Abstract
Pancreatic cancer patients often have a poor prognosis and suffer from nutritional problems. Malnutrition is characterized by weight loss and decreased dietary intake, and is common among pancreatic cancer patients. The objective of this report was to describe the changes in dietary intake, body weight, nutritional status, and metabolic rate on a continuum from the time of diagnosis until the end of life in a patient with pancreatic cancer. In summary, the patient's nutritional status gradually declined, accompanied by extreme weight loss and decreased dietary intake. Conversely, resting energy expenditure, measured by indirect calorimetry, increased from 24 kcal/kg/day to 35 kcal/kg/day. Nutritional management during cancer treatment is important but may be challenging in pancreatic cancer patients.
Pancreatic cancer generally has a poor prognosis and is often diagnosed at advanced stages, making treatment very difficult [1]. More than 80% of patients with pancreatic cancer suffer from significant weight loss at the time of diagnosis [2]. These patients also report various nutrition-related symptoms such as abdominal pain, anorexia, early satiety, anxiety, nausea, vomiting, and diarrhea or constipation [3-5]. Medical care for unresectable pancreatic cancer focuses on symptom management to improve the patient's quality of life (QOL) [6].
Weight stabilization in cases of unresectable pancreatic cancer is associated with improved survival duration and QOL [6]. However, interventions to prevent weight loss have received little or no attention. In terms of energy balance, the progressive wasting could be attributed to changes in dietary intake and/or energy expenditure, which are mediated by metabolic alterations [7]. Although reduced dietary intake is a known problem in cases of progressive cancer, few reports have quantitatively measured dietary intake in pancreatic cancer patients. The metabolic rate among pancreatic cancer patients also remains unclear [7,8].
The purpose of this case report on a patient with pancreatic cancer was to review the changes in dietary intake, body weight, nutritional status, and metabolic rate on a continuum from the time of diagnosis until the end of life. This study was approved by the Institutional Review Board of the National Cancer Center (NCC-CTS-11-570), and written informed consent was obtained from the patient.
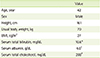
A 42-year-old man diagnosed with pancreatic head cancer at another hospital was referred to our hospital for a second opinion. For further evaluation, the patient underwent a biopsy that yielded positive results for malignant cells. The patient was in good health except for hypercholesterolemia. However, the patient complained of fatigue, dyspepsia, and nausea and developed jaundice. The patient's total bilirubin level was 10.6 mg/dL. Other blood test indices were as follows: albumin, 4.0 g/dL; total cholesterol, 288 mg/dL; and glycosylated hemoglobin (HbA1c), 6.1% (Table 1).
Nutrition consultation was regularly provided by a registered dietitian. Nutritional status was assessed using the scored Patient-Generated Subjective Global Assessment (PG-SGA) at diagnosis, as well as at 2 and 3 months after the diagnosis. Dietary intake was evaluated using 3-day food records. Measured resting energy expenditure (measured REE) was assessed using indirect calorimetry (TrueOne2400; Parvo Medics, Utah, USA), while predicted resting energy expenditure (predicted REE) was calculated using the Harris-Benedict equation at the time of diagnosis and 2 months later. To increase the accuracy of the food records, a trained registered dietitian confirmed all of the records written by the caregiver using face-to-face interviews. The daily intakes of energy and nutrients were calculated using the CAN-pro 3.0 (Korean Nutrition Society, Korea). The main caregiver was a family member (a sister) who assisted with the nutritional assessment by recording the patient's dietary intake.
The patient's height was 161 cm and usual body weight was 70 kg. At diagnosis, the patient's measured REE was 1,707 kcal/day (24.4 kcal/kg/day), while the predicted REE was 1,545 kcal/day (22.1 kcal/kg/day). The patient usually consumed 3 meals a day and sometimes had constipation, but this had no effect on the patient's dietary intake. The mean energy intake was 1,887 kcal/day (27.0 kcal/kg/day), and the mean protein intake was 56 g/day (0.8 g/kg/day). Because the patient was an outpatient at this time, no parenteral nutrition was provided. The ratio of carbohydrates to proteins to lipids was 70:12:18. The patient's weight was stable at 70 kg. According to the PG-SGA, the patient was classified as well nourished (SGA-A) with a PG-SGA score of 2. Physical examination of the subcutaneous fat, muscle mass, and fluid balance did not reveal any depletion in the subcutaneous fat or muscle (Table 2).
The patient was encouraged to divide his daily energy intake over 6 meals: 3 main meals and 3 snacks between meals that included various food items for a well-balanced diet. No strict rules or prohibitions with respect to dietary intake were imposed. The patient received pancreatic enzyme replacement therapy in combination with dietary counseling to maintain his weight and improve the QOL. The patient received concurrent chemo-radiation therapy (CCRT) with 5-fluorouracil (5-FU) after he recovered from hyperbilirubinemia. The patient's weight was stable during the first CCRT.
At the 2-month follow-up after diagnosis, the patient's weight was almost stable at 69 kg. However, the patient reported having a poor appetite and epigastric pain. At this time, the patient intended to reduce his food intake as a result of decreased physical activity. The patient's energy intake decreased to 1,060 kcal/day (15.4 kcal/kg/day), and the protein intake also decreased to 30 g/day (0.44 g/kg/day). Because the patient was an out-patient at this time, no parenteral nutrition was provided. The ratio of carbohydrates to proteins to lipids was 78:11:11. Conversely, the measured REE of the patient increased to 2,416 kcal/day (35.0 kcal/kg/day), while the predicted REE remained stable (1,531 kcal/day). There was no depletion in the subcutaneous fat or muscle. The patient's daily functioning was also good, and the patient was still considered as well nourished (SGA-A), but the PG-SGA score increased to 8. Nutritional education was conducted to encourage dietary intake in order to prevent further deterioration of his nutritional status.
At the 3-month follow-up after diagnosis, the patient was readmitted for a pancreatectomy and was classified as being moderately malnourished or with suspected malnutrition (SGA-B). The PG-SGA score was 8. The patient's weight decreased to 68 kg, and the serum albumin level was 4.1 g/dL. After the total pancreatectomy, the patient was diagnosed with diabetes mellitus and received insulin therapy along with diet education for blood glucose control. The patient reported symptoms such as constipation, poor appetite, and abdominal pain. The frequency of the patient's dyspepsia also increased, which contributed to a decrease in food intake to 500-1,000 kcal/day. A dietitian advised the patient and his caregiver to consume frequent small meals and provided tips for the treatment and prevention of hypoglycemia.
When the patient was discharged, the patient could only consume a very minimal amount of solid food, as the patient was experiencing severe pain and dyspepsia. The patient had several hypoglycemic events; hence, the insulin dosage was reduced. Dietary intake, especially of solid food, continued to decrease. A dietitian provided detailed explanations on food preparation skills to the caregiver in order to increase the nutrition density in food and to prepare a balanced liquid diet.
At the 8-month follow-up after diagnosis, positron emission tomography (PET) findings suggested a recurrence around the superior mesenteric artery with aortocaval lymph node metastasis. While chemotherapy commenced, the patient continued to have poor oral intake, and a dietitian met the patient's caregiver to introduce an oral nutrition supplement. However, the patient's weight was 55 kg and continuously decreased to 49 kg at the last chemotherapy treatment.
At the 11-month follow-up after diagnosis, the patient could not meet the dietitian due to his poor health. Medical care for the patient focused on supportive care due to the advanced stage of the disease and treatment-refractory disease progression. The last weight measurement showed a 15 kg weight increase over a 2-week period due to the accumulation of ascites. The patient was referred to a hospice for end-of-life care.
Malnutrition characterized by weight loss and decreased dietary intake is common among pancreatic cancer patients. The etiology of cancer malnutrition may be multifactorial and is not fully understood [2]. In our case, the patient's nutritional status gradually deteriorated and body weight decreased from 70 kg to 49 kg (30%), as the dietary intake decreased. Conversely, the measured REE increased from 24 kcal/kg/day to 35 kcal/kg/day.
As inadequate nutrient intake contributes to weight loss and may result in decreased response rates to antineoplastic therapy, performance status, and chances of survival [8], it is imperative to find ways to provide adequate nutrition. One of the most important and first steps while creating a nutritional support plan is to assess the patient's energy requirement. Measuring energy expenditure is the most accurate method of determining energy requirements. In a clinical setting, however, measuring energy expenditure using an indirect calorimeter is impractical, time consuming, and expensive. As such, prediction equations using easily measurable variables are commonly used to predict REE [9].
In our case, the measured REE (1,707 kcal/day) was higher than the estimated REE (1,545 kcal/day) based on the Harris-Benedict equation. The measured REE increased to 2,416 kcal/day after 2 months. This observation is congruent with previous studies that measured REE using indirect calorimetry in pancreatic cancer patients. Several previous studies found elevated REE in patients with pancreatic cancer [7,10,11]. However, Dempsey et al. [12] found that patients with pancreatic cancer were predominantly hypometabolic, while Vaisman et al. found no differences in REE between patients and controls [13].
Contrary to the change in REE, energy intake decreased from 1,887 kcal/day (27.0 kcal/kg/day) to 1,060 kcal/day (15.4 kcal/kg/day) during the same period. Over time, the patient's weight rapidly decreased, and his nutritional status deteriorated. Previous studies have also reported insufficient intakes in pancreatic cancer patients [2,7,13]. Bye et al. found that several symptoms adversely influenced energy intake [2]. Our observation of nutritional status was consistent with previous results that reported nutritional depletion in pancreatic cancer patients [3].
Pancreatic cancer is ranked as the ninth most frequent type of cancer and the fifth most common cause of cancer-related deaths in Korea. The prognosis for patients with this disease is extremely poor, mainly due to the unresectable nature of the disease in 80-90% of patients at the time of diagnosis [14]. For these pancreatic patients, adequate nutritional support is necessary to maintain weight and nutritional status as well as to improve their QOL.
When estimating nutritional requirements, it may be important to remember that the values are just estimates and that there is always the possibility of nutritional depletion in this patient group. However, in a clinical setting, we can neither routinely assess REE by indirect calorimetry nor routinely obtain a 3-day food record, as this could be an added burden on the patients. Therefore, a dietitian should conduct a continuous follow-up to determine if estimated nutritional requirements are being met. Further researches on the relationships between dietary intake, metabolic rate, nutritional status, QOL, and other clinical outcomes in pancreatic cancer patients are necessary.
References
1. Stan SD, Singh SV, Brand RE. Chemoprevention strategies for pancreatic cancer. Nat Rev Gastroenterol Hepatol. 2010; 7:347–356.

2. Bye A, Jordhøy MS, Skjegstad G, Ledsaak O, Iversen PO, Hjermstad MJ. Symptoms in advanced pancreatic cancer are of importance for energy intake. Support Care Cancer. 2013; 21:219–227.

3. Wigmore SJ, Plester CE, Richardson RA, Fearon KC. Changes in nutritional status associated with unresectable pancreatic cancer. Br J Cancer. 1997; 75:106–109.

4. Okusaka T, Okada S, Ishii H, Ikeda M, Kosakamoto H, Yoshimori M. Prognosis of advanced pancreatic cancer patients with reference to calorie intake. Nutr Cancer. 1998; 32:55–58.

5. Ferrucci LM, Bell D, Thornton J, Black G, McCorkle R, Heimburger DC, Saif MW. Nutritional status of patients with locally advanced pancreatic cancer: a pilot study. Support Care Cancer. 2011; 19:1729–1734.

6. Davidson W, Ash S, Capra S, Bauer J. Cancer Cachexia Study Group. Weight stabilisation is associated with improved survival duration and quality of life in unresectable pancreatic cancer. Clin Nutr. 2004; 23:239–247.

7. Bosaeus I, Daneryd P, Svanberg E, Lundholm K. Dietary intake and resting energy expenditure in relation to weight loss in unselected cancer patients. Int J Cancer. 2001; 93:380–383.

8. Elliott L, Molseed LL, McCallum PD. The clinical guide to oncology nutrition. 2nd ed. Chicago (IL): American Dietetic Association;2006.
9. Bauer J, Reeves MM, Capra S. The agreement between measured and predicted resting energy expenditure in patients with pancreatic cancer: a pilot study. JOP. 2004; 5:32–40.
10. Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC. Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg. 1994; 219:325–331.

11. Barber MD, McMillan DC, Preston T, Ross JA, Fearon KC. Metabolic response to feeding in weight-losing pancreatic cancer patients and its modulation by a fish-oil-enriched nutritional supplement. Clin Sci (Lond). 2000; 98:389–399.

12. Dempsey DT, Feurer ID, Knox LS, Crosby LO, Buzby GP, Mullen JL. Energy expenditure in malnourished gastrointestinal cancer patients. Cancer. 1984; 53:1265–1273.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download