Abstract
Toxoplasmic encephalitis (TE) is an opportunistic infection found in immunocompromised patients and TE related cerebral mass lesion is often reported in acquired immunodeficiency acquired immunodeficiency syndrome (AIDS) patients. However, incidence of TE related AIDS in Korea is still rare and is unfamiliar to neurosurgeons. Differential diagnosis is needed to rule out other brain lesions. A 39-year-old man visited the emergency room with rapid progressive left hemiparesis. Magnetic resonance imaging showed a ring-enhanced mass lesion in his right frontal lobe. Human immunodeficiency virus and Toxoplasma gondii immunoglobulin G were tested positive by a serologic test. We report here a rare case of patient with TE related AIDS.
Toxoplasmic encephalitis (TE) is an opportunistic infection that progresses rapidly and threatens the patient's life. It usually affects the central nervous system (CNS) of immunocompromised patients or organ transplant recipients by reactivating latent Toxoplasma gondii (T. gondii) [12]. In South Korea, the human immunodeficiency virus (HIV) epidemic has continued unabated since 1985 with 700–800 new infections every year [3].
In Korea, data on clinical cases of TE are limited because of the small number of AIDS patients and the difficulty in making a definitive diagnosis for TE. TE can be diagnosed by serologic examination, but the diagnosis should be confirmed using other techniques. Direct detection of the pathogen in the cerebrospinal fluid using polymerase chain reaction has high specificity, but is insufficient for a definitive diagnosis because of low sensitivity [4]. Additionally, there are no typical findings on neuroimaging modalities including computed tomography scan and MRI.
We report here our experience with TE in an AIDS patient and discuss the importance of early diagnosis and treatment.
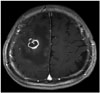
A 39-year-old man with rapid progressive left hemiparesis from motor grade III to IV was admitted to our hospital in January 2014. His mental status was alert and there were no other neurological deficits besides hemiparesis. To evaluate the left hemiparesis and to exclude the possibility of acute cerebrovascular accident, brain MRI with diffusion tense imaging was performed. Contrast enhanced T1-weighted MRI of the brain showed a low intensity lesion with ring enhancement at the right frontal lobe and low intensity around the lesion (Fig. 1). In serological tests, HIV antibody and T. gondii immunoglobulin (Ig)G antibody were tested positive, but T. gondii IgM antibodies were not detected. The concentration of HIV RNA in plasma was 209,898 copies/mL and the CD4 cell concentrate was 1.9% (reference, 38–46%). He had no prior history of keeping a cat nor being a homosexual. Based on the test results, diagnosis of TE related AIDS was made. We immediately began medical therapy for toxoplasmosis, by including sulfadiazine and pyrimethamine drugs in conjunction with AIDS medication (combivir tablet and kaletra tablet).
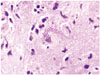
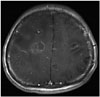
We performed brain biopsy to confirm the pathologic finding of TE using a 3D navigation system. After surgery, a neuropathological study showed many bradyzoites fill a ruptured protozoal pseudocyst suggesting TE (Fig. 2). Ten days subsequent to operation, his mental status changed drowsy and a follow up MRI of the brain was performed. The brain MRI showed multiple high signal lesions on T2-weighted image and the corresponding T1-weighted image showed low signal lesions. In addition, contrast enhanced T1-weighted image showed multiple ring enhancement lesions (Fig. 3). His mental status deteriorated rapidly into coma and he expired after 26 days of treatment.
According to the United Nations Program on HIV/AIDS, the estimated number of people living with HIV/AIDS worldwide is 35.3 million as of 2012 [5]. Since the first reported case of AIDS in 1985, the number of HIV infected people has increased sharply in Korea [6]. According to 2014 data, a total of 431 individuals had progressed to AIDS and 998 were HIV positive. T. gondii is an intracellular protozoan parasite and can infect a human as a definitive host. Humans can be infected in three ways: by ingesting undercooked meat (such as lamb and pork), that contains T. gondii tissue cysts, by ingesting oocysts (containing sporozoites) in contaminated water and through via transplacental (vertical) transmission [7]. Toxoplasmosis is the leading cause of CNS lesions in AIDS patients and the development of life-threatening TE [89]. TE is an opportunistic infection found in at least 5% of patients with AIDS and the incidence may be as high as 40% [101112]. The clinical manifestations of TE patients are focal neurologic deficits and signs. These clinical symptoms often show as subacute onset in 58–89% of patients. However, in 15–25% of patients, the symptoms appear suddenly with seizure and hemorrhage. Mild hemipharesis and/or speech abnormality are the most common initial focal findings. Headache, mental changes, lethargy, brain stem, and cerebellar disorders have also been reported [1314]. These findings are indistinguishable from the findings of other brain lesions. Chorea is believed to be one of the pathognomic findings in TE, but the occurrence is rare.
In the present case, the patient visited the hospital because of left side hemipharesis and was determined to be immunocompromised (positive for HIV antigen). MR imaging findings revealed a ring enhancement mass lesion associated with severe edema. It is difficult to make a diagnosis of TE with only MR. Since the MR findings of TE are very similar to other brain lesions such as brain abscess, metastatic tumor, and CNS lymphoma, differential diagnosis of TE is necessary [15]. TE is generally diagnosed using a toxoplasma antibody titer, but negative serum anti-toxoplasma antibody response has been observed in about 10% of patients with TE related AIDS. Therefore, TE cannot be ruled out in AIDS patients even if serum anti-toxoplasma antibody test is negative [16]. In the case of our patient, T. gondii IgG antibody was positive in the serologic test, but T. gondii IgM antibody was negative. This means that our patient was not in the acute stage of initial infection but had been infected for a long time.
Unfortunately, the patient expired within 10 days after the brain biopsy. TE is a disease characterized by rapid progression. Therefore, if TE related AIDS is suspected, medical treatment should be initiated immediately, and simultaneous surgical evacuation must be considered when the mass is large enough to compress the brain.
A large number of studies on understanding the relationship between AIDS and TE have been reported in radiology, parasitology, neurology, and immunology journals. However, only a few cases of TE related AIDS have been reported in neurosurgical fields. In the past, the number of AIDS patients in Korea was small, but this population has increased gradually. Furthermore, the inflow of immigrants is likely to affect the incidence of AIDS and it is conjectured that TE will eventually become the most common brain lesion in AIDS patients. Therefore, neurosurgeons should always consider the possibility of TE in immunocompromised patients with ring enhanced lesions in brain MRI. Medical treatment should be the first step and surgical evacuation should be considered if patients do not respond to medical treatment or show a rapid neurological deterioration, because misdiagnosis and delayed treatment could be life threatening.
In conclusion, we report a rare case of a TE patient with AIDS in Korea. The number of AIDS patients has been constantly increasing in Korea. Accordingly, TE related AIDS would become the most common cerebral mass lesion in AIDS patients. If TE is suspected in immunocompromised patients with ring enhanced lesions on brain MRI, accurate diagnosis and medical treatment should be performed at the earliest. Additionally, differential diagnosis of ring enhanced lesions must be made because delayed treatment or misdiagnosis could be life threatening.
Figures and Tables
References
3. Korea Centers for Disease Control and Prevention. Annual report on the notified HIV/AIDS in Korea. Statistical Annual Report of HIV/AIDS. Cheongju: Korea Centers for Disease Control and Prevention;2010.
4. Cingolani A, De Luca A, Ammassari A, et al. PCR detection of Toxoplasma gondii DNA in CSF for the differential diagnosis of AIDS-related focal brain lesions. J Med Microbiol. 1996; 45:472–476.

5. The Joint United Nations Programme on HIV/AIDS. UNAIDS report on the global AIDS epidemic 2013. Geneva: The Joint United Nations Programme on HIV/AIDS;2013.
6. Korea Centers for Disease Control and Prevention. The surveillance reports for HIV/AIDS in Korea 2011. Cheongju: Korea Centers for Disease Control and Prevention;2013.
7. Carruthers VB, Suzuki Y. Effects of Toxoplasma gondii infection on the brain. Schizophr Bull. 2007; 33:745–751.

8. Israelski DM, Remington JS. Toxoplasmosis in the non-AIDS immunocompromised host. Curr Clin Top Infect Dis. 1993; 13:322–356.
9. Wong SY, Remington JS. Toxoplasmosis in the setting of AIDS. In : Broder S, Merigan TC, Bolognesi D, editors. Textbook of AIDS medicine. Baltimore: Williams and Wilkins;1994. p. 223–257.
10. Agrawal D, Hussain N. Decompressive craniectomy in cerebral toxoplasmosis. Eur J Clin Microbiol Infect Dis. 2005; 24:772–773.

11. Rosenthal D, LeBoit PE, Klumpp L, Berger TG. Human immunodeficiency virus-associated eosinophilic folliculitis. A unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991; 127:206–209.

12. Rossitch E Jr, Carrazana EJ, Samuels MA. Cerebral toxoplasmosis in patients with AIDS. Am Fam Physician. 1990; 41:867–873.
13. Navia BA, Petito CK, Gold JW, Cho ES, Jordan BD, Price RW. Cerebral toxoplasmosis complicating the acquired immune deficiency syndrome: clinical and neuropathological findings in 27 patients. Ann Neurol. 1986; 19:224–238.

14. Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992; 327:1643–1648.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download