Abstract
To investigate the possible risk factors related to macrosomia. Pregnant women and their newborns (n = 1041) were recruited from a cohort study in Maternal and Child Care Center of Hefei from January 2011 to July 2012. Questionnaires were applied to collect the demographic data besides the medical records. Detailed health records of the entire pregnancy were obtained using retrospective study. Meanwhile the data of neonatal outcomes was prospectively tracked. Associations between exposure risk factors and macrosomia were analyzed using Pearson's chi squared test. Logistic regression models were used to assess the independent association between these potential predictors and macrosomia. The incidence of macrosomia of this cohort was 11.24% of which male: female = 2.55:1. Male incidence (8.07%) of macrosomia was higher than female (3.17%), p < 0.001. Body mass index (BMI) before pregnancy (pre-BMI), maternal height, parity were not independently associated with macrosomia; multiple logistic regression analysis indicated that macrosomia was mainly independently associated with weight gain in pregnancy (OR=1.14, 95% CI [1.10-1.19]), maternal age (OR = 1.09, 95% CI [1.03-1.15]) and gestational age (OR = 1.62, 95% CI [1.31-1.99]), respectively. Our findings indicate that weight gain in pregnancy, maternal age and gestational age should be considered as independent risk factors for macrosomia.
With the rapid development of the society and economy, macrosomia, defined as neonates' birth weight ≥ 4000 g, has become more prevalent in affluent societies [1], which was mainly driven by an increase in maternal obesity and diabetes [2]. Pregnancies with large infants are associated with increased risk of complications for both the babies and their mothers. Oversized infants may suffer both short- and long-term consequences; the occurrence of these unfavorable outcomes and their risks factors has been widely studied, such as increasing risk of neonatal mortality, birth injury, adiposity, cardiovascular disease and cancer in later life [3,4,5,6]. Similarly, it also results in maternal complications genital tract trauma and postpartum bleeding [7,8,9]. The reasons for macrosomia are complex and insufficiently explained. Previous studies have shown some risk factors for macrosomia, including maternal obesity and pre-gestational diabetes, maternal BMI during pregnancy, maternal height, placental factors, maternal serum triglyceride (TG), gestational weight gain and other blood parameters [10,11,12,13,14].
Since attempts at perinatal diagnosis of macrosomia have proven to be difficult and are often inaccurate [6], an accurate diagnosis of macrosomia can be made only by measuring birth weight after delivery [2]. Accurate prediction of macrosomia and Large for Gestational Age (LGA) would allow for improved patient counseling regarding pregnancy risks. Meanwhile, few interventions currently exist for the treatment of high fetal growth. Accordingly, we conducted this retrospective study with healthy nondiabetic, and singleton pregnancies women to focus on risk factors after restricting our study to such normal mothers. The finding not only aid in the diagnosis of macrosomia some weeks earlier than normal but also even can help to reverse the mechanism of such problems by controlling the most independent important factors.
This study was approved by the biomedicine ethical committee of Anhui Medical University. Detailed health records of the entire pregnancy were obtained by using retrospective study and neonatal outcomes data was prospectively tracked at the Maternal and Child Health Care Center of Hefei from January 2011 to July 2012; In brief, a self-administered questionnaire, interview, and medical records were used to collect information on the maternal age at delivery, maternal height, maternal weight, pre-pregnancy weight, gestational weight gain, pre-pregnancy BMI, educational status, parity, gravidity, mode of delivery and blood parameters. Cases without heart disease, diabetic, epilepsy, hyperthyroidism, anomalous fetus, mental illness and family hereditary disease were enrolled and we restricted our analysis to cases who delivered a single live infant between 37 and 41 weeks of gestation in this study. Meanwhile, their neonates were also enrolled. Likewise, the detailed data of neonates were collected, including gestational age, birth height, head circumference, diameter at breast height (DBH) and gender of fetus. Data entry was routinely performed by two different people, respectively. The dataset was subject to rigorous quality checking and the quality control for the database was assessed. The gestational age was determined based on the menstrual history, the prenatal examination, and ultrasound findings during early pregnancy [14]. BMI was defined as kg/m2, and divided into underweight (BMI < 18.5 kg/m2), normal (BMI 18.5-24.9 kg/m2), overweight (BMI ≥ 24.9 kg/m2) groups [10]. Statistical analysis was performed using statistical software SPSS Statistics, version 16.0 (SPSS Inc., Chicago, IL, USA). The results were expressed as the means ± standard deviation (SD) or number (percentage). Birth weight was divided into normal weight group (birth weight < 4000 g) and macrosomia group (birth weight ≥ 4000 g). The 2-sample t-test was used to compare continuous variables and the chi-square test was used for categorical variables between macrosomia group and normal weight group. Logistic regression analysis was used to analysis the possible factors related to macrosomia. The significance level was set at < 0.05.
The general characteristics of the survey participants are shown in Table 1. A total of 1041 cases were included in this study; a total of 117 (11.24%) babies were macrosomia.
Compared with women delivered normal neonates, women with macrosomia neonates were significantly older in age (29.22 ± 4.32 y vs. 27.79 ± 4.23 y, p < 0.001), taller in body height (162.03 ± 4.13 cm vs. 160.94 ± 4.49 cm, p = 0.012), greater in body weight before pregnancy (56.35 ± 7.88 kg vs. 52.89 ± 6.93 kg, p < 0.001), pre-BMI (21.46 ± 2.70 kg/m2 vs. 20.36 ± 2.43 kg/m2, p < 0.001) and weight gain in pregnancy (19.89 ± 5.74 kg vs. 16.67 ± 4.90 kg, p < 0.001), as well as longer in gestational age (39.90 ± 0.92 w vs. 39.50 ± 1.05 w, p < 0.001), respectively. Women with macrosomia neonates were more likely to be multiparous and a male infant, and to experience a cesarean section or instrumental delivery. However, there was no significant difference in maternal TG, fasting blood glucose (FBG), total cholesterol (TC), high-density lipoprotein (HDL) and low-density lipoprotein (LDL) between two groups in this study, as shown in Table 1.
The changes in neonatal relation to macrosomia, such as neonatal height, head circumference, and DBH were also assessed in this survey. As a result, we found neonatal DBH, height, and head circumference have a positive effect on the incidence of macrosomia.
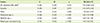
In order to investigate potential risk factors that related to macrosomia, univariate logistic regression analysis was applied, and indicated that maternal age was a risk factor for macrosomia (OR = 1.08, 95% CI [1.03-1.12]). Other risk factors for macrosomia included gestational age (OR = 1.46, 95% CI [1.21-1.77]), weight gain in pregnancy (OR = 1.13, 95% CI [1.09-1.18]), maternal height (OR = 1.06, 95% CI [1.01-1.10]), parity (OR = 1.62, 95% CI [1.04-2.54]), gravidity (OR = 1.59, 95% CI [1.05-2.42]), pre-pregnancy weight (OR = 1.06, 95% CI [1.04-1.09]), and pre-pregnancy BMI (OR = 1.53, 95% CI [1.05-2.23]), respectively. Data was shown in Table 2.
In order to identify the possible risk factors related to macrosomia, multiple logistic regression model was conducted. When we entered all former variables with enter method except for height and weight, since BMI was defined as kg/m2; three variables were found independently related to macrosomia: maternal age (OR = 1.09, 95% CI [1.03-1.15]), gestational age (OR = 1.62, 95% CI [1.31-1.99]), and weight gain in pregnancy (OR = 1.41, 95% CI [1.10-1.19]), respectively. The results were shown in Table 3.
In this study, we evaluated the possible factors which may related to macrosomia. Our data indicated that maternal age, gestational age and weight gain during pregnancy were independent risk factors for delivering a macrosomia neonate among normal women. The prevalence of macrosomia was different in different place, range from 0.5%-14.9% in Asia [1]. Although a previous study has shown maternal TG in the first half of pregnancy (early second trimester) was associated with macrosomia [11], we could not find a statistically significant difference in this study (p = 0.099). In a Japanese study [14], maternal age, maternal height, weight gain during pregnancy, pre-pregnancy BMI, the use of in vitro fertilization, induction of labor, and gestational duration were related to an increased BW. The gestational duration is the most important factor affecting the BW in singleton term infants, which is consistent with the present study. Another similar study found that placental weight was also associated with macrosomia, perhaps due to continuous fetal growth and aging of the placenta. On the other hand, gestational diabetes was not independently associated with fetal macrosomia in Clausen et al.'s study [15]. Interestingly, in another study, the results indicated pre-gestational diabetes was independently associated an increased risk of neonatal LGA delivery [16]. It is recognized now that pre-pregnancy BMI and gestational weight gain depend on different metabolic pathways. Pre-pregnancy BMI represents maternal nutritional conditions before conception, while gestational weight gain is the expression of fetal-maternal physiological changes combined with genetic and nutritional factors. In our study, multiple logistic regression analysis indicated that pre-pregnancy BMI was not independently related to neonate macrosomia (OR = 1.44, 95% CI [0.96-2.62], p = 0.079), but weight gain in pregnancy was independently related to neonate macrosomia. Sunsaneevithayakul et al. have recommended optimal gestational weight gain for each pre-pregnancy BMI category as follows: 10-18 kg for the underweight group, 8-16 kg for the normal weight group, 6-14 kg for the overweight group, and 4-8 kg for the obese group [10]. Excessive weight gain was associated with an OR of 3.3 for macrosomia. In another study, maternal triglyceride levels may be a significant predictor of fetal size in late pregnancy but not in early pregnancy [17]. Also, it was found that maternal food intake at the end of pregnancy was not a significant determinant of fetal macrosomia as compared to maternal BMI at term of pregnancy [18]. Previous studies have documented the relationship between fetal macrosomia and the risk of caesarean delivery despite the use of different thresholds for defining fetal macrosomia [19], which was consistent with ours. A study carried out on a large cohort of pregnant women suggested that suboptimal glycemic control could be an important risk factor for the development of macrosomia, independently of prepregnancy BMI [20], but we have not found any statistical difference in this study (OR = 0.997, 95% CI [0.94-1.06], p = 0.927, data are not shown).
Compared with previous studies we have a very homogenous sample without diabetes, preterm labor, heart disease, epilepsy, hyperthyroidism, an anomalous fetus, and mental illness. Therefore, our findings are more applicable in genral population. There are some limitations in this study. First, the number of our participants was not large enough, which may have effluence on the statistical results compared with previous studies, especially for maternal FBG, TG and other blood parameters in relation to neonatal macrosomia. These factors could be compensated with more study cases added by different study groups. Since we selected one hospital to enroll the participants and collect information, regional differences may present.
Our findings indicate that weight gain in pregnancy, maternal age, and gestational age should be considered as independent risk factors for newborn macrosomia. Intervention, such as counseling on dietary habits leading to a lesser net weight gain may be considered. Namely, weight gain during pregnancy, is more manageable by dietary counseling and lifestyle modification.
Figures and Tables
Table 1
Basic characteristic of 1041 mothers and their neonates

Table 2
Risk factors of macrosomia: results of the univariate logistic regression analysis
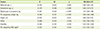
Table 3
Independent risk factors for macrosomia as determined by a multiple logistic regression analysis
Acknowledgements
The authors thank the mothers and their lovely babies who participated in the study, the staff and their colleagues working in the Maternal and Child Health Care Center of Hefei for help in recruitment, data and blood sample collection. C. L. Hu and L. Li were responsible for obtaining funds and supervision and had primary responsibility for the final content. All authors read and approved the final manuscript. This work was supported by grants from the National Natural Science Foundation of China (Grant Numbers 81373011) and Dietary Nutrition Research and Mission Fund of Danone Institution (DIC2014-08) and the Higher Education Department of Anhui Provincial Natural Science Research Project (KJ2012A158).
References
1. Koyanagi A, Zhang J, Dagvadorj A, Hirayama F, Shibuya K, Souza JP, Gülmezoglu AM. Macrosomia in 23 developing countries: an analysis of a multicountry, facility-based, cross-sectional survey. Lancet. 2013; 381:476–483.

2. Henriksen T. The macrosomic fetus: a challenge in current obstetrics. Acta Obstet Gynecol Scand. 2008; 87:134–145.

3. Azadbakht L, Kelishadi R, Saraf-Bank S, Qorbani M, Ardalan G, Heshmat R, Taslimi M, Motlagh ME. The association of birth weight with cardiovascular risk factors and mental problems among Iranian school-aged children: the CASPIAN-III study. Nutrition. 2014; 30:150–158.

4. Walsh JM, Kandamany N, Ni Shuibhne N, Power H, Murphy JF, O'Herlihy C. Neonatal brachial plexus injury: comparison of incidence and antecedents between 2 decades. Am J Obstet Gynecol. 2011; 204:324.e1–324.e6.

5. Lahmann PH, Gullberg B, Olsson H, Boeing H, Berglund G, Lissner L. Birth weight is associated with postmenopausal breast cancer risk in Swedish women. Br J Cancer. 2004; 91:1666–1668.

6. Ezegwui HU, Ikeako LC, Egbuji C. Fetal macrosomia: obstetric outcome of 311 cases in UNTH, Enugu, Nigeria. Niger J Clin Pract. 2011; 14:322–326.

7. Fuchs F, Bouyer J, Rozenberg P, Senat MV. Adverse maternal outcomes associated with fetal macrosomia: what are the risk factors beyond birthweight? BMC Pregnancy Childbirth. 2013; 13:90.

8. Boulet SL, Salihu HM, Alexander GR. Mode of delivery and birth outcomes of macrosomic infants. J Obstet Gynaecol. 2004; 24:622–629.

9. Stotland NE, Caughey AB, Breed EM, Escobar GJ. Risk factors and obstetric complications associated with macrosomia. Int J Gynaecol Obstet. 2004; 87:220–226.

10. Sunsaneevithayakul P, Titapant V, Ruangvutilert P, Sutantawibul A, Phatihattakorn C, Wataganara T, Talungchit P. Relation between gestational weight gain and pregnancy outcomes. J Obstet Gynaecol Res. 2014; 40:995–1001.

11. Schwartz N, Quant HS, Sammel MD, Parry S. Macrosomia has its roots in early placental development. Placenta. 2014; 35:684–690.

12. Mossayebi E, Arab Z, Rahmaniyan M, Almassinokiani F, Kabir A. Prediction of neonates' macrosomia with maternal lipid profile of healthy mothers. Pediatr Neonatol. 2014; 55:28–34.

13. Alberico S, Montico M, Barresi V, Monasta L, Businelli C, Soini V, Erenbourg A, Ronfani L, Maso G. Multicentre Study Group on Mode of Delivery in Friuli Venezia Giulia. The role of gestational diabetes, prepregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. 2014; 14:23.

14. Terada M, Matsuda Y, Ogawa M, Matsui H, Satoh S. Effects of maternal factors on birth weight in Japan. J Pregnancy. 2013; 2013:172395.

15. Clausen T, Burski TK, Øyen N, Godang K, Bollerslev J, Henriksen T. Maternal anthropometric and metabolic factors in the first half of pregnancy and risk of neonatal macrosomia in term pregnancies. A prospective study. Eur J Endocrinol. 2005; 153:887–894.

16. Ehrenberg HM, Mercer BM, Catalano PM. The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol. 2004; 191:964–968.

17. Yadav H, Lee N. Factors influencing macrosomia in pregnant women in a tertiary care hospital in Malaysia. J Obstet Gynaecol Res. 2014; 40:439–444.

18. Denguezli W, Faleh R, Fessi A, Yassine A, Hajjaji A, Laajili H, Sakouhi M. Risk factors of fetal macrosomia: role of maternal nutrition. Tunis Med. 2009; 87:564–568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download