Abstract
Short Bowel Syndrome (SBS) is a condition that causes malabsorption and nutrient deficiency because a large section of the small intestine is missing or has been surgically removed. SBS may develop congenitally or from gastroenterectomy, which often change the motility, digestive, and/or absorptive functions of the small bowel. The surgical procedure for SBS and the condition itself have high mortality rates and often lead to a range of complications associated with long-term parenteral nutrition (PN). Therefore, careful management and appropriate nutrition intervention are needed to prevent complications and to help maintain the physiologic integrity of the remaining intestinal functions. Initial postoperative care should provide adequate hydration, electrolyte support and total parenteral nutrition (TPN) to prevent fatal dehydration. Simultaneously, enteral nutrition should be gradually introduced, with the final goal of using only enteral nutrition support and/or oral intake and eliminating TPN from the diet. A patient should be considered for discharge when macro and micronutrients can be adequately supplied through enteral nutrition support or oral diet. Currently, there is more research on pediatric patients with SBS than on adult patient population. A 35-year-old man with no notable medical history was hospitalized and underwent a surgery for acute appendicitis at a local hospital. He was re-operated on the 8th day after the initial surgery due to complications and was under observation when he suddenly complained of severe abdominal pain and high fever. He was immediately transferred to a tertiary hospital where the medical team discovered free air in the abdomen. He was subsequently diagnosed with panperitonitis and underwent an emergency reoperation to explore the abdomen. Although the patient was expected to be at a high risk of malnutrition due to short bowel syndrome resulting from multiple surgeries, through intensive care under close cooperation between the medical and nutrition support team, his nutritional status improved significantly through continuous central and peripheral parenteral nutrition, enteral nutrition, and oral intake. The purpose of this paper is to report the process of the patient's recovery.
Short bowel syndrome (SBS) is a serious, disabling, socially incapacitating and potentially life-threatening condition [1]. Patients with SBS typically experience severe diarrhea, steatorrhea, electrolyte disturbances, dehydration, malnutrition, and weight loss [2]. Many patients with intestinal failure, particularly SBS, require long-term parenteral nutrition (PN) and/or intravenous (IV) fluids [3]. Although patients require parenteral nutrition (PN) and/or intravenous (IV) fluids in the immediate post-resection period, oral diet and enteral nutrition (EN) should be introduced as soon as possible to enhance intestinal adaptation [4]. Optimizing hydration and enteral nutrition (EN) through individualized dietary and pharmaceutical management of SBS can reduce or eliminate the need for PN/IV and improve the nutritional status of this patient population [4].
This article presents a patient with short bowel syndrome and panperitonitis who needed nutritional support during the hospitalization but was discharged with the ability to receive adequate nutrition through oral intake.
A 35-year-old man was admitted to the surgical ward through the Emergency Room (ER) at Gangnam Severance Hospital on May 20, 2011. He had no notable medical history except a laparoscopic appendectomy for acute appendicitis on May 4, 2011 at a local hospital. He was readmitted to the same hospital 8 days later on May 12 for complication-related reoperation and was under the observation when he developed acute abdominal pain, fever, surgical wound infection and both pulmonary effusions. The patient was immediately transferred to the Gangnam Severance Hospital and was diagnosed with panperitonitis. The X-ray result showed free air in the abdomen, which required him to undergo emergency reoperation. During the operation, perforation was found 50 cm above the terminal ileum and the patient had to undergo small bowel resection and anastomosis. He underwent an emergency exploratory laparotomy, irrigation and drainage, jejunostomy, and percutaneous endoscopic jejunostomy. An endto- end anastomosis at the resection site was difficult; thus, the surgeons performed jejunostomy at the proximal jejunum and inserted a feeding tube at the distal jejunum to attach the distal jejunum to the right anterior peritoneum (Figure 1).
At the initial nutrition assessment upon admission, the patient was categorized as 'patient at high-risk of malnutrition' with serum albumin of 1.8 g/dL, lymphocytes of 0.73 × 103/µL and body mass index of 17.6. And also, before admittance to the Gangnam Severance Hospital, he had already experienced severe weight loss from 55 kg to 50.9 kg (7.5% weight loss) after the appendectomy. To correct his serum albumin level, the medical team injected seven packs of 20% albumin infusion and was able to recover the patient's serum albumin level to 3.6 g/dL; the patient had been receiving 50% of the minimum nutrition requirement through total parenteral nutrition (TPN) during early intensive care unit (ICU) days. The patient was referred to the nutrition support team on hospital stay day 5 and taking everything into consideration, he was classified as 'moderate malnutrition'.
The nutrition support team recommended the use of TPN given that enteral feeding was not a feasible option due to the surgery. Therefore, the patient received parenteral nutrition (2,180 kcal, 260 g of carbohydrate, 58 g of protein, 100 g of fat and 20 g of glutamine per day) through the right jugular line for 15 days after the surgery (Figure 1).
The patient started oral feeding on hospital stay day 8 but nutrients were not properly absorbed because most of them were lost through the proximal jejunostomy.
Enteral nutrition started on hospital stay day 22 through the jejunal feeding tube. Standard enteral nutrition formula (MediWell RTH has 1,000 kcal per 1,000 ml containing 140 g of glucose, 46 g of protein, and 30 g of fat) was provided. The amount of formula administered gradually increased from 300 kcal/300 ml to a maximum of 1,700 kcal/1,700 ml but the infusion rate and volume had to be frequently adjusted to address abdominal discomfort and frequent diarrhea but such changes did not fully improve the patient's condition (Figure 1).
Meanwhile, on hospital stay day 20, the medical and nutrition support team decided to re-administer the bolus that was lost through the proximal jejunostomy back into the jejunal feeding tube, which was expected to extend the contact time between the nutrients and shortened small intestine, thereby increasing absorption. This procedure was employed until the final surgery.
As the amount of standard enteral nutrition provided increased, there was an increase in diarrheal episodes. Following the recommendation of the nutrition support team, the patient started receiving hydrolyzed nutrition formula (MonoWell: 400 kcal per packet containing 50 g of glucose, 16 g of protein and 15 g of fat) on hospital stay day 55 that contains amino acids, which are more easily absorbed than intact proteins.
Taking hypertonicity of the standard enteral nutrition formula into consideration, the hydrolyzed nutrition formula was given in lower concentration (0.5 kcal/ml) and was administered over 15 hours. This adjustment made a significant improvement in reducing diarrheal episodes. The volume was then gradually increased over a month and reached a daily average of 1,000 kcal and 40 g of protein. To complement the inadequacy of the enteral nutrition, a 1,000 kcal peripheral intravenous nutrition, containing 50 g of protein, vitamins and minerals, was provided until the final surgery.
On hospital stay day 66, the medical team desired to readminister standard enteral nutrition formula to stimulate normal digestive function of the small bowel but the patient continued to show maladjustment signs like diarrhea. Thus, the team provided continuous but a small volume of the standard enteral nutrition until the final surgery.
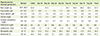
Despite the administration of TPN after the initial surgery, the patient experienced rapid weight loss of about 3 kg over 3 weeks since the admission to the hospital. By the 21st day of hospitalization at Gangnam Severance Hospital, the patient weighed approximately 47 kg. However, through enteral and parenteral nutrition support, his weight stabilized and his blood lab values also returned to normal figures (Table 1).
At the final surgery on hospital stay day 85, the medical team removed the jejunal feeding tube, repaired the jejunostomy, eliminated a section of the edematous distal jejunum by 50 cm, and performed anastomosis of the distal jejunum and the healthy proximal jejunum. The patient switched from parenteral nutrition to liquid diet on hospital stay day 89 and was discharged on hospital stay day 97 when he was completely able to eat a regular meal instead of a liquid diet.
Most patients with short bowel syndrome are often malnourished because they have significantly lower macro and micronutrient intake and absorption than healthy individuals. Thus, it is essential that appropriate nutritional support is provided at each phase of the treatment. Nutritional support for SBS patients should aim to control diarrhea, abdominal discomfort, weight loss, and dehydration.
The process of nutrition intervention employed for this particular SBS patient is a great example to illustrate the importance of careful nutrition management: prescribing an appropriate enteral nutrition product and being attentive to the amount and method of administration of the formula. Central intravenous nutrition was administered during the initial stage in order to reduce diarrheal episodes and to improve the nutrition status of the patient. Taking low serum cholesterol level into consideration, administration of lipid emulsion was actually higher than the recommended amount. Optimal enteral nutrition support with scrupulous nutritional management has prevented further weight loss and led to the improvement of the intake volume, nutrition status and blood lab results, and advancement in the form of the diet consumed. Particularly, the medical team's request for nutrition support team consultation to better manage the nutrition status of the patient on hospital stay day 5 was appropriate given the nature of the disease. Consequently, the medical team officially requested a total of 15 consultations during the patient's hospitalization and the patient was monitored at least 3 to 4 times a week, which ensured proper and prompt response to the patient's status.
Several practices that could have been done differently during the nutritional support provision. First, the elemental formula could have been given earlier; the use of hydrolyzed enteral nutrition was delayed to some extent because of the high cost of the product. Second, a more accurate evaluation of the patient's gastrointestinal function could have been made prior to switching back from elemental to standard enteral nutrition formula to prevent maladaptation complications such as diarrhea.
In general, the daily dietary caloric consumption should increase by at least 50% of the typical intake to compensate for the malabsorption of both macro and micronutrients associated with SBS. Patients who received enteral tube feeding or consumed oral diet in conjunction with tube feeding had a significantly higher caloric, lipid, and protein intake compared with patients who received oral diet alone. Positive outcomes observed with tube feeding in this study may have arisen from the continuous mode of administration and the resulting persistent luminal stimulation [5].
For patients with SBS who require tube feeding, studies suggest that elemental and polymeric diets are similar in terms of nutrient absorption and fluid and electrolyte loss [6,7]. Generally, polymeric formulas are less costly and less hyperosmotic than elemental formulas and are generally well tolerated. Additionally, polymeric diets may better enhance intestinal adaptation compared to elemental diets [8]. Given these advantages, polymeric formulas are more commonly administered to patients with SBS [9]. However, when it is not tolerated because patient has severe malabsortion, an elemental diet should be used.
In this particular case, elemental diet produced better results and more effectively reduced incidence of diarrhea than the polymeric diet. Maybe the left bowel was too short to absorb intact nutrients from the polymeric formula. A relationship between dietary intact protein and longer duration of diarrhea has been reported in rats after 80% small intestinal resection during a 4-week study [10]. Compared with intact protein, an elemental diet obviously requires less processing of protein digestion before absorption. And also report of Hua et al. showed that SBS piglets without ileum had less ability to tolerate polymeric formula [11]. Interestingly, the patient was given a polymeric formula with fiber first. Diet that includes soluble fiber (e.g. pectin) has been shown to be helpful for patients with SBS; soluble fiber can solidify stool, increase colonic transit time, and act as a substrate for colonic fermentation into short chain fatty acids [12-14]. But in this case the effect of soluble fiber didn't work properly.
Considering this case, close monitoring and modification of diets are critical when providing enteral nutrition support. And also, throughout the adaptive and post-adaptive phases of recovery, patients should be periodically reevaluated to determine whether further reduction in parenteral nutrition is possible [4].
The basic guidelines of nutritional support in short SBS are not different between pediatric and adult patients. Nutrition management of the infant or young child with significant injury to the GI tract that requires resection and long term use of PN is complex. Each patient is unique, and management should be individualized based on the initial injury, amount and site of resection, and duration of PN. Early focus on engaging and educating the primary caregivers is a key predictor for success. Early, aggressive introduction and advancement of enteral feeds are critical for promoting intestinal adaptation, preventing intestinal failure-associated liver disease, and weaning the patient off PN [15]
Currently, reports on intensive nutritional support and management for adult SBS patients are meager. As such, it is not easy to encounter SBS patients in general hospitals. The SBS patient presented in this case experienced severe diarrhea, electrolyte imbalance and micronutrient deficiencies from multiple small bowel resections. However, after receiving optimal nutrition using elemental and standard enteral formula in addition to the parenteral nutrition support during his recovery, the patient successfully adapted to an oral diet. This case not only epitomizes the importance of appropriate nutrition care but also presents how close cooperation between the medical and the nutrition support team can notably contribute to the recovery of the patient.
Figures and Tables
References
1. Nightingale J, Woodward JM. Small Bowel and Nutrition Committee of the British Society of Gastroenterology. Guidelines for management of patients with a short bowel. Gut. 2006; 55:Suppl 4. iv1–i12.

2. Thompson JS, Weseman R, Rochling FA, Mercer DF. Current management of the short bowel syndrome. Surg Clin North Am. 2011; 91:493–510.

3. Compher C, Winkler M, Boullata JI. Nutritional management of short bowel syndrome. In : Marian M, Russell MK, Shikora SA, editors. Clinical nutrition for surgical patients. Sudbury (MA): Jones and Bartlett Publishers;2008. p. 283–306.
4. Matarese LE. Nutrition and fluid optimization for patients with short bowel syndrome. JPEN J Parenter Enteral Nutr. 2013; 37:161–170.

5. DiBaise JK, Young RJ, Vanderhoof JA. Intestinal rehabilitation and the short bowel syndrome: part 2. Am J Gastroenterol. 2004; 99:1823–1832.

6. Levy E, Frileux P, Sandrucci S, Ollivier JM, Masini JP, Cosnes J, Hannoun L, Parc R. Continuous enteral nutrition during the early adaptive stage of the short bowel syndrome. Br J Surg. 1988; 75:549–553.

7. McIntyre PB, Fitchew M, Lennard-Jones JE. Patients with a high jejunostomy do not need a special diet. Gastroenterology. 1986; 91:25–33.

8. Healey KL, Bines JE, Thomas SL, Wilson G, Taylor RG, Sourial M, Pereira-Fantini PM. Morphological and functional changes in the colon after massive small bowel resection. J Pediatr Surg. 2010; 45:1581–1590.

9. Sundaram A, Koutkia P, Apovian CM. Nutritional management of short bowel syndrome in adults. J Clin Gastroenterol. 2002; 34:207–220.

10. Iglesias AC, Portari PE, Zucoloto S, Vannucchi H. Experimental short-bowel syndrome: free amino acid versus intact protein in nutritional support. Nutr Res. 1994; 14:1831–1839.

11. Hua Z, Turner JM, Mager DR, Sigalet DL, Wizzard PR, Nation PN, Ball RO, Pencharz PB, Wales PW. Effects of polymeric formula vs elemental formula in neonatal piglets with short bowel syndrome. JPEN J Parenter Enteral Nut. 2013; Forthcoming.

12. Meier R, Beglinger C, Schneider H, Rowedder A, Gyr K. Effect of a liquid diet with and without soluble fiber supplementation on intestinal transit and cholecystokinin release in volunteers. JPEN J Parenter Enteral Nutr. 1993; 17:231–235.

13. Cummings JH, Southgate DA, Branch WJ, Wiggins HS, Houston H, Jenkins DJ, Jivraj T, Hill MJ. The digestion of pectin in the human gut and its effect on calcium absorption and large bowel function. Br J Nutr. 1979; 41:477–485.

14. Atia A, Girard-Pipau F, Hébuterne X, Spies WG, Guardiola A, Ahn CW, Fryer J, Xue F, Rammohan M, Sumague M, Englyst K, Buchman AL. Macronutrient absorption characteristics in humans with short bowel syndrome and jejunocolonic anastomosis: starch is the most important carbohydrate substrate, although pectin supplementation may modestly enhance short chain fatty acid production and fluid absorption. JPEN J Parenter Enteral Nutr. 2011; 35:229–240.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download