Abstract
Anaplastic large T-cell lymphoma (ALCL) encompasses different clinical entities that can be aggressive or localized. Scalp anaplastic lymphoma kinase (ALK)-negative ALCL is considered a localized lymphoma, and usually extends to the regional lymph nodes; intracranial invasion is rare. A 74-year-old woman was diagnosed with scalp ALK-negative ALCL, but did not exhibit invasion of the lymph nodes. Computed tomography and magnetic resonance imaging revealed intracranial masses with bony erosions. We treated the patient using CHOP chemotherapy and achieved short-term regression of the scalp and intracranial lesions. However, the patients ultimately died of pneumonia during the pancytopenic period. Therefore, caution must be exercised when treating scalp ALK-negative ALCL with intracranial invasion.
Primary non-Hodgkin lymphoma of the skull and scalp very rarely exhibits intracranial and extracranial extensions. However, this tumor can mimic other intracranial tumors, such as neurofibromatosis type II or multiple meningioma. The prognosis varies according to the pathology, although these tumors seldom develop intracranial lesions and rarely cause death. Based on the rarity of intracranial invasion, we report our experience with a case of anaplastic lymphoma kinase (ALK)-negative anaplastic large T-cell lymphoma (ALCL) and intracranial invasion.
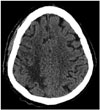
A 74-year-old woman presented with a 3-month history of disorientation without B symptoms. Our physical examination revealed diffuse and irregular areas with rounded scalp swelling at the right frontal side, but no tenderness or discharge. The largest mass was 10×7 cm, and all masses were soft, easily movable, and exhibited no pigmentation. We tried to take a picture of the scalp lesion, but the patient's family objected. We also performed a whole-body examination, but failed to identify any other skin lesions. Neurological examinations revealed that the patient had impaired recent memory, with disorientation regarding the time and place. Enhanced computed tomography (CT) subsequently revealed a homogenous well-enhanced scalp mass and multiple intracranial masses in the right frontal and parietal lobes, with bony erosions. Magnetic resonance imaging also revealed multiple homogenous enhanced masses that were similar to meningioma, with edematous changes surrounding the intracranial masses, and that the scalp mass exhibited central necrosis (Fig. 1). We performed surgical biopsy under local anesthesia at the right frontal scalp, and the gross finding was a yellowish and rubbery mass. We also performed routine laboratory tests, which revealed all normal findings, and a bone marrow biopsy, which did not reveal any evidence of bone marrow involvement. Chest, abdominal, and pelvic CT were also performed, although we did not detect metastasis to the lymph nodes or other organs. Therefore, we did not perform positron emission tomography-CT.
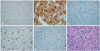
The pathological findings were negative for ALK, positive for CD20, positive for CD30, positive for CD79a, positive for CD138, and positive during hematoxylin and eosin staining (×400) (Fig. 2).
We assumed that the patient had stage IVA (Ann Arbor system; The American Joint Committee on Cancer, Chicago, IL, USA) lymphoma and consulted our Department of Hematology and Oncology. Based on this consultation, we treated the patient using CHOP chemotherapy (cyclophosphamide, doxorubicin, vincristine, and prednisolone) and dexamethasone to control the brain edema. The chemotherapy achieved regression of the scalp and intracranial lesions (Fig. 3), although the patient subsequently developed pancytopenia and pneumonia. The patient ultimately died at 3 weeks after the first chemotherapy cycle.
The definition of ALCL has evolved since its original description by Stein et al. [1] in 1985, and ALCL is currently considered a type of non-Hodgkin lymphoma involving aberrant T-cells [2]. This tumor is characterized by large anaplastic lymphoid cells with uniform strong expression of CD30, and exhibits a tendency to grow cohesively and invade lymph node sinuses [3]. ALCL usually starts as one or a few skin tumors with variable sizing (diameter: <1 inch to several inches) and is typically observed in 50–69-year-old individuals, although it can also occur in children. The frequency of ALCL is 2-fold greater among men (vs. women). In most cases, the tumor does not spread beyond the skin and the prognosis is very good, with the presence of the ALK protein defining a subgroup of patients who respond very well to standard chemotherapy [3]. However, several studies have demonstrated that patients with ALK-negative ALCL have a poorer prognosis, compared to patients with ALK-positive ALCL [2]. In the present case, the tumor mimicked other tumors, such as neurofibromatosis type II and multiple meningioma. For example, the magnetic resonance imaging revealed an extensive, homogeneously enhanced, extra-axial dura-based mass (similar to meningioma), which exhibited an isointense signal on the T1-weighted images and a low-intensity signal on the T2-weighted images of the intracranial lesions. Moreover, the lesions were restricted on the diffusion-weighted images.
Primary non-Hodgkin's lymphoma is rare in the central nervous system (CNS), as it accounts for only 1% of intracranial tumors [4]. In addition, most primary CNS lymphomas are B-cell type tumors and are located intra-axially. Furthermore, T-cell tumors account for 1–3.6% of all primary CNS lymphomas. However, several reports have described lymphomas arising from the skull base, typically in the apical clivus and sella regions [2456]. In 2012, Martin et al. [7] reported a case with scalp and intracranial vault masses, although the tumor was B-cell lymphoma and the patient experienced an excellent prognosis (survival: 12 years).
Another case, Yeung et al. [8] reported a case with ALK-negative ALCL in traumatic injury of scalp. The patients not had any symptom except ulcerated scalp lesion. On biopsy of ulcerated scalp lesion, the patients diagnosed ALK-negative ALCL. The patient treated chemotherapy and radiation therapy, but after 2 months died of pneumonia.
Unfortunately, we had considered the ALCL to be a direct extension from skin to the bone and intracranial lesions, and did not think to perform a biopsy of the intracranial lesions, which limits our ability to comment on this aspect of the case.
There are three possible pathophysiological routes for intracranial and extracranial extension. First, most lymphomas exhibit hematogenous spread and direct extension from adjacent bone metastasis or through centripetal growth along the neurovascular bundles. Our patient exhibited multiple intracranial and extracranial masses with connected bony erosions in the same area, although there was no evidence of metastasis to other internal organs or lymph nodes. Second, the intracranial and extracranial masses may develop as a double primary tumor, although the probability of this route is low, based on the rarity of lymphoma. However, we did not perform biopsy of the intracranial mass, and we cannot definitively exclude the possibility of double primary tumors. Third, it is possible that we did not identify the primary site and extranodal spread from the primary site. However, the rate of extranodal spread is low for ALK-negative ALCL, and the CNS is only involved in 1% of these cases [3].
In the present case, we suspect that the patient's poor prognosis was related to her old age, general weakness because of decreased activity, and complications of the CHOP chemotherapy. For example, the patient developed pancytopenia and fever 7 days after starting the chemotherapy. Thus, she had an increased risk of infection as a side effect of the chemotherapy, subsequently developed pneumonia, and ultimately died.
In conclusion, scalp ALK-negative ALCL can infrequently spread to the intracranial and extracranial spaces, although these patients typically have a good prognosis. The chemotherapy in the present case achieved short-term resolution of the intracranial lesions and extracranial mass, although the patient ultimately died of pneumonia during the pancytopenic period at 3 weeks after starting the CHOP chemotherapy. Therefore, caution must be exercised when treating scalp ALK-negative ALCL with intracranial invasion, in order to avoid similar poor outcomes.
Figures and Tables
Fig. 1
Computed tomography findings. A: Non-enhanced brain computed tomography reveals multiple scalp and intracranial masses at the right frontal lobe. B: Enhanced brain computed tomography reveals homogenous well-enhanced lesions that appeared similar to multiple meningioma. C: Computed tomography reveals bony erosions at the right frontal area. D: T2-weighted magnetic resonance imaging reveals edema in the right parietal lobe. E: T1-weighted magnetic resonance imaging reveals central necrosis in the right scalp lesion.

References
1. Stein H, Mason DY, Gerdes J, et al. The expression of the Hodgkin's disease associated antigen Ki-1 in reactive and neoplastic lymphoid tissue: evidence that Reed-Sternberg cells and histiocytic malignancies are derived from activated lymphoid cells. Blood. 1985; 66:848–858.

2. Medeiros LJ, Elenitoba-Johnson KS. Anaplastic large cell lymphoma. Am J Clin Pathol. 2007; 127:707–722.

3. Savage KJ, Harris NL, Vose JM, et al. ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project. Blood. 2008; 111:5496–5504.

4. Kim MY, Kim SM, Chung SY, Park MS. Dural marginal zone lymphoma confused with meningioma en plaque. J Korean Neurosurg Soc. 2007; 42:220–223.
5. Yoon SH, Paek SH, Park SH, Kim DG, Jung HW. Non-Hodgkin lymphoma of the cranial vault with retrobulbar metastasis mimicking a subacute subdural hematoma: case report. J Neurosurg. 2008; 108:1018–1020.

6. Sacho RH, Kogels M, du Plessis D, Jowitt S, Josan VA. Primary diffuse large B-cell central nervous system lymphoma presenting as an acute space-occupying subdural mass. J Neurosurg. 2010; 113:384–387.

7. Martin J, Ramesh A, Kamaludeen M, Udhaya , Ganesh K, Martin JJ. Primary non-Hodgkin's lymphoma of the scalp and cranial vault. Case Rep Neurol Med. 2012; 2012:616813.

8. Yeung CY, Hong KT, Chiang CP, Chen YH, Ma HI, Tsai TH. Anaplastic lymphoma kinase-negative anaplastic large cell lymphoma manifesting as a scalp hematoma after an acute head injury-a case report and literature review. World Neurosurg. 2016; 88:688.e13–688.e16.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download