Abstract
Figures and Tables
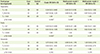
Table 1
Comparison of general characteristics between case and control groups

Table 2
Associations between macronutrients intakes and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45).
SFA: saturated fatty acid, MUFA: monounsaturated fatty acid, PUFA: polyunsaturated fatty acid, OR: odds ratios, CI: confidence intervals.
*p < 0.05; †p < 0.01.
Table 3
Associations between vitamin intakes and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake(in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year;20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber(in g/d; < 27.5, 27.5-45, or > 45).
RE: retinol equivalents, OR: odds ratios, CI: confidence intervals.
*p < 0.05; †p < 0.01; ‡p < 0.001.
Table 4
Associations between mineral intakes and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45)
OR: odds ratios, CI: confidence intervals.
*p < 0.05.
Table 5
Associations between intakes of grains and mixed foods and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45) and red meat (in serving/week; < 0.93, 0.93-2.7, or > 2.7).
OR: odds ratios, CI: confidence intervals.
*p < 0.05; †p < 0.01.
Table 6
Associations between intakes of meat·fish·eggs·beans and milk·dairy products and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45) and red meat (in serving/week; < 0.93, 0.93-2.7, or > 2.7).
OR: odds ratios, CI: confidence intervals.
*p < 0.01; †p < 0.001.
Table 7
Associations between intakes of fruits, vegetables, and seaweeds and colorectal cancer incidence
Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45) and red meat (in serving/week; < 0.93, 0.93-2.7, or > 2.7).
OR: odds ratios, CI: confidence intervals.
*p < 0.05; †p < 0.01
Table 8
Associations between intakes of lipids & sugars and beverage and colorectal cancer incidence

Multivariate model 1 OR (95% CI): Adjusted for energy intake (in kcal/d; < 1,620, 1,620-2,250, or ≥ 2,250), sex (male, female), age (in year; 20-29, 30-39, 40-49, 50-59, 60-69, or 70-79), household income (in 10,000 won; < 100, 100-200, 200-400, or ≥ 400), education (≤ elementary school, middle school, high school, ≥ university), smoking (none, ex/current), alcohol drinking frequency (in times/month; none, < 1, 1-3, 4-11, or ≥ 12), exercise frequency (in times/week; none, 1-3, or ≥ 4), BMI (in kg/m2; < 18.5, 18.5-22.9, 23-24.9, 25-29.9, or ≥ 30), Multivariate model 2 OR (95% CI): Adjusted for the variables included in the model 1 and dietary fiber (in g/d; < 27.5, 27.5-45, or > 45) and red meat (in serving/week; < 0.93, 0.93-2.7, or > 2.7).
OR: odds ratios, CI: confidence intervals.
*p < 0.05; †p < 0.01; ‡p < 0.001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download