/day for the males and females, respectively, and higher intake of manganese were shown in subject with older age than the other. Nkwenkeu et al. [39] reported that the manganese intake are 2.0-8.8 mg/day worldwide, 2.4 mg/day in USA, 2.9 mg/day in Canada, 2.7 mg/day in Germany, 2.4 mg/day in Spain, 2.6 mg/day in Belgium, 4.6 mg/day in England, 2.9 mg/day in Australia, and 2.2 mg/day in India. Because there is a high manganese content in grains, rice, nuts, and tea, it has been reported that a vegetarian diet or a vegetable-centered diet provides a high manganese intake of 13-20 mg/day [40]. Although the vegetable-centered diet of Korean traditionally provides a sufficient manganese intake, it is estimated that the manganese intake is low in younger generations due to the Westernized diet. In addition, this study has revealed that the manganese intake decreases with a decrease in age.
Because many studies investigate the relation between blood pressure and diet mainly focusing on the major minerals, there is a limited number of studies focusing on the trace minerals. Thus, our study is a pioneering study in the field which has explored the relation between copper and manganese intake and blood pressure and a significant result was obtained. In particular, the manganese intake had a significantly negative correlation with a systolic blood pressure.
This study has several limitations in generalizing its findings. First, limited methodology was used to investigate the mineral intakes of subjects as we carried out the 24-hour recall for only one day but food frequency records or repeated 24-hour recalls were not conducted [41]. Thus, it is possible that this research does not reflect the long-term mineral intake status of subjects. However, we used a mineral content database among the diverse food data to accurately assess the intake levels. And, the present Korea NHANES in which one-day 24-hour dietary recall method was utilized to investigate the various nutrient intake levels in Korean adults [2]. Second, this study cannot explain the mechanism behind the correlation between the manganese intake and the blood pressure because this is a cross-sectional study. To clarify the effect between the trace mineral intake and the blood pressure and to explain the mechanism, longitudinal studies including analyses of various biomarkers are necessary in the future.
The copper intake in normotensive adults from a normal meal was 1.3 mg (0.6 mg/1000 kcal) and 1.2 mg (0.7 mg/1000 kcal) for the males and females, respectively. The manganese intake was 4.2 mg (2.1 mg/1000 kcal) and 4.1 mg (2.3 mg/1000 kcal), respectively, which exceeded the adequate intakes. Specifically, the manganese intake of the male subjects had a significantly negative correlation with the systolic blood pressure after adjusting for gender, age, BMI, and energy intake. These results indicate a possibility of a positive effect of manganese intake on blood pressure.
Figures and Tables
Table 1
General characteristics and blood pressure of the subjects by gender and age
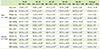
Table 2
Daily energy and nutrient intakes of the subjects by gender and age
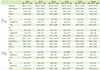
Table 3
Correlation between copper and manganese intakes and blood pressure of the subjects

References
1. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013; 1–8.
2. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2012: Korea National Health and Nutrition Examination Survey (KNHANES V-3). Cheongwon: Korea Centers for Disease Control and Prevention;2013.
3. Meneton P, Jeunemaitre X, de Wardener HE, MacGregor GA. Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiol Rev. 2005; 85:679–715.

4. Skrabal F, Auböck J, Hörtnagl H. Low sodium/high potassium diet for prevention of hypertension: probable mechanisms of action. Lancet. 1981; 2:895–900.

5. Bucher HC, Cook RJ, Guyatt GH, Lang JD, Cook DJ, Hatala R, Hunt DL. Effects of dietary calcium supplementation on blood pressure. A meta-analysis of randomized controlled trials. JAMA. 1996; 275:1016–1022.

6. Jee SH, Miller ER 3rd, Guallar E, Singh VK, Appel LJ, Klag MJ. The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials. Am J Hypertens. 2002; 15:691–696.

7. Bazzano LA, Green T, Harrison TN, Reynolds K. Dietary approaches to prevent hypertension. Curr Hypertens Rep. 2013; 15:694–702.

8. Bukkens SG, de Vos N, Kok FJ, Schouten EG, de Bruijn AM, Hofman A. Selenium status and cardiovascular risk factors in healthy Dutch subjects. J Am Coll Nutr. 1990; 9:128–135.

9. McDermott JH. Antioxidant nutrients: current dietary recommendations and research update. J Am Pharm Assoc (Wash). 2000; 40:785–799.

10. Grossman E. Does increased oxidative stress cause hypertension? Diabetes Care. 2008; 31:Suppl 2. S185–S189.

11. Vlad M, Caseanu E, Uza G, Petrescu M. Concentration of copper, zinc, chromium, iron and nickel in the abdominal aorta of patients deceased with coronary heart disease. J Trace Elem Electrolytes Health Dis. 1994; 8:111–114.
12. Singh RB, Gupta UC, Mittal N, Niaz MA, Ghosh S, Rastogi V. Epidemiologic study of trace elements and magnesium on risk of coronary artery disease in rural and urban Indian populations. J Am Coll Nutr. 1997; 16:62–67.

13. Klotz LO, Kröncke KD, Buchczyk DP, Sies H. Role of copper, zinc, selenium and tellurium in the cellular defense against oxidative and nitrosative stress. J Nutr. 2003; 133:1448S–1451S.

14. Klimis-Tavantzis DJ, Leach RM Jr, Kris-Etherton PM. The effect of dietary manganese deficiency on cholesterol and lipid metabolism in the Wistar rat and in the genetically hypercholesterolemic RICO rat. J Nutr. 1983; 113:328–336.

15. Davis CD, Ney DM, Greger JL. Manganese, iron and lipid interactions in rats. J Nutr. 1990; 120:507–513.

16. Rural Development Administration, National Rural Resources Development Institute (KR). Food composition table. 7th ed. Suwon: Rural Development Administration, National Rural Resources Development Institute;2006.
17. Rural Development Administration, National Institute Agricultural Sciences (KR). Food composition table. 8th rev. ed. Suwon: Rural Development Administration, National Institute Agricultural Sciences;2011.
18. Kerr S, Brosnan MJ, McIntyre M, Reid JL, Dominiczak AF, Hamilton CA. Superoxide anion production is increased in a model of genetic hypertension: role of the endothelium. Hypertension. 1999; 33:1353–1358.

19. Tanito M, Nakamura H, Kwon YW, Teratani A, Masutani H, Shioji K, Kishimoto C, Ohira A, Horie R, Yodoi J. Enhanced oxidative stress and impaired thioredoxin expression in spontaneously hypertensive rats. Antioxid Redox Signal. 2004; 6:89–97.

20. Ward NC, Croft KD. Hypertension and oxidative stress. Clin Exp Pharmacol Physiol. 2006; 33:872–876.

21. Dandona P, Mohanty P, Ghanim H, Aljada A, Browne R, Hamouda W, Prabhala A, Afzal A, Garg R. The suppressive effect of dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J Clin Endocrinol Metab. 2001; 86:355–362.

22. Duffy SJ, Gokce N, Holbrook M, Huang A, Frei B, Keaney JF Jr, Vita JA. Treatment of hypertension with ascorbic acid. Lancet. 1999; 354:2048–2049.

23. Ward NC, Hodgson JM, Croft KD, Burke V, Beilin LJ, Puddey IB. The combination of vitamin C and grape-seed polyphenols increases blood pressure: a randomized, double-blind, placebo-controlled trial. J Hypertens. 2005; 23:427–434.

24. Rumbold AR, Crowther CA, Haslam RR, Dekker GA, Robinson JS. ACTS Study Group. Vitamins C and E and the risks of preeclampsia and perinatal complications. N Engl J Med. 2006; 354:1796–1806.

25. Prohaska JR, Brokate B. Lower copper, zinc-superoxide dismutase protein but not mRNA in organs of copper-deficient rats. Arch Biochem Biophys. 2001; 393:170–176.

26. Medeiros DM, Bagby D, Ovecka G, McCormick R. Myofibrillar, mitochondrial and valvular morphological alterations in cardiac hypertrophy among copper-deficient rats. J Nutr. 1991; 121:815–824.

27. Bureau I, Lewis CG, Fields M. Effect of hepatic iron on hypercholesterolemia and hypertriacylglycerolemia in copper-deficient fructose-fed rats. Nutrition. 1998; 14:366–371.

28. Klevay LM, Halas ES. The effects of dietary copper deficiency and psychological stress on blood pressure in rats. Physiol Behav. 1991; 49:309–314.

29. Li Y, Guo H, Wu M, Liu M. Serum and dietary antioxidant status is associated with lower prevalence of the metabolic syndrome in a study in Shanghai, China. Asia Pac J Clin Nutr. 2013; 22:60–68.
30. Aschner JL, Aschner M. Nutritional aspects of manganese homeostasis. Mol Aspects Med. 2005; 26:353–362.

31. Butterworth RF, Spahr L, Fontaine S, Layrargues GP. Manganese toxicity, dopaminergic dysfunction and hepatic encephalopathy. Metab Brain Dis. 1995; 10:259–267.

32. Jiang Y, Zheng W. Cardiovascular toxicities upon manganese exposure. Cardiovasc Toxicol. 2005; 5:345–354.

33. Cowan DM, Zheng W, Zou Y, Shi X, Chen J, Rosenthal FS, Fan Q. Manganese exposure among smelting workers: relationship between blood manganese-iron ratio and early onset neurobehavioral alterations. Neurotoxicology. 2009; 30:1214–1222.

34. Chrissobolis S, Faraci FM. Sex differences in protection against angiotensin II-induced endothelial dysfunction by manganese superoxide dismutase in the cerebral circulation. Hypertension. 2010; 55:905–910.

35. Kostial K, Landeka M, Slat B. Manganese ions and synaptic transmission in the superior cervical ganglion of the cat. Br J Pharmacol. 1974; 51:231–235.

36. Šarić M, Hrustić O. Exposure to airborne manganese and arterial blood pressure. Environ Res. 1975; 10:314–318.

37. Taylor MD, Erikson KM, Dobson AW, Fitsanakis VA, Dorman DC, Aschner M. Effects of inhaled manganese on biomarkers of oxidative stress in the rat brain. Neurotoxicology. 2006; 27:788–797.

38. The Korean Nutrition Society. Dietary reference intakes for Koreans. 1st rev. ed. Seoul: The Korean Nutrition Society;2010.
39. Nkwenkeu SF, Kennedy G, Philippe S, Zayed J. Oral manganese intake estimated with dietary records and with direct chemical analysis. Sci Total Environ. 2002; 287:147–153.

40. Rubio C, Gutiérrez ÁJ, Revert C, Reguera JI, Burgos A, Hardisson A. Daily dietary intake of iron, copper, zinc and manganese in a Spanish population. Int J Food Sci Nutr. 2009; 60:590–600.

41. Jaceldo-Siegl K, Knutsen SF, Sabaté J, Beeson WL, Chan J, Herring RP, Butler TL, Haddad E, Bennett H, Montgomery S, Sharma SS, Oda K, Fraser GE. Validation of nutrient intake using an FFQ and repeated 24 h recalls in black and white subjects of the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2010; 13:812–819.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download