Abstract
The aim of this study was to compare the quality of life (QoL) depending on the postoperative survival period or nutritional status in gastric cancer patients. Surviving gastric cancer patients (n = 222) after the gastrectomy were included in the study at Soonchunhyang University Bucheon Hospital from April 2010 to August 2012. The Korean versions of the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) and a gastric cancer-specific module, the EORTC QLQ-STO22, were used to assess the QoL. The postoperative survival period of the patients fell into two groups; the less-than-1-year group or the more-than-1-year group, and the nutritional status of the patients fell into three groups by a score of patient generated-subjective global assessment (SGA)-A, B, and C. As a result, the rate of malnutrition was 34.5% in the less-than-1-year group and 19.8% in the more-than-1-year group, respectively. Score for the fatigue (p = 0.006), loss of appetite (p = 0.002), reflux (p = 0.027) and body image (p = 0.004) in which the QoL was significantly lower in the less-than-1-year group than in the more-than-1-year group. The score of QoL according to the nutritional status of all subjects, overall health status (p = 0.043), physical functioning (p = 0.016), fatigue (p = 0.006), pain (p = 0.028), loss of appetite (p = 0.017), reflux (p = 0.003), eating restriction (p = 0.002), anxiety (p = 0.010), and body image (p = 0.001) was significantly lower in the SGA-C group than in other SGA groups. These results suggest that the nutritional status of the gastrectomy patients with stomach cancer may impact on their QoL. It is necessary to to develop nutritional intervention to improve QoL in gastric cancer patients with postoperative malnutrition.
Cancer negatively affects the quality of life (QoL) owing to the disease itself but also adverse effects of cancer therapy and the possibility of relapse. The best treatment for gastric cancer is determined by the survival rate and the QoL in patient after the treatment. Therefore, many studies have continued to evaluate the QoL in cancer patients [1]. Gastric cancer is the second most common cancer in Korea and the first among Koream men [2]. From an early stage of cancer development, gastric cancer patients experience malnutrition and weight loss mainly due to loss of appetite and decrease in bowel function. In addition, there are considerable changes in the physical symptoms and emotional status depending on the timing and the method of the treatment. Since these conditions greatly affects the QoL, the demands on shortand long-term QoL assessment is getting increased [3]. In fact, studies on the QoL of Korean gastric patients have been conducted according to the type of reconstruction surgery, resection extent, and the status of long-term survival [456]. These studies have demonstrated that enhanced level of QoL with increasing survival rate of cancer patients was closely related with the treatment methods or conditions. Cancer recurrence is different for each type of cancer. Usually recurrence of gastric cancer is confirmed one year after surgery. On the other hand, the malnutrition rate in patients after gastrectomy is still high and several problems co-exist, including dumping syndrome, anemia, and nutrient malabsorption.
Therefore, it is very important to devlop a method to identify the malnutrition early and to improve nutritional status because it is directly linked to patient symptoms and the QoL [7]. However, studies that simultaneously assess the nutritional status and QoL are limited in Korea. Therefore, we conducted this study to help improve the QoL of gastric cancer patients by investigating the malnutrition rate of gastric cancer patients through the evaluation of nutritional status and the QoL, and to determine whether the QoL is different in gastric cancer patients depending on the postoperative survival period or nutritional status.
The subjects were 222 gastric cancer survivors who underwent gastrectomy at the Surgery Department of Soonchunhyang University Hospital, and had no evidence of relapse and no disease in other organs. The goal of the study was thoroughly explained to the patients, who then signed the consent form. The results were obtained through one-on-one interviews. Clinicopathological factors including disease stage, surgical methods, extent of resection, and chemotherapy status were investigated by using the medical records, and the nutritional status was evaluated by the score of patient generated-subjective global assessment (PG-SGA), which the attending dietitian of the gastric cancer surgical team commonly uses for cancer patients. Using the evaluation score, the nutritional status was divided into three stages (SGA-A: well nourished, SGA-B: moderate malnutrition, SGA-C: severe malnutrition). Korean versions of the European Organization for Research and Treatment of Cancer Core Questionnaire (EORTC) QLQ-C30 and the EORTC QLQ-STO22, corresponding to the gastric cancer module, were used to evaluate the QoL. The score was calculated by investigating 15 scales from the EORTC QLQ-C30 and 9 scales from the EORTC QLQ-STO22. In the EORTC QLQ-C30, the QoL is higher when the general health and functional scale score is higher, and the QOL is lower when the symptom scale score is higher. In the EORTC QLQ-STO22, the QoL is lower when the score of each category is higher. In this study, the postoperative survival period was divided into two groups (the less-than-1-year group and the more-than-1-year group) and the nutritional status into three groups (SGA-A, B, and C), and each indicator was analyzed comparatively. Statistical analysis for all data collected from the investigation were performed by using the SPSS program (ver. 18.0, SPSS Inc., Chicago, IL, USA). The Soonchunhyang University Medical School IRB approved the study protocol. The general information of the patients was presented as means and standard deviation, and the postoperative malnutrition rate was analyzed by using the chi-square test. Analysis of covariance (ANCOVA), adjusted for gender and follow up duration, was conducted for comparison of QoL between groups according to postoperative elapsed time period. Among the groups divided by the nutritional status, the differences of QoL were also tested by ANCOVA adjusted for extent of gastric resection which showed the significant differences. Then, post hoc comparison was performed among groups of different nutritional status. For all analyses, p < 0.05 was considered statistically significant.
A total of 222 patients participated in the study; the mean age was 54.9, with 68.9% men and 31.1% women. A group of the less-than-1-year of post-operation, with a mean survival duration of 8.6 month, had 116 (52.3%) patients, and a group of the more-than-1-year of post-operation, with a mean survival duration of 18.4 months, had 106 (47.7%) patients. When the final disease stage was classified according to the 6th Union for International Cancer Control (UICC), 120 (54.1%) patients had stage I and II while 102 (45.9%) patients had stage III and IV, showing no significant difference between the two groups. In terms of the surgical methods, 153 (68.9%) underwent laparoscopic surgery and 69 (31.1%) underwent laparotomy. Considering the resection extent, 168 (75.7%) received subtotal gastrectomy and 54 (24.3%) received total gastrectomy; adjuvant chemotherapy was administered to 78 patients (35.1%), and there was no significant difference in the distribution between the two groups (Table 1).
When indicators of nutritional status were compared between two groups of postoperative survival period, there was no difference in the serum albumin and hemoglobin levels, since these indicators were within the normal range in patient of both groups. The serum albumin level was significantly different after the surgery between two groups. The mean weight loss was 5.1% in the less-than-1-year group and 3.3% in the more-than-1-year group, and the difference was significant (p < 0.001). The pre-operative malnutrition rate for all subjects was 4.5%. After surgery, the rate of moderate malnutrition and the rate of severe malnutrition was 25.9% and 8.6% in the less-than-1-year group and 17.0% and 2.8% in the more-than-1-year group, respectively; thus, the malnutrition rate was significantly higher in the less-than-1-year group (p < 0.05) (Table 2).
The overall health status considering the EORTC QLQ-C30 was lower in the less-than-1-year group, but the difference between two groups was not significant. When the 15 functional scales were compared, although the QoL considering the physical, emotional, congnitive and social function categories was lower in the less-than-1-year group than in the more-than-10year group, the difference between two groups was not significant. In the 9 categories pertaining to symptom scales, the QoL considering fatigue, pain, sleep disorder, loss of appetite, diarrhea and finalcial difficulties was lower in the less-than-1-year group but the mean scores for nausea and vomiting were the same. On the other hand, the QoL considering the dyspnea was higher in the less-than-1-year group than in the more-than-10year group. Among those symptoms, the symptoms that reached statistical significance were fatigue (p < 0.01) and loss of appetite (p < 0.01), in which the QoL was significantly lower in the less-than-1-year group. The QoL considering all the 9 categories of the QLQ-STO22 was lower in the less-than-1-year group, but the result was significant for only two categories of reflux (p < 0.05) and body image (p < 0.01) (Table 3).
When we compared the QoL according to the nutritional status of all subjects, the overall health status was the highest for the well-nourished group (SGA-A) (p < 0.05). In terms of the functional scales, the QoL of the SGA-A and SGA-B groups was higher than that of the SGA-C group in the physical funtioning (p < 0.05). Regarding the symptom scales, the QoL was significantly lower in the SGA-C group than in the SGA-A group for considering the categories of fatigue (p < 0.01) and pain (p < 0.05), and the QoL was significantly lower in the SGA-C group than in the other two groups for considering the category of loss of appetite (p < 0.05). Considering most categories of the QLQ-STO22, SGA-C group has significantly lower QoL for reflux (p < 0.01), eating restriction (p < 0.01), anxiety (p < 0.05), and body image (p < 0.01) (Table 4).
The results from QoL studies in gastric cancer patients are diverse [489]. In studies of the QoL according to resection extent, patients who underwent partial resection showed a significant difference in the overall health status at 3 months after the surgery compared to the patients who underwent total resection [4]. In addition, the QoL was reported to be lower in patients whose diagnosed disease stage was higher and who underwent total resection [8], and the QoL was higher in patients who underwent laparoscopic surgery than in patients who underwent laparotomy [9]. In this study, when the QoL categories were evaluated according to the postoperative survival period, a significant difference was observed only in symptoms of fatigue, loss of appetite, reflux, and body image. This is somewhat different from the results reported by Park et al. [10], that the QoL score of both groups was lower than the mean score for overall health status and that significant differences were shown regarding the physical function, dyspnea, constipation, diarrhea, financial difficulties, loss of appetite, and body image between two groups.
The malnutrition rate of the subjects in our study was 34.5% in the less-than-1-year group but this number was decreased to 19.8% in the more-than-1-year group. This was slightly higher than the rate reported by Ryu & Kim [11] and similar to the result of Wu et al. [12]. As the postoperative nutritional status of patients are getting worse and manifested with weight loss and hypoalbuminemia even at 6 months after the surgery, continuous nutritional management is recommended [13]. From up to date studies which explored the relationship between the nutritional status and QoL are very rare. In a study by Seo et al. [14], there was no association between the QoL and nutritional indicators such as the total serum protein and albumin levels, prognostic nutrition index (PNI), and a body weight. Regarding nutrient intake, the group with a lower QoL had significantly less intake of nutrients such as proteins, iron, and zinc, and such a problem was more severe in women than in men; thus, a balanced nutrient intake is emphasized to improve the post-operative QoL [15]. In our study, the QoL was significantly lower in the SGA-C group than in the SGA-A group considering the overall health status including functional scales (physical functioning), and symptom scales (fatigue, pain, and loss of appetite) of the EORTC QLQ-C30, and the QoL in the SGA-C group was lower for considering reflux, eating restriction, anxiety, and body image scales of the QLQ-STO22. This is consistent with the results from other study for the nunutritional evaluation by using the nutritional risk screening (NRS) 2002, in which the QoL of the high-risk group with NRS ≥ 3 was significantly lower than that of other groups [16]. The association between the nutritional status and the QoL of cancer patients was well described in a study by Marín Caro et al. [17]. Therefore, as QoL markedly decreases when the nutritional status deteriorates, great efforts to prevent malnutrition to enhance early recovery from post-surgery need to be made.
This study has some limitations. Different recovery patterns among patients owing to variations in the elapsed time from the surgery could result in differences in QoL, but our classification might have been somewhat broad owing to a criterion value of 1 year. Unfortunately, QoL comparison or adjusting the results with the surgical method or range could not be performed. Though many studies has been performed to associate the surgical method and QoL, this study is still meaningful because the study involved nutritional evaluation methods commonly used by dietitians. The results of this study implicate the relationship between nutritional status and QoL. Therefore, these two indicators could be included in the management protocol of postoperative gastric cancer and also be utilized in the care system of long-term survivals from gastric cancer.
Our results indicate that the QoL of gastric cancer patients is getting lower with lesser elapsed time of post-gastrectomy and with a worsening of nutritional status. To improve the QoL when treating cancer, active nutritional management must be performed and continuous studies that integrate the effect of the long-term outcome and diet quality on the QoL are required.
Figures and Tables
Table 1
Clinicopathologic data according to the period of postoperative survival
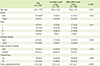
Table 2
Comparison of nutritional status according to the period of postoperative survival

Table 3
Comparison of quality of life according to the period of postoperative survival
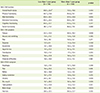
Table 4
Comparison of quality of life according to nutritional status

References
1. Ferrell BR, Wisdom C, Wenzl C. Quality of life as an outcome variable in the management of cancer pain. Cancer. 1989; 63:2321–2327.

2. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, Lee KH. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–141.

3. Yasuda K, Shiraishi N, Etoh T, Shiromizu A, Inomata M, Kitano S. Long-term quality of life after laparoscopy-assisted distal gastrectomy for gastric cancer. Surg Endosc. 2007; 21:2150–2153.

4. Park S, Chung HY, Lee SS, Kwon O, Yu W. Serial comparisons of quality of life after distal subtotal or total gastrectomy: what are the rational approaches for quality of life management? J Gastric Cancer. 2014; 14:32–38.

5. Kim AR, Cho J, Hsu YJ, Choi MG, Noh JH, Sohn TS, Bae JM, Yun YH, Kim S. Changes of quality of life in gastric cancer patients after curative resection: a longitudinal cohort study in Korea. Ann Surg. 2012; 256:1008–1013.

6. Lee JH, Kim YW, Ryu KW, Lee JR, Kim CG, Choi IJ, Kook MC, Nam BH, Bae JM. A phase-II clinical trial of laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for gastric cancer patients. Ann Surg Oncol. 2007; 14:3148–3153.

7. Horváth OP, Kalmár K, Cseke L, Pótó L, Zámbó K. Nutritional and life-quality consequences of aboral pouch construction after total gastrectomy: a randomized, controlled study. Eur J Surg Oncol. 2001; 27:558–563.

8. Rausei S, Mangano A, Galli F, Rovera F, Boni L, Dionigi G, Dionigi R. Quality of life after gastrectomy for cancer evaluated via the EORTC QLQ-C30 and QLQ-STO22 questionnaires: surgical considerations from the analysis of 103 patients. Int J Surg. 2013; 11:Suppl 1. S104–S109.

9. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, Bae JM. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.

10. Park JY, Eom BW, Jo MJ, Yoon HM, Ryu KW, Kim YW, Nam BH, Lee JH. Health-related quality of life after robot-assisted distal gastrectomy in early gastric cancer. World J Surg. 2014; 38:1112–1120.

11. Ryu SW, Kim IH. Comparison of different nutritional assessments in detecting malnutrition among gastric cancer patients. World J Gastroenterol. 2010; 16:3310–3317.

12. Wu GH, Liu ZH, Wu ZH, Wu ZG. Perioperative artificial nutrition in malnourished gastrointestinal cancer patients. World J Gastroenterol. 2006; 12:2441–2444.

13. Sungurtekin H, Sungurtekin U, Balci C, Zencir M, Erdem E. The influence of nutritional status on complications after major intraabdominal surgery. J Am Coll Nutr. 2004; 23:227–232.

14. Seo KS, Lee JM, Kim WY. Comparison of reconstructive techniques after total gastrectomy as determined by patient quality of life and nutritional status. J Korean Gastric Cancer Assoc. 2007; 7:219–227.

15. Tian J, Chen JS. Nutritional status and quality of life of the gastric cancer patients in Changle County of China. World J Gastroenterol. 2005; 11:1582–1586.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download