Abstract
The purposes of the study were to assess knowledge, self-efficacy, and perceived barriers on a low-iodine diet among thyroid cancer patients and to identify strategies for nutrition education. A self-administered questionnaire was developed based on a review of literature and pilot-tested. A total of 121 female thyroid cancer patients participated in a survey and 117 responses were used for data analysis. An average knowledge score of the thyroid cancer patients was 4.5 point (available score: 0-10 point). Majority of the respondents knew that seaweeds such as lavers, brown seaweeds, and sea tangles contain large amount of iodine. However they mistook the low iodine diet as a low salt diet and were not aware of foods and seasonings that are allowed on the low iodine diet. While self-efficacy related to consuming various fruits and vegetables, to choosing potatoes and sweet potatoes for snacks, and restricting consumption of eggs, milk and milk products, and processed foods was rated highly, self-efficacy for preparing foods without using sea salts was rated low. The self-efficacy score increased as their interest on the dietary life and perceived cooking skills were greater. Most perceived barriers toward practicing the low iodine diet were related to preparation of the low iodine menus. As their interest in the dietary life and cooking and perceived cooking skills were greater, the patients perceived barriers on practicing the low iodine diet less. While the patients showed higher self-efficacy and lower barrier perception on selecting foods low in iodine and restricting food high in iodine, they showed lower self-efficacy and higher barrier perceptions on preparing low iodine meals. Clinical dietitians should recognize the gap between what the patients should know and what they really know and identify strategies on how to improve self-efficacy and reduce perceived barriers on the low iodine diet. Recent literature and the findings of the study reveal that incorporating cooking classes into nutrition education for thyroid patients is effective to enhance self-efficacy and to reduce perceived barriers on the low iodine diet.
The incidence of thyroid cancer has been increasing rapidly in both Korea and abroad. The Ministry of Health and Welfare and Korea Central Cancer Registry of the National Cancer Center [1] reported that 192,561 people were newly diagnosed with cancer in 2009. In particular, thyroid cancer patients accounted for the highest ratio with 16.6% (31,977 people). Thyroid cancer accounts for 28.7% of cancer diagnosed in women.
Radioactive iodine (I131) therapy which follow thyroidectomy has been reported to destroy residual tissues and to decrease the recurrence of thyroid cancer [2-4]. Radioactive isotopes are orally ingested and accumulated at a high concentration in the thyroid tissue. The β-rays emitted from the radioactive isotopes treat thyroid diseases without affecting surrounding tissues. The effectiveness of the radioactive iodine (RAI) therapy is influenced by the radiation dose that reaches the residual thyroid tissue or tumor [5,6]. As the iodine accumulated in the body reduces the treatment effect, the iodine remaining in the body must be minimized before administrating RAI therapy. Before the RAI treatment, therefore, a temporary low-iodine diet (LID) is recommended to optimize RAI uptake of the thyroid tissues. The theoretical basis of this treatment is that low plasma iodine concentrations increase the expression of sodium iodide symporter (hNIS) to eventually increase the specific activities of RAI [7,8].
Many physicians in Korea recommend 1-4 week LID for thyroid cancer patients to deplete iodine in the body before implementing RAI therapy. Previous studies have reported that iodine-restricted diet not only increases radioactive iodine uptake by 17-233%, but it also raises the effective half-life of radioactive iodine. These two factors in turn increase the radiation dose up to 51-146% [9-11]. Morris et al. [12] reported that urine iodine excretion was significantly lower after institution of LID and Goslings & Hannon [9] also reported that the urinary iodine excretion decreased from 121.6 ± 36.9 µg/day to 30.0 ± 9.7 µg/day after LID for 4 days. By measuring 24 hour urinary iodine excretion in Dutch thyroid cancer patients, Pluijmen et al. [13] reported that LID was effective in RAI therapy.
Previous studies on LID for thyroid cancer patients conducted in Korea have mainly focused on comparing the effectiveness of LID by stringency and duration of the iodine restriction [14-16]. Yoo et al. [16] compared the success rate of postsurgical RAI ablation in differentiated thyroid cancer patients between less strict LID, which restricted seafood, iodized salt, egg yolk, dairy products, processed meat, instant food, and multi-vitamin supplements and very strict LID, which also restricted rice, freshwater fish, spinach, and soybean products in addition to the food types above. Results of the study showed that the very strict LID did not present significant differences in the success rate of therapy preparation, but rather made patients feel a high level of discomfort.
Despite the high incidence rate of thyroid cancer and the importance of LID among thyroid patients before receiving RAI therapy, studies on the nutritional education for thyroid cancer patients preparing for LID remain insufficient in Korea. Considering that the goal of nutrition education is to help subjects to acquire nutrition knowledge and related skills and practice recommended dietary behaviors through group education or individual counseling [17], it is important for clinical dietitians to assess the preparedness of the thyroid cancer patients of LID before developing a nutritional education program on LID. Nutrition education experts have argued that the theories of education and behavioral changes must be applied to enhance the effectiveness of nutrition education since acquisition of nutrition knowledge is an essential factor for behavioral changes but is not enough for behavioral changes. In particular, the Health Belief Model or Social Cognitive Theory commonly applied in nutrition education places emphasis on self-efficacy, which can be defined as the 'confidence in successfully performing behaviors necessary for producing favorable results' [18]. Studies have reported that people with higher self-efficacy are more likely to perform certain behaviors or overcome barriers. The perceived barriers refer to the 'personal awareness of the physical and psychological costs that must be paid to perform recommended behaviors.' These perceived barriers can be reduced through re-confirmation of perceived barriers, correction of wrong information, compensation, and support.
The objectives of this study were to investigate the patients' knowledge of LID and self-efficacy and perceived barriers for practicing LID and to identify an educational strategy for enhancing the practice of LID among thyriod cancer patients preparing for RAI therapy.
Subjects were recruited from a general hospital located in Seoul. The subjects were selected from the female patients aged between 18-90 that were preparing for RAI therapy. Patients that had received RAI therapy in the past were excluded. This study was reviewed by the Institutional Review Board (IRB) of Gangnam Severance Hospital and the research participants signed the informed consent form after receiving an explanation on the purpose of study. A total of 121 patients consented to research participation and answered the questionnaire from July 2011 to February 2012. Four incomplete questionnaires were excluded and 117 questionnaires were used in analysis.
The survey was conducted using a self-administered questionnaire. Since literature review did not reveal studies on the nutrition education related to LID for the thyroid cancer patients, the research team developed a questionnaire based on research on nutrition education and dietary habits of adolescents, adults and diabetes patients and literature related with LID for thyroid cancer patients [16,19-24]. The questionnaire was modified after a pilot test with 15 women. The final questionnaire was composed of dietary life and cooking practices, knowledge of LID, perception of self-efficacy and barriers for practicing LID, and demographic information.
The dietary life and cooking practice section was composed of eight items including interest in dietary life, interest in cooking, and frequency of cooking and dining out. The knowledge of LID was evaluated through 10 items including the types of food allowed and not allowed for LID and cooking methods of low-iodine food (scale: true, false, not sure). The self-efficacy for practicing LID was assessed with 12 items and was evaluated through a Likert type seven-point scale (1: not confident at all, 7: very confident). The perceptions of 11 personal and environmental barriers in relation to LID were evaluated through a Likert type seven-point scale (1: strongly disagree, 7: strongly agree). Lastly, the demographic information of participants, such as their age, level of education, and number of family members, were investigated.
Data were analyzed through SPSS software program (PASW 18.0). Descriptive statistics analysis and correlation analysis were conducted. Means among groups were compared through one-way analysis of variance (ANOVA) and the Least Significant Difference (LSD) post-hoc tests was performed when significant differences were found from ANOVA. All tests were implemented at a significance level of 0.05.
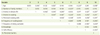
The research participants were all female thyroid patients waiting for RAI therapy (Table 1). The patients were aged between 24-66 (average age: 41.5) and more than half of the respondents were in their 30s. Nearly 60% of the participants were college graduates and a majority lived in Seoul and Gyeonggi area. Approximately 20% of the participants answered that they did not prefer meat, fruits or fish, whereas 25% answered that they were not particularly fussy about food (Table 2). Ten to fifteen percent of the respondents did not enjoy dairy products and eggs which were restricted in LID, whereas a majority enjoyed seaweeds. The respondents generally showed a high level of interest in dietary life. Half of the respondents answered that they were interested in cooking but evaluated their own cooking skills to be average.
Participants' LID knowledge scores ranged from 0 to 9 (available score: 0-10 point) and the average was 4.51 (standard deviation: 2.14) (Table 3). The item that presented the highest percentage of correct answers was 'Seaweeds such as laver, brown seaweeds, and sea tangles are high in iodine.' However, the percentage of correct answers was low in other items. Nearly half of the respondents misunderstood that LID should be continued even after RAI therapy, when in truth it must be practiced for a short period (generally 2-4 weeks) before treatment. Also, the respondents did not know that they were allowed to eat kimchi prepared by refined salt. The respondents also possessed little knowledge on the foods restricted in LID, such as soybean paste, soy sauce, multi-vitamins, processed meats, milk, and dairy products. The item 'LID is a low-salt diet (false)' presented the lowest percentage of correct answers (12%).
The self-efficacy of thyroid cancer patients for practicing LID was measured through 12 items. The Cronbach's alpha of the 12 items was presented as 0.86 and the items showed high level of internal consistency. The self-efficacy scores were dispersed across a range of 3.9-5.9 (Table 4). The following items showed high self-efficacy: 'I am confident in consuming various fruits while I practice LID for 2 weeks (5.9)', 'I am confident in consuming various vegetables excluding seaweeds (5.7)', and 'I am confident in eating potatoes and sweet potatoes rather than commercial bakery products for snacks (5.6).' These items were related with the intake of foods allowed in LID. The following items presented low self-efficacy: 'I am confident in preparing tasty food without using sea salt (3.9)', 'I am confident in using low-iodine sauces and condiments instead of soybean paste and soy sauce that contain sea salt (4.1)', and 'I am confident in choosing low-iodine food and products when shopping (4.2).' In this regard, the respondents showed low self-efficacy in restricting foods that were not allowed on LID.
The perception of the potential barriers related to practicing LID was measured through 11 items. Cronbach's alpha was 0.73, which indicated acceptable internal consistency. The scores of perceived barriers measured through the seven-point scale was dispersed across a range of 1.9-5.5 (Table 5).
The most significant barrier perceived by the patients was 'I am not knowledgeable about how to prepare low-iodine menus (5.5)', and 'There is no one to prepare low-iodine meals for me (4.9).' In addition, 'I cannot distinguish foods high in iodine from those low in iodine (4.8)', 'I enjoy foods with high iodine content (4.5)', 'It is inconvenient to separately prepare different food from other family members (4.3)', and 'I lack cooking skills (4.1)' were also perceived as barriers with average or higher scores.
To establish a strategy for developing a nutrition education program for thyroid cancer patients preparing for LID, this study analyzed the correlation among the patients' knowledge of LID, self-efficacy and barriers of practicing LID, the demographic variables, and dietary life-related variables of thyroid cancer patients (Table 6). While the thyroid cancer patients' knowledge of LID significantly decreased with higher age (p < 0.05), the knowledge score did not show significant correlation with the patients' interest in dietary life, perceived cooking skills, interest in cooking, self-efficacy for practicing LID, and perceived barriers. The self-efficacy for practicing LID presented a significantly positive correlation with interest in dietary life (p < 0.01), interest in cooking (p < 0.01), and perceived cooking skills (p < 0.01). On the other hand, it presented a negative correlation with frequency of dining out (p < 0.05) and perceived barriers for practicing LID (p < 0.001).
The perceived barriers for practicing LID presented a negative correlation with age (p < 0.05), interest in dietary life (p < 0.01), interest in cooking (p < 0.01), perceived cooking skills (p < 0.01), and cooking frequency (p < 0.01) and a positive correlation with dining out frequency (p < 0.05). The number of family members was significantly correlated only with the frequency of dining out. The frequency of dining out decreased with increased number of family members (p < 0.05). The subjects who were interested in dietary life showed a high level of interest in cooking (p < 0.01), highly assessed their own cooking skills (p < 0.01) and showed a significant increase in the frequency of home cooking (p < 0.05).
Influences of the age, interest in dietary life, interest in cooking, and self-assessed cooking skills, which were significantly correlated with knowledge on LID and self-efficacy and perceived barriers for practicing LID, on knowledge, self-efficacy, and perceived barriers were analyzed through ANOVA. The LID knowledge score was the highest (4.9 points) in the group aged below 35, followed by the group aged between 36-45 (4.7 points), group aged between 46-55 (4.3 points), and group aged above 56 (3 points). The knowledge score generally decreased with higher age, but this result did not show a statistical significance (Table 7). The knowledge of LID significantly increased with higher level of education (p < 0.01). Although the subjects that graduated from a high school scored 3.6, the subjects that graduated from a college scored 4.9 and the subjects that graduated from a graduate school scored 5.5. The subjects that answered that they were very interested in dietary life gained knowledge score of 3.8 whereas the subjects that answered that they were very interested or not interested in dietary life scored 3.8, thus verifying that the level of interest in dietary life was unrelated with the knowledge of LID. Furthermore, knowledge of LID was not significantly different by the subject's level of interest in cooking and self-assessed cooking skills.
The self-efficacy for practicing LID was the lowest in the group aged below 35 (55.3 points), followed by the group aged between 46-55 (62.4 points), group aged between 36-45 (60.8 points), and the group aged above 56 (59 points) (p = 0.053). Self-efficacy did not significantly differ by the education level of the respondents (Table 7). However, the group that was very interested in dietary life showed the significantly higher self-efficacy score (70 points) than any other groups (p = 0.001). The self-efficacy scores were 59, 56.9, and 55 for the group that showed interest in dietary life, the group that showed average interest in dietary life, and the group that was uninterested in dietary life, respectively. Although the self-efficacy score was not significantly different by subjects' interest in cooking, the score decreased with lower interest. The self-efficacy for practicing LID were significantly different by self-assessed cooking skills (p = 0.002). The group that evaluated their own cooking skills to be good obtained a self-efficacy score of 66. The subjects that evaluated their cooking skills to be fair or poor showed self-efficacy scores of 57.9 and 56, respectively.
The perception of thyroid cancer patients regarding the personal and environmental barriers related with LID was the highest in the group aged above 56, followed by the group aged below 35, group aged between 36-45, and group aged between 46-55. However there was no significant difference (Table 7). The level of perceived barriers did not differ significantly according to the level of education. However, the group that was very interested in dietary life showed a significantly lower score for the perceived barriers (39.5 points) (p < 0.05). The scores for perceived barriers were 44, 46, and 50 for the group that presented interest in dietary life, the group that presented average interest in dietary life, and the group that was uninterested in dietary life, respectively. The level of interest in cooking also influenced perceived barriers. The score for perceived barriers was 43.5 in the group showing high interest in cooking and the score increased to 44.5 and 50 in the group the showed average interest in cooking and the group that was uninterested in cooking, respectively. The subjects with higher interest in cooking perceived less barriers for LID (p = 0.057). The level of perceived barriers for LID significantly differed by the self-assessed cooking skills (p = 0.009). The group that assessed their cooking skills to be good scored 39.8 for perceived barriers. On the other hand, the score increased to 45.7 and 47.6 in the groups that assessed their cooking skills to be fair or poor, respectively. Thus, the results showed that the awareness of personal and environmental factors that make practicing LID difficult was more affected by the level of interest in dietary life, interest in cooking, and self-assessed cooking skills than the level of education or age.
It is important for thyroid cancer patients to practice LID for a limited period of time before receiving RAI therapy to achieve greater therapeutic effects and quick recovery [16]. Thus, clinical dietitians should apply various strategies in an education program in order to deliver knowledge related with LID to thyroid cancer patients and help the patients to practice LID. This study investigated the knowledge level of thyroid patients regarding LID and analyzed self-efficacy, an important factor emphasized in the nutrition education theories, as well as potential barriers in practicing LID. In addition, factors were examined that influence these variables and an educational strategy was identified for enhancing practice of LID.
The thyroid cancer patients that participated in this study scored an average of 4.5 out of 10 points for knowledge related with LID. Although the knowledge on LID increased with higher level of education, the patients generally possessed low level of knowledge. Thus, enhancing the knowledge on LID should be an important educational goal regardless of the educational background of the patients. Furthermore, although knowledge scores significantly decreased with increased age, there was no significant relationship with the self-efficacy of practicing LID and the perceived barriers.
Although the patients that were very interested in dietary life were expected to show high level of nutritional knowledge, the correlation between the two variables was not significant. It can be explained by the fact that LID restricts only iodine, a nutrient that is not emphasized in the nutrition education for general population. As iodine is not evenly dispersed in various types of food but is rather intensively contained in certain foods, such as seaweeds, it is important to provide education on foods with high iodine content and low iodine content [25]. The respondents generally possessed a low level of knowledge on the food types that are allowed and restricted for LID, except for their knowledge regarding the high iodine content in seaweeds. In particular, only 37% of the subjects knew that fish cakes and hams were high in iodine. The iodine consumption varied by area and food culture. Whereas the main sources of iodine have been reported to be seaweeds, fish, milk, and dairy products in Korea, they are known as milk, dairy products, cereal, iodized salt, and bakery products in the U.S. and European countries [25]. Seaweeds were also a preferred food by most respondents in this study. The knowledge of dairy products and processed food must be emphasized in LID education since the consumption of the products have increased in Korea.
More than half of the subjects did not know that they were allowed to eat kimchi prepared by refined salt without using sea salt. The subjects did not fully understand that sea salt was restricted in LID due to high iodine content but refined salt with low iodine content was permitted [24]. In particular, most subjects falsely understood LID as a low-sodium diet. Previous studies have reported that thyroid cancer patients have perceived LID boring and difficult to follow [11,26]. Seasoning is an important factor in determining the taste of food. Therefore, unnecessary practice of low-sodium diet can reduce the taste of food, which leads lower nutrient intake, and even result in hyponatraemia among elderly patients aged above 65 [27-29]. Clinical dietitians should recognize the potential side effects of LID [26]. They also should emphasize the restricted intake of sea salt and educate patients on the allowed salt types and the fact that LID is not equal to a low-sodium diet. As a considerable number of the subjects falsely understand that sugar and chili powder were not allowed in the LID, it is important to educate subjects on the allowed seasonings by using specific examples.
The practice of LID is an important factor for achieving success in RAI therapy. It is known that a compliance with LID decreases with stricter LID [16]. In a study that compared the success rate of initial 131I ablation among Korean thyroid cancer patients by stringency of LID, it was observed that certain patients did not follow the recommended diet guidelines in the very strict LID group that restricted such stable foods for Koreans as rice and soybean products [16]. The education programs provided for thyroid cancer patients in many hospitals tend to emphasize the foods that be restricted. This approach makes patients perceive many barriers in food selection and consumption. In particular, as LID is recommended for a relatively short period of 2-4 weeks, the patients who feel restricted tend to give up consuming various foods or excessively depend on certain foods rather than to make efforts to consume various foods excluding only foods that are not allowed on LID, which results in nutritional problems. Thus, in the nutritional education on LID, it should be emphasized that LID only restricts the intake of iodine and requires sufficient ingestion of other foods and nutrients. Also, the allowed foods should be explained in detail to help patients achieve a balanced intake of various foods.
Many patients experience difficulties in understanding and practicing LID due to psychological and physical stress and the lack of knowledge on LID. Higher self-efficacy, which is defined as the confidence in performing certain behaviors, promotes more behavioral changes [18]. Behaviors that showed high level of self-efficacy in relation to LID practice include the intake of various fruits and vegetables excluding seaweeds and the intake of potatoes and sweet potatoes as snacks instead of commercial bakery products. These foods are recommended in LID due to their low iodine content. Furthermore, the subjects showed a relatively high level of self-efficacy for restricting the intake of eggs, milk, dairy products, and processed foods. Thus, LID practice related to those foods can be improved by increasing knowledge on the foods through education.
On the contrary, the self-efficacy for preparing delicious meals without using sea salt was relatively low. By surveying the personal and environmental factors perceived as barriers during the 2-week LID, 'I am not knowledgeable about how to prepare low-iodine menus' was identified as the greatest barrier. As indicated in the knowledge assessment, many thyroid cancer patients mistake the restriction of sea salt as the restriction of all types of salt, thus thinking that it is impossible to cook delicious food without using salt. Therefore, patients should acquire proper knowledge (e.g.: types of salt allowed on LID) through education to reduce the perceived barriers for this behavior and achieve higher self-efficacy.
Low self-efficacy was also reported in the item 'I am confident in using low-iodine seasonings and condiments instead of using soybean paste and soy sauce that contain sea salt.' The low self-efficacy of the item can be explained by with the fact that soybean paste and soy sauce are main seasonings in the Korean food culture and that the subjects lacked knowledge and experience of using other sauces and condiments. The results showed that patients needed to be provided with information on low-iodine seasonings that can enhance flavor, such as refined salt, vinegar, sugar, chili powder, mustard, garlic, sesame, and herb, and be educated on the method of using these seasonings. Except the barriers related with cooking, the other barrier items were rated low: lack of time for practicing LID, working conditions, and frequent dining out, and length of LID duration.
Overall, the subjects were confident in avoiding food with high iodine content and selecting food with low iodine content and did not view these items as barriers. On the other hand, the subjects showed a low level of confidence for cooking with the relevant food types. To increase the self-efficacy for cooking low-iodine food and decrease perceived barriers related to cooking, education and training are required to help patients prepare delicious meals without using sea salt or seasonings with high iodine content. This study discovered that the subjects' interest in dietary life and self-assessed cooking skills were factors that influenced self-efficacy for practicing LID. The subjects with high interest in dietary life and good self-assessed cooking skills presented higher self-efficacy for practicing LID. Furthermore, the barriers related with the practice of LID were lower with higher interest in dietary life, interest in cooking, and self-assessed cooking skills. To enhance the subjects' ability to practice LID, it is recommended to incorporate experiential components into educational programs in addition to the lecture-type education provided in many hospitals.
The perceived barriers for LID significantly decreased with higher self-efficacy for LID, and self-efficacy and perceived barriers were significantly correlated with the interest in dietary life, interest in cooking, self-assessed cooking skills, and frequency of dining out. Yoo et al. [16] assumed that the RAI therapy success rate would be lower among subjects with jobs, in that these subjects would have difficulties in cooking the low-iodine meals. However, no significant difference was found in the actual success rate. This is probably because the study did not investigate whether there was another person to prepare low-iodine meals for the working patients.
According to a survey conducted on Korean patients with diseases requiring diet therapy, 81.8% of the patients responded that they were in need or in extreme need of diet therapy. However, only 6.1% answered that they were practicing diet therapy [30]. The reasons for the difficulty of practicing diet therapy mentioned by patients included inconvenience of cooking separate meals, poor taste of food due to restricted cooking methods and ingredients, and difficulty in cooking therapeutic diet. Dietitians also mentioned the similar reasons: inconvenience of cooking separate meals, no opportunity to learn cooking methods for therapeutic diet, and poor taste of food due to restricted cooking methods and ingredients.
In this regard, the nutrition education provided for patients should not only include the roles of certain nutrients, but also include how to select proper foods and prepare meals for the diet therapy. It was reported that it was difficult for patients lacking cooking knowledge and skills to practice the educational content if the curriculum did not include detailed explanations or demonstrations on how to prepare meals [31].
One of the characteristics of recent nutrition education programs is incorporating cooking class. A cooking class has been reported to be effective for increasing the intake of fruits and vegetables among children and adults and increasing the participation rate of adults in nutrition education programs [32-34]. Thus, if the method for cooking tasty low-iodine meals is included in the LID education program for thyroid cancer patients, the education program will effectively enhance the self-efficacy of patients and help them overcome barriers for practicing LID.
Figures and Tables
References
1. Ministry of Health & Welfare, Korea Central Cancer Registry, National Cancer Center Annual report of cancer statistics in Korea in 2009. 2011. Publication No. 11-1352000-000145-10.
2. Simpson WJ, Panzarella T, Carruthers JS, Gospodarowiez MK, Sutcliffe SB. Papillary and follicular thyroid cancer: impact of treatment in 1578 patients. Int J Radiat Oncol Biol Phys. 1988. 14:1063–1075.

3. DeGroot LJ, Kaplan EL, McCormick M, Straus FH. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab. 1990. 71:414–424.

4. Samaan NA, Schultz PN, Hickey RC, Goepfert H, Haynic TP, Johnston DA, Ordonez NG. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab. 1992. 75:714–720.

5. Maxon HR, Thomas SR, Hertzberg VS, Kereiakes JG, Chen IW, Sperling MI, Saenger EL. Relation between effective radiation dose and outcome of radioiodine therapy for thyroid cancer. N Engl J Med. 1983. 309:937–941.

6. Maxon HR, Thomas SR, Samaratunga RC. Dosimetric considerations in the radioiodine treatment of macrometastases and micrometastases from differentiated thyroid cancer. Thyroid. 1997. 7:183–187.

7. Uyttersprot N, Pelgrims N, Carrasco N, Gervy C, Maenhaut C, Dumont JE, Miot F. Moderate doses of iodide in vivo inhibit cell proliferation and the expression of thyroperoxidase and Na +/I- symporter mRNAs in dog thyroid. Mol Cell Endocrinol. 1997. 131:195–203.

8. De la Vieja A, Dohan O, Levy O, Carrasco N. Molecular analysis of the sodium/iodide symporter: impact on thyroid and extrathyroid pathophysiology. Physiol Rev. 2000. 80:1083–1105.

9. Goslings BM, Hannon R. The effect of a low-iodine diet on 131-I therapy in follicular thyroid carcinoma. Netherlands J Med. 1973. 16:136–137.
10. Goslings BM. Proceedings : effect of a low iodine diet on 131-I therapy in follicular thyroid carcinomata. J Endocrinol. 1975. 64:30.
11. Maxon HR, Thomas SR, Boehringer A, Drilling J, Sperling MI. Low iodine diet in I-131 ablation of thyroid remnants. Clin Nucl Med. 1983. 8:123–126.

12. Morris LF, Wilder MS, Waxman AD, Braunstein GD. Reevaluation of the impact of a stringent low-iodine diet on ablation rates in radioiodine treatment of thyroid carcinoma. Thyroid. 2001. 11:749–755.

13. Pluijmen MJ, Eustatia-Rutten C, Goslings BM, Stokkel MP, Arias AM, Diamant M, Romijn JA, Smit JW. Effects of low-iodine diet on postsurgical radioiodide ablation therapy in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf). 2003. 58:428–435.

14. Roh JH, Kim BI, Ha JS, Chang SJ, Shin HY, Choi JH, Kim DM, Kim CS. Comparison of urine iodine/creatinine ratio between patients following stringent and less stringent low iodine diet for radioiodine remnant ablation of thyroid cancer. Nucl Med Mol Imaging. 2006. 40:322–326.
15. Choi JH, Kim HI, Park JW, Song EH, Ko BJ, Cheon GJ, Kim BI. Analysis of urine iodine excretion decrease by two-week stringent low iodine diet for remnant thyroid ablation with radioactive iodine in Korean patients with thyroid cancer: prospective study. Nucl Med Mol Imaging. 2008. 42:375–382.
16. Yoo ID, Kim SH, Seo YY, Oh JK, O JH, Chung SK. The success rate of initial 131I ablation in differentiated thyroid cancer: comparison between less strict and very strict low iodine diets. Nucl Med Mol Imaging. 2012. 46:34–40.

17. Son SM, Lee KH, Kim KW, Lee YK. Nutrition education and practice. 2007. Seoul: Life Science.
18. Koo JY, Kim KW, Kim CL, Park DY, Park HR. Theory and practice of nutrition education. 2007. Seoul: Power Book.
19. Miller CK, Edwards L, Kissling G, Sanville L. Evaluation of a theory-based nutrition intervention for older adults with diabetes mellitus. J Am Diet Assoc. 2002. 102:1069–1081.

20. Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: application of the health belief model. J Nutr Educ Behav. 2003. 35:260–267.

21. Ko SY, Kim KW. Nutrition label use, self-efficacy, snacking and eating behavior of middle school students in Kyunggi Area. Korean J Community Nutr. 2010. 15:513–524.
22. Na SY, Ko SY, Eom SH, Kim KW. Intakes and beliefs of vegetables and fruits, self-efficacy, nutrition knowledge, eating behavior of elementary school students in Kyunggi area. Korean J Community Nutr. 2010. 15:329–341.
23. Poddar KH, Hosig KW, Anderson ES, Nickols-Richardson SM, Duncan SE. Web-based nutrition education intervention improves self-efficacy and self-regulation related to increased dairy intake in college students. J Am Diet Assoc. 2010. 110:1723–1727.

24. ThyCa: Thyroid Cancer Survivors' Association. Low-iodine cookbook: guidelines and tips for the low-iodine diet used for a short time when preparing to receive radioactive iodine. 2010. cited 2012 April 15. 7th ed. Available from www.thyca.org.
25. Lee H, Min H. Iodine intake and tolerable upper intake level of iodine for Koreans. Korean J Nutr. 2011. 44:82–91.

26. Sawka AM, Ibrahim-Zada I, Galacgac P, Tsang RW, Brierley JD, Ezzat S, Goldstein DP. Dietary iodine restriction in preparation for radioactive treatment or scanning in well-differentiated thyroid cancer: a systematic review. Thyroid. 2010. 20:1129–1138.

27. Kim MW. Disease Focus for clinical dietitians - Thyroid cancer: radioactive iodine therapy and management. Nutrition and Dietetics. 2012. 35:22–25.
28. Krishnamurthy VR, McDougall IR. Severe hyponatremia: a danger of low-iodine diet. Thyroid. 2007. 17:889–892.

29. Shakir MK, Krook LS, Schraml FV, Hays JH, Clyde PW. Sympomatic hyponatremia in association with a low-iodine diet and levothyroxine withdrawal prior to I131 in patients with metastatic thyroid carcinoma. Thyroid. 2008. 18:787–792.

30. Yoo CH. Need assessment and quality analysis of cook/chill-based menus for developing a home-delivered therapeutic meal service model. 2008. Seoul: Seoul Women's University;[Doctoral Dissertation].
31. Byrd-Bredbenner C. Food preparation knowledge and attitudes of young adults: Implications for nutrition practices. Topics Clin Nutr. 2004. 19:154–163.
32. Liquori T, Koch PD, Contento IR, Castle J. The cookshop program: outcome evaluation of a nutrition education program linking lunchroom food experiences with classroom cooking experience. J Nutr Edu. 1998. 30:302–313.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download