Abstract
Background
In this study, we aimed to compare repeated resection and radiation treatment, such as Gamma knife radiosurgery (GKRS) or conventional radiotherapy (RT), and investigate the factors influencing treatment outcome, including overall survival (OS), progression-free survival (PFS), and complication rates.
Methods
We retrospectively reviewed 67 cases of recurred intracranial meningiomas (repeated resection: 36 cases, radiation treatment: 31 cases) with 56 months of the median follow-up duration (range, 13–294 months).
Results
The incidence of death rate was 29.9% over follow-up period after treatment for recurred meningiomas (20/67). As independent predictable factors for OS, benign pathology [hazard ratio (HR) 0.132, 95% confidence interval (CI) 0.048–0.362, p<0.001] and tumor size <3 cm (HR 0.167, 95% CI 0.061–0.452, p<0.001) were significantly associated with a longer OS. The incidence of progression rate was 23.9% (16/67). Only treatment modality was important for PFS as an independent predictable factor (GKRS/RT vs. open resection; HR 0.117, 95% CI 0.027–0.518, p<0.005). The complication rate was 14.9% in our study (10/67). Larger tumor size (≥3 cm, HR 0.060, 95% CI 0.007–0.509, p=0.010) was significant as an independent prognostic factor for development of complications. Although treatment modality was not included for multivariate analysis, it should be considered as a predictable factor for complications (p=0.001 in univariate analysis).
Conclusion
The role of repeated resection is questionable for recurred intracranial meningiomas, considering high progression and complication rates. Frequent and regular imaging follow-up is required to detect recurred tumor sized as small as possible, and radiation treatment can be a preferred treatment.
Meningioma has the second highest incidence rate among primary tumors occurring in the central nervous system (CNS), comprising 13–16% of intracranial tumors [12]. Based on the fourth classification of World Health Organization (WHO) in 2007, 92% of meningiomas are divided into benign tumors (WHO grade I) that grows comparatively slowly [345]. They arise from the arachnoid “cap” cells of the arachnoid villi in the meninges and typically attached to the dural broad base [6]. Some of them invade skull or cause hyperostosis to subjacent bone. Gamma knife radiosurgery (GKRS) is recognized as a good treatment option for relatively small meningioma with actuarial tumor control rate of 97.9% at 5 years post-GKRS [7]. However, complete surgical removal (Simpson grade I–III) remains the first treatment option of meningioma despite recurrence can be occur in histologically benign meningiomas on macroscopic total resection and removal of dural attachment and abnormal bone (Simpson grade I). Nanda et al. [8] revealed that, in benign meningioma, the recurrence rate in Simpson grades 0/I group was 2.9%, otherwise in Simpson grades II–IV group, the recurrence rate was 31%. Furthermore, the pathological grade is also important for prediction of recurrence. In atypical meningioma, the overall recurrence rate in Simpson grades I/II resection was 31%. In grades III/IV, the overall recurrence rate was 73%, and this high recurrence rate in these groups was confined within 5 years.
Despite high clinical relevance of recurrence, the proper strategy for the diagnosis and treatment of recurred meningiomas has not been fully established. In the present study, we analyzed treatment outcomes of patients with recurred meningiomas to determine the predictors for survival, progression and postoperative complications.
This study was approved by the Institutional Review Board of the hospital (CNUHH-2017-97) and written informed consent was obtained from patients or their legal surrogates for using clinical data. A retrospective study was performed on 884 patients who received surgery and were histopathologically confirmed as a meningioma in our hospital from June 1993 to November 2011. Of the 884 meningioma patients, 75 patients (8.5%) were treated as recurrent meningiomas. Some patients who had partial uncertain or omitted records were excluded and finally 67 cases were enrolled in the study; open resection (n=36), radiation treatment [GKRS or conventional radiotherapy (RT), n=31].
The location and size of the craniotomy was determined for each case, and navigation system was introduced to correctly localize the tumors. In some cases, the feeding vessels and tumor vascularity were evaluated by cerebral angiography before surgery. In the cases with high bleeding risk, preoperative embolization was conducted to minimize the hemorrhage during surgery and ease resection of the tumor. Whenever possible, gross total resection (GTR) with removal or coagulation of involved dura mater was attempted. However, remnant tumor was inevitable in case in which it had invaded the venous sinus or when it was very adherent to the cranial nerves, cerebral arteries and functionally important cortex. GKRS was performed with the Leksell Gamma Knife (model C or Perfexion, Elekta AB, Stockholm, Sweden). The median maximal dose was 26.5 Gy (range, 18–36 Gy), with a median marginal tumor dose of 13.2 Gy (range, 9–18 Gy) at the 45–50% isodose line.
The clinical and radiological data of the enrolled patients were retrospectively reviewed. Clinicoradiological factors including, age, sex, location, size, perilesional edema, calcification, magnetic resonance (MR) imaging characteristics, Simpson grade, initial neurologic symptoms, and pathology were retrospectively analyzed. The size of the tumor indicates the maximal diameter on 3-dimensional T1-weighted MR images with enhancement. Peritumoral edema, evaluated by axial T2-weighted MR images, were used to classify the patients into 2 groups [none or mild (<5 mm in edema thickness) vs. moderate to severe (≥5 mm in edema thickness)]. The extent of tumor resection was classified in accordance with the Simpson's classification. Simpson's grade I or II resection without remnant tumor on follow-up MR imaging was defined as GTR. WHO classification system was applied for pathological grade for all tumors. Newly-developed neurological deficits or aggravated pre-existing deficits after treatment were regarded as treatment-related complications. In this study, we defined the complication as permanent neurologic deficit or sequelae, not transient. If the problem persisted longer than 6 months or needed subsequent surgical operation, it was regarded as a permanent complication. To evaluate tumor recurrence, postoperative follow-up MR imaging was obtained from all patients 6 months after surgery and then annual imaging for the rest of the patient's life. On follow-up MR imaging, a newly-enhanced mass in a completely resected case or a re-growing symptomatic mass in an incompletely resected case was regarded as progression.
Overall survival (OS) was calculated from the date of treatment of recurrence until death, or until the date of the last visiting for patients who were still alive. Progression-free survival (PFS) rates calculated from date of treatment for recurrence to date of first recurrence in complete resection case or regrowth in remnant case, or last follow-up in patients with no recurrence or regrowth were estimated with the Kaplan-Meier method and compared with the log-rank test. For the multivariate analysis, independent prognostic factors were determined using the Cox's proportional hazards model. The comparison of a permanent complication occurrence and a categorical variable was done by a Chi-square test or Fisher-exact probability test. Furthermore, binary logistic regression test was applied for multivariate analysis. All statistical analyses were performed using SPSS version 20.0 for Windows (IBM Corp., Armonk, NY, USA); p<0.05 was considered statistically significant.
Clinicoradiological characteristics of the enrolled 67 patients with recurred meningiomas are summarized in Table 1. Several features at initial operation were also analyzed. Poor resection margin between tumor and normal arachnoid was noted in 27 patients (40.2%) and GTR (Simpson grade I/II) was performed in 48 patients (71.7%). In WHO classification, majority of the patients (42/67, 62.7%) were diagnosed as a WHO grade I. Multi-lobulated tumor was documented in 31 patients (46.2%).
On 2nd treatment, the mean tumor size was 2.1 cm and 29 cases were larger than 3 cm. Most commonly, parasagittal (20.8%), convexity (17.9%), and sphenoidal ridge (11.9%) meningiomas were accounted. Thirty-one patients showed symptoms at recurrence, with headache or dizziness in 8 patients, and cranial nerve symptoms in 13 patients. Median follow-up duration was 56 months (range, 13–294 months). On T2-weighted MR images, 11 cases showed low signal intensity and 11 cases revealed moderate to severe peritumoral edema formation.
The incidence of death rate was 29.9% over follow-up period after treatment for recurred meningiomas (20/67). The 5-, 10-, and 15-year survival rates were 73.1, 70.1, and 70.1%, respectively (Fig. 1A). The results of analyses of the variables correlated with OS are shown in Fig. 1B-F and Table 2.
On univariate analysis, initial pathology, location, size, and postoperative complication showed statistical significance. The more aggressive pathology group (WHO grade II/III) manifested a shorter survival time than the benign group (71.9±12.0 months vs. 148.4±9.6 months, p<0.001). The tumor location was influential factor for survival time [61.8±16.6 months (convexity) vs. 133.5±9.7 months (non-convexity), p=0.014]. The size of tumor was also an important variable in survival time [146.7±10.1 months (group <3 cm) vs. 81.5±11.9 months (group ≥3 cm), p=0.003]. With regard to permanent complication after treatment for recurrence, the presence of complication had a significantly correlation with shorter survival time (44.1±9.6 months vs. 132.3±9.6 months, p=0.011). Our study showed that the patient treated with open resection survived for a shorter period than patients treated with GKRS/RT, with marginal significance (p=0.097). Pretreatment symptom also showed a marginal significance (p=0.099). On multivariate analysis, initial pathology and tumor size were independent predicting factors for survival rate. Benign pathology [hazard ratio (HR) 0.132, 95% confidence interval (CI) 0.048–0.362, p<0.001] and tumor size <3 cm HR 0.167, 95% CI 0.061–0.452, p<0.001) were significantly associated with longer survival rate.
The incidence of progression rate was 23.9% over follow-up period after treatment for recurred meningiomas (16/67). The 5-, 10-, and 15-year PFS were 79.1, 76.1, and 76.1%, respectively (Fig. 2A). The results of analyses of the factors correlated with survival time are shown in Fig. 2B and Table 3. On univariate analysis, only treatment modality for recurred lesion was important for PFS [80.4±11.1 months (open resection) vs. 133.4±7.8 months (GKRS/RT), p=0.001]. This parameter was an independent predictable factor for PFS (GKRS/RT; HR 0.117, 95% CI 0.027–0.518, p<0.005). However, factors such as resection degree, pathological grade, tumor size, and location did not show statistical significance in the statistical analyses.
Permanent complication occurred in 10 patients (14.9%). The most common complication was hemorrhagic change (n=2, 3.0%), followed by hydrocephalus (n=2, 3.0%), and infection (n=2, 3.0%). The results of analyses of the variables that could be correlated with permanent complications are shown in Table 4.
On univariate analysis, tumor size and treatment modality showed statistical significance. Permanent complications were more prevalent in patient with tumor ≥3 cm than those with tumors <3 cm (2.6% vs. 31.0%, p=0.001). Patients treated with open resection had a higher complication rate, as compared to the patients treated with GKRS/RT (27.8% vs. 0%, p=0.001). Multivariate analysis confirmed that larger tumor size (HR 0.060, 95% CI 0.007–0.509, p=0.010) was significant as an independent prognostic factor for development of complications. Although treatment modality was not included for multivariate analysis, it should be considered as one of the predictable factor for complication. Age, sex, preoperative symptoms, WHO grade, resection degree, tumor consistency, and location were not statistically significant.
On comparing result from treatment modalities for recurred meningiomas, few showed significant differences, including size of tumors, re-progression rate, and complication rate. In GKRS/RT, mean size of tumors was 2.2 cm, but 4.3 cm in open resection (p<0.001). Based on larger than 3 cm, the number of open resection was over two-fold higher than those of GKRS/RT (p<0.015). Re-progression rate was 6.5% in GKRS/RT and 38.9% in open resection (p<0.002). Complication rate was 27.8% when treated by open resection; however, there was no complication after GKRS/RT (p<0.001). The Simpson grade or WHO grade were statistically not significant (Table 5).
Meningiomas account for approximately one-third of primary CNS tumors [910]. In the classification of meningiomas based on the WHO grades, benign meningiomas reportedly comprise 92%, atypical meningioma 5–7%, and malignant meningioma 1–3% of the total [1112131415]. Although not all meningiomas warrant treatment, surgery and/or radiation therapy constitutes the initial therapeutic approach [16].
As meningiomas are histologically benign tumors, macroscopic total resection is expected to be curative. However, several meningiomas recur after macroscopic total resection. In WHO grade I meningiomas, 5-year recurrence or progression rates are reported as approximately 10% after complete resection and 45% after non-radical resection [1718]. Van Alkemade et al. [19] showed that OS at 5, 10, 15, and 20 years was 91.5, 81.4, 62.5, and 53.4%, respectively. After 13 years, the observed survival is positioned significantly under the expected survival curve due to excess mortality related to brain tumor or stroke. Recurrence rates at 5, 10, and 15 years were also reported as 18, 26, and 32%, respectively.
Atypical and malignant meningiomas are associated with an increased risk of local recurrence and decreased OS, as compared with WHO grade I meningiomas. Klinger et al. [20] reported that 44% of atypical meningiomas developed clinical-radiologic evidence of recurrence at an average of 32.4 months after surgical resection. In our previous study, overall recurrence rate of atypical meningioma was 25.5% (14% in Simpson's grade I and 37% in Simpson's grade II/III/IV) [21]. In malignant meningiomas, the recurrence rate after complete extirpation is 20–40% by the decade and increases to 40–60% in partial extirpation patients [22]. Statistical significances varied by studies, nevertheless, histologically higher grade meninigioma showed higher recurrence or progress rate.
According to original Simpson's grade, recurrent rates were 9% for grade I, 16% for grade II, and 29% for grade III [23]. This is comparable with results from another cohort and it suggests the remnant tumor cells left behind removed space and that cells could be in continuous proliferation [24]. Some authors propose that a Simpson grade 0 resection can decrease recurrence by additional removal a 2–4 cm outwards each dural margin [2526].
Although the majority occur within the first two to three years after resection, late recurrences are common. Recent studies indicate that adjuvant RT or GKRS after surgery show good outcomes for preventing recurrence, but guidelines of treatment for already recurred meningioma are still not established. In our study, independent predictive factor for longer survival were benign pathology (HR 0.132, 95% CI 0.048–0.362, p<0.001) and tumor size <3 cm (HR 0.167, 95% CI 0.061–0.452, p<0.001). In univariate statistics, tumor location and complication at the first operation showed statistical significance. Treatment modality (open resection vs. radiation treatment) showed marginal significance. In PFS, only radiation treatment was an independent predictive factor (HR 0.117, 95% CI 0.027–0.518, p<0.005). Regarding complication rates, larger than 3 cm size (HR 0.060, 95% CI 0.007–0.509, p=0.010) was a significant independent predictive factor for development of complications. Although treatment modality was not a significant factor, it should be considered as a predictable factor for complication. As shown in Table 5, radiation treatment was better in all parameters than open resection as the treatment modality for recurred lesion.
In addition to surgical resection or radiation treatment, pharmacologic therapy is in use for recurred meningiomas [27]. Mainly antiangiogenic agents such as bevacizumab, vatalanib, and sunitinib have made promising results but they are still in issue to be used clinically [2829]. Other agents including hydroxyurea, epidermal growth factor inhibitor, hormonal therapeutics, α-interferon, and somatostatin receptor agonists have been tried for recurred meningioma [303132]. Up to now, pharmacologic therapy is not first therapeutic option for recurred meningioma and used narrowly for refractory recurrent tumor. However, the solidity of the evidence might soon advance with identification of the pharmacologic target effect.
Major limitation of this study is its retrospective design, which makes many types of bias. Another limitation is inclusion of all WHO grades for studied patients, possibly leading a selection bias for treatment. In addition, the size of recurred tumor may cause another selection bias for treatment modality. The relatively small number of patients and short follow-up duration can be other limitations in current study. Further studies need to be performed prospectively with large numbers of benign pathology for establishing treatment strategy of recurred meningiomas.
In conclusion, although open surgical resection is the treatment choice for symptomatic or large sized meningiomas, it is questionable for recurred tumors, considering high progression and complication rates after repeated open resection. Thus, frequent and regular imaging follow-up is required to detect recurred tumor sized as small as possible, and radiation treatment can be considered as a preferential treatment.
Figures and Tables
Fig. 1
Kaplan-Meier curves showing OS of 67 study patients based on different predictors (overall comparison was estimated using a log-rank test). The number on right lower in each curve represents the p-value. A: Entire patients. B: WHO grade. C: Location. D: Size of tumor. E: Treatment modality for recurrence. F: Postoperative complication. OS, overall survival; GKRS, Gamma knife radiosurgery; RT, radiotherapy.
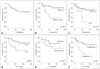
Fig. 2
Kaplan-Meier curves showing PFS of 67 study patients based on different predictors (overall comparison was estimated using a log-rank test). The number on right lower in each curve represents the p-value. A: Entire patients. B: Treatment modality for recurrence. PFS, progression-free survival; GKRS, Gamma knife radiosurgery; RT, radiotherapy.

Table 1
Clinicoradiological characteristics of 67 patients with recurred meningiomas

Table 2
Univariate and multivariate analyses for overall survival from the treatment for recurred meningiomas

Table 3
Univariate and multivariate analyses for progression-free survival from the treatment for recurred meningiomas

Table 4
Univariate and multivariate analyses for postoperative complication from the treatment for recurred meningiomas

Table 5
Comparison of clinicoradiological characteristics according to treatment modalities for recurred meningiomas

Acknowledgments
This study was supported by a grant of Chonnam National University Hospital Research Institute of Clinical Medicine.
References
1. Hoessly GF, Olivecrona H. Report on 280 cases of verified parasagittal meningioma. J Neurosurg. 1955; 12:614–626.

2. Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL. Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg. 1985; 62:18–24.

3. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.

4. Willis J, Smith C, Ironside JW, Erridge S, Whittle IR, Everington D. The accuracy of meningioma grading: a 10-year retrospective audit. Neuropathol Appl Neurobiol. 2005; 31:141–149.

5. Ojemann SG, Sneed PK, Larson DA, et al. Radiosurgery for malignant meningioma: results in 22 patients. J Neurosurg. 2000; 93:Suppl 3. 62–67.

6. Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics. 1991; 11:1087–1106.

7. Kollová A, Liscák R, Novotný J Jr, Vladyka V, Simonová G, Janousková L. Gamma Knife surgery for benign meningioma. J Neurosurg. 2007; 107:325–336.

8. Nanda A, Bir SC, Konar S, et al. Outcome of resection of WHO Grade II meningioma and correlation of pathological and radiological predictive factors for recurrence. J Clin Neurosci. 2016; 31:112–121.

9. Ostrom QT, Gittleman H, Fulop J, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008-2012. Neuro Oncol. 2015; 17:Suppl 4. iv1–iv62.

10. Wrensch M, Minn Y, Chew T, Bondy M, Berger MS. Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro Oncol. 2002; 4:278–299.

11. Al-Mefty O, Kadri PA, Pravdenkova S, Sawyer JR, Stangeby C, Husain M. Malignant progression in meningioma: documentation of a series and analysis of cytogenetic findings. J Neurosurg. 2004; 101:210–218.

12. Lim YS, Kim MK, Park BJ, Kim TS, Lim YJ. Long term clinical outcomes of malignant meningiomas. Brain Tumor Res Treat. 2013; 1:85–90.

13. Harris AE, Lee JY, Omalu B, Flickinger JC, Kondziolka D, Lunsford LD. The effect of radiosurgery during management of aggressive meningiomas. Surg Neurol. 2003; 60:298–305. discussion 305.
14. Jung HW, Yoo H, Paek SH, Choi KS. Long-term outcome and growth rate of subtotally resected petroclival meningiomas: experience with 38 cases. Neurosurgery. 2000; 46:567–574. discussion 574-5.

15. Kallio M, Sankila R, Hakulinen T, Jääskeläinen J. Factors affecting operative and excess long-term mortality in 935 patients with intracranial meningioma. Neurosurgery. 1992; 31:2–12.

16. Chamberlain MC. Treatment of meningioma, including in cases with no further surgical or radiotherapy options. Oncology (Williston Park). 2015; 29:369–371.
18. Gondi V, Tome WA, Mehta MP. Fractionated radiotherapy for intracranial meningiomas. J Neurooncol. 2010; 99:349–356.

19. van Alkemade H, de Leau M, Dieleman EM. Impaired survival and long-term neurological problems in benign meningioma. Neuro Oncol. 2012; 14:658–666.

20. Klinger DR, Flores BC, Lewis JJ, et al. Atypical meningiomas: recurrence, reoperation, and radiotherapy. World Neurosurg. 2015; 84:839–845.

21. Moon HS, Jung S, Jang WY, Jung TY, Moon KS, Kim IY. Intracranial Meningiomas, WHO Grade II: Prognostic Implications of Clinicopathologic Features. J Korean Neurosurg Soc. 2012; 52:14–20.

22. Adegbite AB, Khan MI, Paine KW, Tan LK. The recurrence of intracranial meningiomas after surgical treatment. J Neurosurg. 1983; 58:51–56.

23. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957; 20:22–39.

24. Giombini S, Solero CL, Morello G. Late outcome of operations for supratentorial convexity meningiomas. Report on 207 cases. Surg Neurol. 1984; 22:588–594.

25. de Vries J, Wakhloo AK. Repeated multifocal recurrence of grade I, grade II, and grade III meningiomas: regional multicentricity (primary new growth) or metastases? Surg Neurol. 1994; 41:299–305.

26. Borovich B, Doron Y, Braun J, et al. Recurrence of intracranial meningiomas: the role played by regional multicentricity. Part 2: Clinical and radiological aspects. J Neurosurg. 1986; 65:168–171.

27. Nabors LB, Portnow J, Ammirati M, et al. Central nervous system cancers, version 2.2014. Featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2014; 12:1517–1523.
28. Kaley TJ, Wen P, Schiff D, et al. Phase II trial of sunitinib for recurrent and progressive atypical and anaplastic meningioma. Neuro Oncol. 2015; 17:116–121.

29. Lou E, Sumrall AL, Turner S, et al. Bevacizumab therapy for adults with recurrent/progressive meningioma: a retrospective series. J Neurooncol. 2012; 109:63–70.

30. Chamberlain MC, Glantz MJ. Interferon-alpha for recurrent World Health Organization grade 1 intracranial meningiomas. Cancer. 2008; 113:2146–2151.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download