Abstract
Wheat is a common cause of food allergy. Wheat-induced anaphylaxis (WIA) and wheat-dependent exercise induced anaphylaxis (WDEIA) are severe forms of immunoglobulin E (IgE) mediated allergic reaction to wheat protein. As the diagnosis of WIA or WDEIA is not easy because of the risk of oral challenge, identification of specific IgE of various wheat proteins is helpful for diagnosis. In Korea, there are only a few reports on WIA in adults. We report six cases of WIA diagnosed on the basis of clinical history and specific IgE of wheat proteins or provocation test. For immunologic evaluation of severe wheat allergy including WIA and WDEIA, it is important to measure specific IgE to each component of wheat including gluten and ω-5 gliadin not just measuring wheat-specific IgE.
Wheat is a major staple of the diet worldwide and wheat allergy is defined as an adverse immunologic reaction to wheat protein [1]. Depending on the route of exposure and the underlying immunologic mechanisms, wheat allergy are diagnosed as different forms of allergic diseases such as classic food allergy, food-dependent exercise-induced anaphylaxis (FDEIA), occupational asthma, rhinitis or contact urticaria [2]. IgE mediated allergy to wheat may be presented with various severity from simple urticaria to anaphylaxis. In Korea, only a few studies on wheat-induced anaphylaxis (WIA) have been performed [3,4]. We herein report six cases of severe wheat allergy including WIA and wheat-dependent exercise-induced anaphylaxis (WDEIA).
We reviewed three cases of WIA and three cases of WDEIA. All the patients visited our allergy clinic for the evaluation of symptoms such as urticaria, dyspnea, or syncope. History taking revealed that they ate wheat-containing foods before their symptoms had started. The clinical characteristics of the patients are shown in Table 1. Their ages ranged from 29 to 65 years and mean ± standard deviation (SD) of age was 45 ± 14 years. The mean ± SD of the patient's age at the onset of the symptoms was 38 ± 10 years (from 27 to 55 years). One patient with WIA and two patients with WDEIA were males and the others were females. All patients with WIA had combined allergic diseases and only one patient with WDEIA had allergic rhinitis. There was no patient who took aspirin or NSAIDs which might enhance food induced anaphylaxis.
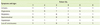
The patient's symptoms of anaphylaxis are presented in Table 2. All six patients had skin manifestation, such as urticaria (100%) and 4 of 6 had angioedema. Five patients had respiratory symptoms such as wheezing or dyspnea, and only one patient with WIA had gastrointestinal symptoms. All patients showed hypotension during the events of anaphylaxis and 4 patients had experienced loss of consciousness.
The mean ± SD of the level of total IgE was 512.20 ± 668.86 IU/mL. The levels of total serum IgE were higher than normal range in 4 patients. Total serum IgE was not evaluated in one patient (No. 3) and another patient showed normal level of total serum IgE (No. 5, 94 IU/mL). Wheat-specific IgE detected by ImmunoCAP (UniCAP PHAD®, Pharmacia & Upjohn, Uppsala, Sweden) showed class 1 in two patients and class 2 in the other two patients. Gluten-specific IgE was increased as class 2 in 3 patients (2 WIA and 1 WDEIA) and as class 3 in 2 patients (1 WIA and 1 WDEIA). ω-5 gliadin-specific IgE was increased in 4 patients, class 3 in 3 patients (1 WIA and 2 WDEIA) and class 4 in one patient with WIA. The levels of gluten or ω-5 gliadinspecific IgE were higher than wheat-specific IgE in all six patients. The details are shown in Table 3.
Skin prick test was conducted in 3 patients with WDEIA. The patients showed a positive response in skin prick test with wheat as shown in Table 4. All of them had positive results for skin prick tests for other foods: one patient (No. 4) also had a history of urticaria with seafood. Another patient (No. 5) was diagnosed as oral allergy syndrome. In addition, those with WDEIA had positive skin prick test for common inhalant allergens.
While 5 patients were diagnosed on the basis of repeated histories and specific IgE to wheat proteins, one patient (No. 5) suspected as having WDEIA underwent an exercise provocation test 30 minutes after eating wheat-containing food. Within 5 minutes after 6 minutes free running, the patient developed generalized itching and urticaria. At 15 minutes, the patient complained of dyspnea and presented with hypotension (systolic blood pressure 63 mmHg). Symptoms were resolved gradually after treatment, with restoration of normal vital signs and physical examination findings.
The three patients with WIA were advised the life-long avoidance of wheat containing products and the others with WDEIA were taught to avoid wheat-containing food, and importantly to avoid exercise for at least six hours when they accidentally ate wheat-containing food. They were prescribed Epipen® by the allergists in our clinic.
Food allergy is increasing and the prevalence of food allergy is estimated to be 6-8% of children and 1-3% of adults [5]. Wheat is an important part of human diet and one of the six most common foods causing allergy [6]. Depending on the route of allergen exposure and the underlying immunologic mechanisms, wheat allergy may appear as classic food allergy affecting the skin, gut, or respiratory tract; exercise-induced anaphylaxis; occupational asthma and rhinitis; or contact urticaria. In addition, ingestion of wheat gluten may cause celiac disease (T-cell-mediated intestinal inflammation), or dermatitis herpetiformis (blistering skin eruption). With the exception of the latter two, specific IgE to wheat proteins play a central role in all of the above [1].
Despite the high prevalence of wheat allergy in children, relatively little is known about its natural history. The natural course of only a few patients with wheat allergy has been reported in the literature, and in these studies 25% to 35% of patients became tolerant in a 1- to 2-year period [6]. In the study by Keet et al. [7], 35% of the children who had wheat allergy remained allergic during their teenage years. In some cases, it may lead to exacerbation of atopic dermatitis and gastrointestinal symptoms. A unique form of allergy, WDEIA, develops predominantly in young adults and adolescents [8]. A few cases of WIA, which were enhanced by aspirin or nonsteroidal anti-inflammatory drugs, have been reported in adult patients [9]. Recently, it has also been reported that FDEIA could be dependent on the temperature [10]. In this study, all of the cases of WIA were adult-onset and 4 (67%) of the patients had co-morbid allergic diseases. Most of them experienced urticaria, respiratory symptoms and hypotension during the events, but only one patient had gastrointestinal symptom. Four of the 6 patients showed increased levels of total IgE than normal range and 3 patients with WDEIA had positive responses to skin prick test with common food allergen and aeroallergens.
Because of the difficulty of strict wheat avoidance, complete diagnosis for the patients who were suspected wheat allergy is critical. To diagnose WIA or WDEIA, food challenge test with wheat or exercise challenge test following wheat ingestion should be performed. However, the provocation test is time-consuming and has a risk of inducing anaphylaxis. On top of that, the amount of food and the degree of exercise vary. Thus, in vitro diagnostic test for predicting severe systemic reactions is desirable. Considering the risk of food challenge tests in patients with a history of anaphylaxis, in vitro tests using ImmunoCAP could be a useful method in clinical practice with definite history of anaphyalxis [4].
Wheat proteins are classified depending on the basis of their solubility in a series of solvents: water (albumins), dilute salt solutions (globulins), aqueous alcohol (gliadins), and dilute alkali or acid (glutenins) [2]. Classic food allergy and atopic dermatitis are related to a wide range of water/salt-soluble and insoluble wheat proteins [11]. WDEIA is usually known to be associated with gluten, particularly ω-5 gliadin and high-molucular-weight (HMW) glutenin subunits [12]. Although most recent studies suggested major roles of HMW glutenin subunits and ω-5 gliadin in WIA and WDEIA [13], low molecular weight (LMW) glutenin subunits are also known to be involved in immediate type childhood and adult wheat allergies, including WDEIA [11]. In the study by Park et al., 17 subjects with WIA or WDEIA showed strong positive specific IgE response to ω-5 gliadin allergens, but not to wheat, indicating that ω-5 gliadin is the causative allergen in adults with WIA [4]. Using the log-transformed specific IgE ratio of ω-5 gliadin to wheat, they found 100% sensitivity and specificity distinguishing patients with severe wheat allergy, such as WDEIA or WIA, from patients with other forms of wheat allergies in the 27 subjects. All of the patients in our cases also showed stronger specific IgE response to ω-5 gliadin than the response to wheat.
In Korea, only a few studies reported the cases of wheat-induced anaphylaxis in adults. We report six cases of wheat-induced anaphylaxis diagnosed on the basis of clinical history and specific IgE of wheat proteins or provocation test. For immunologic evaluation of severe wheat allergy including WIA and WDEIA, it is important to measure specific IgE to each component of wheat including gluten and ω-5 gliadin rather than measuring wheat-specific IgE.
Figures and Tables
References
3. Lee HB, Ahn IS, Choi JH, Park CW, Lee CH. A case of wheat-dependent exercise-induced anaphylaxis. Ann Dermatol. 2009; 21:447–449.

4. Park HJ, Kim JH, Kim JE, Jin HJ, Choi GS, Ye YM, Park HS. Diagnostic value of the serum-specific IgE ratio of omega-5 gliadin to wheat in adult patients with wheat-induced anaphylaxis. Int Arch Allergy Immunol. 2012; 157:147–150.

5. Sotkovský P, Sklenář J, Halada P, Cinová J, Setinová I, Kainarová A, Goliáš J, Pavlásková K, Honzová S, Tučková L. A new approach to the isolation and characterization of wheat flour allergens. Clin Exp Allergy. 2011; 41:1031–1043.

6. Sampson HA, Scanlon SM. Natural history of food hypersensitivity in children with atopic dermatitis. J Pediatr. 1989; 115:23–27.

7. Keet CA, Matsui EC, Dhillon G, Lenehan P, Paterakis M, Wood RA. The natural history of wheat allergy. Ann Allergy Asthma Immunol. 2009; 102:410–415.

8. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, Kwon HS, Park CH, Park HW, Kim SS, Cho SH, Min KU, Kim YY, Chang YS. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36.

9. Matsukura S, Aihara M, Sugawara M, Kunimi Y, Matsuki M, Inoue Y, Kambara T, Ikezawa Z. Two cases of wheat-dependent anaphylaxis induced by aspirin administration but not by exercise. Clin Exp Dermatol. 2010; 35:233–237.

10. Jo EJ, Yang MS, Kim YJ, Kim HS, Kim MY, Kim SH, Cho SH, Min KU, Chang YS. Food-dependent exercise-induced anaphylaxis occurred only in a warm but not in a cold environment. Asia Pac Allergy. 2012; 2:161–164.

11. Pastorello EA, Farioli L, Conti A, Pravettoni V, Bonomi S, Iametti S, Fortunato D, Scibilia J, Bindslev-Jensen C, Ballmer-Weber B, Robino AM, Ortolani C. Wheat IgE-mediated food allergy in European patients: alpha-amylase inhibitors, lipid transfer proteins and low-molecular-weight glutenins. Allergenic molecules recognized by double-blind, placebo-controlled food challenge. Int Arch Allergy Immunol. 2007; 144:10–22.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download