Abstract
This report presents a case of fourth ventricle neurenteric cyst (NE cyst) mimicking hemangioblastoma, which developed in a 50-year-old woman. A tiny enhancing mural portion of the fourth ventricle in MRI suggested that the cyst was hemangioblastoma, but pathological evidence showed that the cyst was in fact NE cyst in the fourth ventricle. In order to make proper decision on to what extent of surgical resection should be done, considering every possibility in differential diagnosis might be helpful. This case reports an unusual pathology in 4th ventricle, considering the patient's age, and demonstrates that a rarer disease may share radiological features of a common disease.
Neurenteric cyst (NE cyst) is an intracranial benign cystic lesion composed of epithelial lining of endodermal origin [1]. Though its exact etiology is still uncertain, it is widely believed to originate from incomplete dissolution of the neurenteric canal in embryonic stage. Because of the endodermal origin of the cyst, NE cyst is most frequently found in the spinal cord, which is close to respiratory organs [2].
Among all reported cases of NE cysts, as much as 78% of them are found in the posterior fossa or craniocervical junction area [2345]. These locations are, compared to other parts of the brain, nearer to the torso; this explains why an overwhelming majority of the reported intracranial NE cysts are found here. On the other hand, fourth ventricle is where only rarely the cyst is expected to be found [345].
A 50-year-old woman who was previously healthy presented with headache. She described her headache as dull pain on whole head and it started 3 months earlier. At beginning, the pain was mild and intermittent, but it was getting worse and worse. Moreover, on admission day, she had nausea and dizziness.
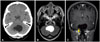
She had no definite neurological deficit on admission, and there was no abnormality on cerebellar function test. Her brain CT scan showed a 4.1×3.3 cm-sized, hypo-dense cystic lesion at the fourth ventricle and the cerebellum (Fig. 1A), and the magnetic resonance (MR) imaging scan also showed a cystic lesion with the same size as that of the CT scan in the cerebellar inferior vermis. The signal intensity of the cyst in the MR image was the same as that of cerebrospinal fluid (CSF). The T2 MR image confirms that the cyst content might be similar to CSF (Fig. 1B). Suspicious tiny enhancing mural portion at right inferior cystic wall was visible in enhanced coronal T1 MR image (Fig. 1C), which seemed to be an enhancing nodule of hemangioblastoma, although transfemoral cerebral angiography did not show any definitive vascular abnormality or staining. Hyperintense cyst on T2-weighted MR, enhancing mural portion and the cyst location of posterior fossa suggest that the lesion might be hemangioblastoma with small nodule. Because NE cyst and other intracranial cystic lesions lack specific imaging features.
Clinical diagnosis based on radiological evidence listed above was cystic hemangioblastoma with small nodule.
Midline sub-occipital craniotomy was performed, and the cyst was removed completely. The cyst was filled with CSF-like fluid, and was covering cerebellar vermis inferior of the hemisphere. The cyst wall was gray to pinkish in color, and slightly thick with some vascularity. No mural nodule was found, and almost all visible cyst walls including the portion adjacent to brainstem were removed. The intraoperative neuromonitoring was performed during surgery, and there was no change in motor evoked potentials and somatosensory evoked potentials.
The patient fully recovered and did not show any neurological deficit. No evidence of recurrence was detected for three years after operation.
The cyst specimen contained cuboidal epithelial cells (Fig. 2A). As shown in Fig. 2B, the epithelium was stained positive for CK7, and was stained negative for CK20. Microscopic feature of hemangioblastoma is vacuolated stromal cells with negative for cytokeratin. So, considering histology with the immunohistochemistry results, the cyst was diagnosed as NE cyst of respiratory origin.
The patient in this report had a cystic lesion with a tiny enhancing mural portion in the fourth ventricle. Intracranial cysts with an enhanced mural nodule are well-known radiologic features of fluid-secreting neoplasms, such as hemangioblastoma, pilocytic astrocytoma, ganglioglioma, and pleomorphic xanthoastrocytoma as the most common examples and tanycytic ependymoma, intraparenchymal schwannoma, desmoplastic infantile ganglioma, and cystic metastasis as the less common examples [67]. But, the location of the cyst prioritized hemangioblastoma and arachnoid cyst in the differential diagnosis. Because NE cyst is rarely accompanied by an enhancing mural nodule on MRI and median age of intracranial NE cyst at presentation is 34 years (range 0–78 years), we didn't expect it [2589101112]. However, contrary to what was expected, operative findings and pathological examination as described above confirmed that the cyst was actually NE cyst.
Hemangioblastoma, arachnoid cyst, and NE cyst are usually stable with slow growth patterns, so expectant management without surgery may occasionally be considered if lesion is stable and nonsymptomatic [6]. But, if it needs surgical resection, appropriate surgical intervention for each disease varies greatly. While only the mural nodule should be surgically removed in hemangioblastoma, intracranial NE cyst might require the whole cyst to be removed by surgery. Therefore, in order to make proper decision on to what extent of surgical resection should be done, every possibility should be considered in the differential diagnosis [213].
Granted, fourth ventricle is not a place where intracranial NE cyst is expected to be found frequently [345]. From 1952 to 2011, 140 cases of histologically confirmed intracranial NE cysts have been reported: among the 140 intracranial NE cysts, two most frequently found locations were the posterior fossa (47 cases), especially cerebellopontine angle and the craniocervical junctional area (61 cases), while only two of them were found in the fourth ventricle [1312]. Nevertheless, two among 140 is not a portion that is small enough to be readily dismissed.
NE cyst in fourth ventricle is rare, and its radiological appearance may mislead to similar intracranial lesions that are difficult to distinguish and require different treatment. Therefore, though uncommon, we suggest we should not exclude intracranial NE cyst from differential diagnosis when a cystic structure filled with CSF-like fluid is found in the fourth ventricle.
Figures and Tables
Fig. 1
Preoperative images of patient. A: Transverse CT image of the patient's head. A cystic lesion is clearly visible at the fourth ventricle and the cerebellum. B: Axial T2 MR image of the patient's head. The white color of the cystic region shown in this image suggests that the cyst is filled with CSF-like fluid. C: Coronal T1 MR image shows a suspicious tiny enhancing mural portion at right inferior cystic wall (pointed by the arrow). CSF, cerebrospinal fluid.
References
1. Okabe S, Kamata K, Kohno T, Harada Y. Enterogenous cyst in the fourth ventricle--case report. Neurol Med Chir (Tokyo). 1995; 35:40–44.
2. Wang L, Zhang J, Wu Z, et al. Diagnosis and management of adult intracranial neurenteric cysts. Neurosurgery. 2011; 68:44–52. discussion 52.

3. Afshar F, Scholtz CL. Enterogenous cyst of the fourth ventricle: case report. J Neurosurg. 1981; 54:836–838.
4. Sharma RR, Ravi RR, Gurusinghe NT, et al. Cranio-spinal enterogenous cysts: clinico-radiological analysis in a series of ten cases. J Clin Neurosci. 2001; 8:133–139.

5. Perrini P, Rutherford SA, King AT, du Plessis D, Di Lorenzo N. Enterogenous cysts of the cerebellopontine angle: short review illustrated by two new patients. Acta Neurochir (Wien). 2008; 150:177–184. discussion 184.

6. Yamamoto J, Shimajiri S, Akiba D, Nakano Y, Nishizawa S. Intracranial neurenteric cyst with an enhanced mural nodule and melanin pigmentation: radiologic-pathologic correlation. World Neurosurg. 2017; 97:758.e11–758.e19.

7. Raz E, Zagzag D, Saba L, et al. Cyst with a mural nodule tumor of the brain. Cancer Imaging. 2012; 12:237–244.

8. Cho JM, Ahn JY, Kim SH, Lee KS, Chang JH. An endodermal cyst mimicking an intra-axial tumor in the medulla oblongata. Childs Nerv Syst. 2010; 26:853–856.

9. Ko BS, Jung S, Jung TY, Moon KS, Kim IY, Kang SS. Neurenteric cyst with xanthomatous changes in the prepontine area: unusual radiological findings. J Neurosurg Pediatr. 2008; 2:351–354.

10. Roder C, Ebner FH, Schuhmann MU. Neurenteric cysts of the cerebellopontine angle. J Neurol Surg A Cent Eur Neurosurg. 2013; 74:Suppl 1. e36–e40.

11. Shin JH, Byun BJ, Kim DW, Choi DL. Neurenteric cyst in the cerebellopontine angle with xanthogranulomatous changes: serial MR findings with pathologic correlation. AJNR Am J Neuroradiol. 2002; 23:663–665.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download