Abstract
The Nutrition Care Process (NCP), developed by the American Dietetic Association, is a significant issue to dietetic professionals in many countries and there are rising needs for NCP implementation in Korea. We surveyed clinical nutrition managers of Korean general hospitals regarding the perception of NCP, the status of NCP implementation, and the opinions on NCP. The questionnaire was collected from 35 hospitals. Most clinical nutrition managers perceived NCP, but NCP implementation in hospital was at early stage. NCP was implemented in a fourth of the surveyed hospitals and many clinical nutrition managers responded that the lack of knowledge and the concern on increasing working time were major barriers to implementing NCP. To successfully implement NCP in Korean hospital, ongoing education and training programs should be developed to provide adequate knowledge and help dietitians to cope with the barriers.
The Nutrition Care Process (NCP), developed by the American Dietetic Association (now the Academy of Nutrition and Dietetics), was designed to improve the consistency and quality of individualized care for patients/clients or groups and the predictability of the patients/client outcome [1]. It consists of four distinct, interrelated steps - nutrition assessment, nutrition diagnosis, nutrition intervention, and nutrition monitoring and evaluation. The NCP provides dietetic professionals with a framework for critical thinking and decision-making. It is thought that use of the NCP can lead to more efficient and effective care and greater recognition of the role of dietetic professionals in all care settings [1,2]. Also the Academy of Nutrition and Dietetics developed International Dietetics and Nutritional Terminology (IDNT) to describe the unique functions of dietetic professionals in each step of NCP [2,3]. Now the dietetic professionals have shown significant interest in NCP and are trying to implement NCP in many countries [4-6]. Also in Korea, the attention to NCP has been increasing among the dietetic professionals.
Several Korean hospitals attempted to apply NCP into their clinical practices and made many efforts to improve NCP implementation consistently for years. The Korean Dietetic Association (KDA) recognized the needs to gather information on NCP and the necessity of NCP implementation in Korea. Accordingly KDA undertook a few projects, and the 'International Dietetics and Nutritional Terminology (IDNT), second edition' was translated into Korean in March 2012. The Korean Society of Hospital Dietitians (KSHD, the organization under KDA) held the workshops and education programs on NCP for hospital dietitians, and in 2012, organized a taskforce team to develop NCP education programs for dietetic professionals. Not only KSHD but some local branches of KDA also constructed education programs. Besides KDA, several academic societies have made an effort to enhance the abilities to apply and to teach NCP. Moreover NCP is included in the standard education curriculum for Clinical Dietitian training. As Clinical Dietitian is now certified by the Ministry of Health and Welfare (legislated in 2010), it is recommended that Clinical Dietitian candidates fully experience NCP at Clinical Dietitian training institutes. These various situations provoke the dietetic professionals' attention to NCP in Korea.
In this circumstance, we conducted the survey to investigate the status of NCP implementation in Korean hospitals. Also we surveyed the perception and the opinions on NCP of clinical nutrition managers of general hospitals in Korea.
This survey was carried out among clinical nutrition managers of general hospitals in Korea. The questionnaires were delivered to 82 general hospitals located nationwide via e-mail in May 2012. These 82 hospitals had experiences of attending the second Hospital Evaluation Program conducted by the Ministry of Health and Welfare (2007-2009) and the clinical nutrition managers of those hospitals are recognized to possess relatively higher awareness of the professional performance of clinical dietitians at their own fields in Korea. Of the 82 questionnaires delivered, 37 responses were collected, for a response rate of 45.1%. We analyzed data from 35 responses and 2 incomplete responses were excluded.
The questionnaire was composed of three parts. The questions included in the first part were on the information on structural characteristics of hospitals related to clinical nutrition care performance. The second part was composed of questions on the perceptions and knowledge on NCP. The questions related to the NCP practice were included in the final part. A pretest was conducted and the initial questionnaire was corrected and revised according to results of the pretest.
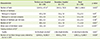
General characteristics of surveyed hospital are presented in Table 1. Sixty-eight percent of hospitals were tertiary care hospitals (designated by Ministry of Health and Welfare among general hospitals, and should be satisfied the assigned levels of disease severity of treated, staffs, facilities, and equipment etc) and 45.7% of hospitals (16 hospitals) were located in Seoul. The percentage of Clinical Dietitian training institutes was significantly higher in tertiary care hospital.
The responses to questions regarding perception and knowledge on NCP and IDNT are shown in Table 2. More than 90% of respondents answered that they had known NCP or IDNT, and major routes to know them were academic programs and the education programs of the KDA. Most respondents had taken education on NCP and more than 75% of respondents had taken education on IDNT. Seminars or workshops held by the KSHD played important roles in providing hospital dietitians with the opportunities to know NCP and IDNT. Respondents answered that the known levels of dietitians working in their hospitals were not relatively high, especially IDNT. Although there were shown no significant differences, the percentages of respondents perceived NCP and IDNT were higher in those who worked in the hospitals implementing NCP (Table 3). However there were significant differences in dietitians' knowledge levels on NCP and IDNT between the hospitals implementing NCP and the hospitals not implementing NCP. The percentages of dietitians responded "very well" and "well" were higher in the hospitals implementing NCP.
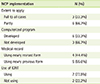
NCP was implemented in 9 hospitals among surveyed hospitals and Table 4 shows the status of NCP implementation in these hospitals. Six of those hospitals were Clinical Dietitian training institutes. Mean duration of NCP implementation was 21.9 months, but the duration varied greatly depending on the hospital (2 to 52 months). In a-third of those hospitals, NCP was applied to all nutrition therapy cases. Computerized programs were using in NCP implementation in two-thirds of hospitals implementing NCP. IDNT had been used in NCP records in 7 hospitals and the steps of NCP using IDNT were different depending on the hospital (Figure 1). The clinical nutrition managers of 21 hospitals among 26 hospitals not implementing NCP responded that they planned to introduce NCP in the near future.
The opinions of clinical nutrition managers on NCP are shown in Table 5. The percentages of NCP steps responded as the most difficult to implement were similar among 3 steps except nutrition assessment step. The major benefits of NCP implementation thought by the clinical nutrition managers from NCP implementing hospitals were the easy decision-making and the quality improvement of nutrition care. Lack of knowledge and increased time spent were pointed out as the major difficulties in settlement of NCP implementation. These were also the major reasons that made the clinical nutrition managers hesitate to introduce NCP to their hospitals.
The results of this survey showed that NCP implementation in Korea is in an early stage. Most clinical nutrition managers perceived NCP and IDNT and had the education experiences on NCP and IDNT. However many hospitals did not implement NCP. Even among Clinical Dietitian training institutes, NCP was implemented in less than a third of the hospitals. This low NCP implementation rate is going to be a problem not only in the improvement of nutrition care, but in the training of Clinical Dietitian candidates. Many clinical nutrition managers were concerned about the lack of knowledge and skills of their dietitians and the increase of time spent with adopting NCP. It was consistent with the responses on difficulties in implementing NCP from the clinical nutrition managers in hospitals that had adopted NCP. However many clinical nutrition mangers responded 'easy decision-making' and 'efficient communication' as the benefits of NCP implementation. This suggests that there is no need to delay NCP implementation because of the concern in the extra time spent. In the initial stage, it may become an issue because dietitians have to change their way of work, but the working time may decrease after the adapting to the new method. In fact, the periods of NCP implementation were less than a year in about a half of hospitals that had adopted NCP. The barriers to adopt NCP and difficulties in implementing NCP pointed out from our survey results were similar to the responses reported in the U.S. [7].
IDNT was used in many hospitals implemented NCP, but the extent of IDNT use varied depending on the hospital. IDNT was used at nutrition diagnosis step in all hospitals using IDNT, but used at other steps of NCP in less than a half of those hospitals. Nutrition diagnosis is the new step that distinguishes NCP from the existing process and requires using IDNT. As a result, nutrition diagnosis terminology will be familiar and widely used in practice compared to other terminologies (nutrition assessment terminology, nutrition intervention terminology, and nutrition monitoring & evaluation terminology). It was found that nutrition diagnosis terminology was the most familiar and was most widely used in the U.S. [8].
Our survey was carried out on a small scale and administered to limited subjects, clinical nutrition managers. Therefore it is possible that there were differences between our results and the thought of overall working dietitians in clinical fields. The role of clinical manager is important to adopt NCP, however dietitians who practice nutrition therapy in the fields play an important role also. The extensive comprehensive survey will be needed and it will provide us with valuable information needed to implement NCP and to improve NCP implementation.
Implementation of NCP is required to enhance efficiency, effectiveness, and quality of nutrition therapy. To successfully implement NCP in Korean hospital, ongoing education and training programs should be developed to provide adequate knowledge and help dietitians to cope with the barriers to NCP implementation.
Figures and Tables
Figure 1
The steps of NCP using IDNT in 7 hospitals using IDNT. NCP: nutrition care process, IDNT: international dietetics and nutritional terminology.
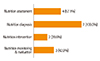
Table 3
Comparison of the perception and knowledge on NCP and IDNT according to NCP implementation in the hospital*

References
1. Lacey K, Pritchett E. Nutrition Care Process and Model: ADA adopts road map to quality care and outcomes management. J Am Diet Assoc. 2003; 103:1061–1072.

2. American Dietetic Association. International Dietetics & Nutrition Terminology (IDNT) reference manual: standardized language for the nutrition care process. 3rd ed. Chicago (IL): American Dietetic Association;2010.
3. Writing Group of the Nutrition Care Process/Standardized Language Committee. Nutrition care process part II: using the International Dietetics and Nutrition Terminology to document the nutrition care process. J Am Diet Assoc. 2008; 108:1287–1293.
4. Baker SD, Cotugna N. Students entering internship show readiness in the nutrition care process. J Hum Nutr Diet. 2013; Forthcoming.

5. Van Heukelom H, Fraser V, Koh JC, McQueen K, Vogt K, Johnson F. Implementing nutrition diagnosis at a multisite health care organization. Can J Diet Pract Res. 2011; 72:178–180.

6. Atkins M, Basualdo-Hammond C, Hotson B. Dietitians of Canada. Canadian perspectives on the nutrition care process and international dietetics and nutrition terminology. Can J Diet Pract Res. 2010; 71:e18–e20.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download