Abstract
Central neurocytoma (CN) typically presents as an intraventricular mass causing obstructive hydrocephalus. The first line of treatment is surgical resection with adjuvant conventional radiotherapy. Stereotactic radiosurgery (SRS) was proposed as an alternative therapy for CN because of its lower risk profile. The objective of this systematic analysis is to assess the efficacy of SRS for CN. A systematic analysis for CN treated with SRS was conducted in PubMed. Baseline patient characteristics and outcomes data were extracted. Heterogeneity and publication bias were also assessed. Univariate and multivariate linear regressions were used to test for correlations to the primary outcome: local control (LC). The estimated cumulative rate of LC was 92.2% (95% confidence interval: 86.5-95.7%, p<0.001). Mean follow-up time was 62.4 months (range 3-149 months). Heterogeneity and publication bias were insignificant. The univariate linear regression models for both mean tumor volume and mean dose were significantly correlated with improved LC (p<0.001). Our data suggests that SRS may be an effective and safe therapy for CN. However, the rarity of CN still limits the efficacy of a quantitative analysis. Future multi-institutional, randomized trials of CN patients should be considered to further elucidate this therapy.
Central neurocytoma (CN) is an extremely rare neuroepithelial tumor that accounts for 0.1–0.5% of all adult primary brain tumors [12345]. CN is classified by the World Health Organization as a grade II (benign) neoplasm [36]. By definition, CN is located in the ventricular system. As such, patients often present with headaches, nausea, or vomiting consistent with an obstructive pattern of hydrocephalus [347891011121314151617]. Computed tomography images demonstrate a heterogeneously hyperdense, enhancing mass. CN is typically isointense, iso-hyperintense and moderately hyperintense on T1-, T2-, and contrast enhanced magnetic resonance imaging, respectively[4811151718192021].
Management of CN involves surgical resection and/or adjuvant treatment consisting of radiotherapy or chemotherapy. Gross total resection (GTR) is often curative, with a 99% 5-year survival rate [41222232425]. However, due to its central location, GTR is rarely achieved (30% to 50% of cases) [2627]. Thus, subtotal resection (STR) with adjuvant treatment is often necessary [4122628]. Adjuvant therapy for CN traditionally consisted of conventional radiotherapy, but was limited by associated cognitive deficits and other neurotoxicities [22272930313233]. Recently, stereotactic radiosurgery (SRS) is increasingly utilized as an alternative modality because of fewer fractions and associated toxicities [5222731343536373839404142434445464748]. Several studies have demonstrated equivalent tumor control and fewer complications with adjuvant SRS when compared with conventional radiotherapy [1249].
A quantitative systematic review by Park and Steven [22] in 2012 (62 patients) demonstrated the efficacy of SRS for CN. The current systematic analysis updates the findings of Park and includes several additional case series published since then for a total of 150 patients [50515253]. To our knowledge, this study represents the largest and most current review of CN patients treated with SRS.
Adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (http://www.prisma-statement.org) was maintained throughout this study. The PubMed database was searched by two independent authors using terms “CN” and “radiosurgery”. Abstracts were reviewed and screened against inclusion and exclusion criteria. Inclusion criteria were: 1) original data, 2) sufficient data on SRS outcomes for treatment of CN, and 3) more than one patient. Exclusion criteria were: 1) non-English text, 2) review articles, and 3) studies from the institutions/utilizing the same patient pool already included in analysis. Our screening process is summarized in Fig. 1.
Statistical analysis was performed using Comprehensive Meta-Analysis software (version 3.0; Biostat, Englewood, NJ, USA). The Q Statistic of the χ2 value test and inconsistency index was used to estimate heterogeneity of included studies. A random-effect model was chosen to better account for heterogeneity between included studies. A funnel plot, Begg's rank correlation test, and Egger's linear regression method were used to graphically and quantitatively assess publication bias. The summary of local control (LC) rate and 95% confidence interval (CI) were calculated from reported pooled data. Sensitivity analysis was done to see if any individual study significantly affected our results.
Additional univariate and multivariate analyses were completed using the Statistical Analysis System (SAS, version 9.3; SAS Institute Inc., Cary, NC, USA). Linear regression of the overall data was used to test if various predictive variables were correlated with patient outcomes. Independent variables analyzed included mean tumor volume and dose. Data collated from individual articles was also analyzed using N-1 Pearson chi-squared tests to compare proportions [5455]. Statistical significance was set at a p-value less than 0.05.
A total of 10 studies (all case series) comprising 150 patients were included in our quantitative synthesis. These patients were treated with either Gamma Knife radiosurgery (GKRS; n=146, 97%) or linear accelerator radiosurgery (n=4, 3%) (Table 1). Resection (STR or GTR) was previously performed in 125 patients (83.3%), while 25 patients (16.7%) were treated with primary SRS. Mean marginal dose was 14.7 Gy (range 9–25 Gy). Mean tumor volume was 9.3 mL (range 0.4–36.4 mL). Complications included intracerebral (tumoral) hemorrhage (n=3), cerebral edema (n=3), and radiation injury (n=2). Overall survival was 98% at a mean follow-up of 62.4 months (range 3–149 months).
Test of heterogeneity was non-significant (p=0.98). The Q-value was 2.53 (df=9) and I2=0. Publication bias was assessed graphically via funnel plot, which displays no significant asymmetry (Fig. 2). Begg's rank correlation test and Egger's linear regression method were both insignificant, with 2-tailed p-values of 0.09 and 0.93, respectively. Fig. 3 displays the control rates of all included studies. Overall LC was 92.2% (95% CI 86.5–95.7%) (p<0.001).
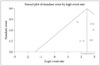
Univariate linear regression models for both mean tumor volume and mean dose were significantly correlated with improved LC. Smaller tumor volumes were associated with better overall LC (p<0.001). Likewise, greater radiation doses correlated with better overall LC (p<0.001).
The optimal management of CN remains controversial [56]. Schild et al. [12] first reported the use of SRS for CN in 1997. Since then, multiple case series and systematic reviews have reaffirmed its efficacy [522273134353637383940414243444546474849]. The aforementioned study by Park and Steven [22] represents the first quantitative systematic review of SRS for treatment of CN. That study analyzed 5 retrospective case series (64 CNs in 62 patients). Of the 62 patients, only 4 displayed tumor growth after undergoing SRS (6.3%). We have analyzed 10 retrospective case series with a total of 150 patients, making this the largest review to date. Park and Steven [22] initially reported a LC rate of 91.1% with 2 local failures at a mean follow-up of 59.3 months. The expanded patient pool used in our study allowed us to calculate a similar LC rate (92.2%) reflecting 9 local failures at a mean follow-up of 62.4 months. Our data supports the conclusion that SRS is a viable treatment for CN.
The two LC failures in Park and Steven's [22] initial review were associated with unknown etiology and inadequate dosing. In our analysis, individual data was available for 4 of the 9 LC failures. Mean marginal dose for local recurrences was 12.8 Gy compared to 15.6 Gy in 62 reported patients achieving tumor control. In addition, we found that mean dose was significantly correlated with LC. Despite the small sample size, this provides evidence that radiation dose could contribute to LC. Matsunaga et al. [5] reported improved LC with relatively low marginal doses of 13 to 18 Gy and therefore recommend a marginal dose of at least 13 Gy for effective tumor control. Our findings corroborate the recommendation of Matsunaga et al. [5] to maintain a dose high enough to achieve tumor control but not so high as to cause toxicity. This is largely consistent with the studies we reviewed, which have an overall mean dose of 14.7 Gy (range 10.5–17.0 Gy) (Table 1).
MIB-1 (Ki-67) labeling index has been demonstrated to be the most important marker of potentially malignant behavior in CN [4565758596061626364]. CN is considered atypical if the MIB-1 (Ki-67) labeling index is greater than or equal to 2% [45758]. Interestingly, Genc et al. [56] reported that MIB-1 (Ki-67) indices had no significant effect on tumor response to SRS. However, the authors acknowledge that interpretation of their findings may be limited by a short follow-up duration (mean 36 months), particularly of atypical CNs. Data on MIB-1 (Ki-67) labeling index was not available for most studies, which prevented further analyses with regard to index and LC.
SRS has been demonstrated to be effective in primary management of CN, particularly in cases less amenable to surgical resection [293150]. In our study, 25 patients (16.7%) were treated with GKRS alone. Individual patient data was available for 18 patients. We found similar LC between primary SRS and our overall cohort (88.9% vs. 92.2%, p=0.63). Kim et al. [29] report a 20% LC failure rate for patients treated with primary SRS vs. 40% LC failure in patients treated with adjuvant SRS. Similarly, Karlsson et al. [50] found primary SRS to be efficacious in control of incidental, asymptomatic CN. The report of effective primary control is consistent with our findings that mean tumor volume is directly correlated with LC failure, since smaller tumor volumes are less likely to need surgical decompression or be symptomatic. Moreover, our data suggests that smaller tumor volume is significantly correlated with better LC.
Radiation associated adverse events (AREs), defined as hyperintensity surrounding the treated lesion on imaging, are rare after SRS for CN (Table 1) [52]. There are only 3 reported AREs (all cases of cerebral edema) in the literature with only one becoming symptomatic (Table 1) [294150]. Only 2% of the patients reviewed experienced AREs. Interestingly, Karlsson et al. [50] also reported that 45% (19/42) of their patients developed ventricular enlargement with 33% (1/3) requiring surgical management. This has not been reported elsewhere in the literature. Long term outcomes and toxicities of SRS for CN are not known. There have been two reported cases of increased MIB-1 (Ki-67) index, angiogenesis and glial differentiation in recurrent tumor that may have been attributable to SRS [565]. Given the low complication rate and favorable tumor control, current dosages reported are considered both safe and effective, respectively.
Limitations to this study were ever-present despite an increase in sample size (>two-fold) as compared to the prior quantitative systematic review. The rarity of CN makes available data sporadic, consisting of only case series. Mean follow-up for the included studies is another limitation, as a limited window can blind our results to potential failures occurring after end-of-study (Table 1).
Our data suggests that SRS may be an effective and safe therapy for CN. The rarity of CN limits the efficacy of a quantitative analysis. Future prospective, randomized studies with extended follow-up should be conducted to elucidate long-term efficacy of SRS in treatment of typical and atypical CN.
Figures and Tables
Table 1
Literature review of SRS for central neurocytoma
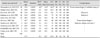
| Author and year [ref] | n | Mean age | Modality | MTV (mL) | Mean dose (Gy) | F/U (mos) | RR (%) | LC (%) | DC (%) | OS (%) | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Yamanaka et al., 2016 [53] | 36 | 35.0 | GKRS | 4.9* | 15.0* | 54.5* | 88 | 94 | 92 | 97 | Tumor hemorrhage×2, radiation injury×1 |
| Monaco et al., 2015 [52] | 8 | 29.0 | GKRS | 5.5 | 14.6 | 63.3 | 88 | 100 | 88 | 100 | – |
| Kim et al., 2013 [29] | 20 | 32.0 | GKRS | 11.0 | 15.4 | 103 | 70 | 85 | 85 | 100 | Edema×1 |
| Karlsson et al., 2012 [50] | 42 | 32.0 | GKRS | 12.0 | 13.0 | 73 | 91 | 95 | 95 | 100 | Edema×1 |
| Genc et al., 2011 [56] | 22 | 30.2 | GKRS | 13.4 | 16.4 | 36 | 95 | 95 | 100 | 100 | – |
| Yen et al., 2007 [46] | 7 | 26.7 | GKRS | 6.0 | 16.0 | 60 | 100 | 100 | 100 | 86 | Tumor hemorrhage×1 |
| Martín et al., 2003 [41] | 4 | 26.3 | LINAC | 3.2 | 16.5 | 33 | 100 | 100 | 100 | 100 | Alopecia, edema, necrosis×1 |
| Anderson et al., 2001 [27] | 4 | 28.3 | GKRS | 7.0 | 17.0 | 17 | 100 | 100 | 100 | 100 | – |
| Bertalanffy et al., 2001 [34] | 3 | 22.3 | GKRS | 3.9 | 12.8 | 60 | 100 | 100 | 100 | 67 | – |
| Cobery et al., 2001 [35] | 4 | 27.5 | GKRS | 14.8 | 10.5 | 44 | 100 | 100 | 100 | 100 | – |
| Total | 150 | ||||||||||
| Mean | 31.5 | 9.3 | 14.7 | 62.4 | 89 | 94 | 94 | 98 |
Acknowledgments
The authors thank Jason Sheehan, MD, PhD, University of Virginia School of Medicine, Michael B. Sisti, MD, FACS, Columbia University Medical Center, Richard C.E. Anderson, MD, FACS, FAAP, Columbia University Medical Center, Tony J.C. Wang, Columbia University Medical Center, Dong Gyu Kim, MD, PhD, Seoul National University College of Medicine, and Jin Wook Kim, MD, Seoul National University College of Medicine, for sharing their data.
References
1. Hassoun J, Gambarelli D, Grisoli F, et al. Central neurocytoma. An electron-microscopic study of two cases. Acta Neuropathol. 1982; 56:151–156.
2. Sharma MC, Deb P, Sharma S, Sarkar C. Neurocytoma: a comprehensive review. Neurosurg Rev. 2006; 29:270–285. discussion 285.

3. Yang I, Ung N, Chung LK, et al. Clinical manifestations of central neurocytoma. Neurosurg Clin N Am. 2015; 26:5–10.

4. Choudhari KA, Kaliaperumal C, Jain A, et al. Central neurocytoma: a multi-disciplinary review. Br J Neurosurg. 2009; 23:585–595.

5. Matsunaga S, Shuto T, Suenaga J, Inomori S, Fujino H. Gamma knife radiosurgery for central neurocytomas. Neurol Med Chir (Tokyo). 2010; 50:107–112. disucussion 112-3.

6. Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109.

7. Sharma MC, Sarkar C, Karak AK, Gaikwad S, Mahapatra AK, Mehta VS. Intraventricular neurocytoma: a clinicopathological study of 20 cases with review of the literature. J Clin Neurosci. 1999; 6:319–323.

8. Jaiswal S, Vij M, Rajput D, et al. A clinicopathological, immunohistochemical and neuroradiological study of eight patients with central neurocytoma. J Clin Neurosci. 2011; 18:334–339.

9. De Tommasi A, D'Urso PI, De Tommasi C, Sanguedolce F, Cimmino A, Ciappetta P. Central neurocytoma: two case reports and review of the literature. Neurosurg Rev. 2006; 29:339–347.

10. Ashkan K, Casey AT, D'Arrigo C, Harkness WF, Thomas DG. Benign central neurocytoma. Cancer. 2000; 89:1111–1120.

11. Chandrashekhar TN, Mahadevan A, Vani S, et al. Pathological spectrum of neuronal/glioneuronal tumors from a tertiary referral neurological institute. Neuropathology. 2012; 32:1–12.

13. Agranovich AL, Ang LC, Fryer CJ. Central neurocytoma: report of 2 cases and literature review. J Neurooncol. 1993; 16:47–53.

14. Brat DJ, Scheithauer BW, Eberhart CG, Burger PC. Extraventricular neurocytomas: pathologic features and clinical outcome. Am J Surg Pathol. 2001; 25:1252–1260.
15. Hassoun J, Söylemezoglu F, Gambarelli D, Figarella-Branger D, von Ammon K, Kleihues P. Central neurocytoma: a synopsis of clinical and histological features. Brain Pathol. 1993; 3:297–306.

16. Moussa R, Abadjian G, Nader M, et al. [Central neurocytoma. Four patients]. Neurochirurgie. 2004; 50:639–646.
17. Shin JH, Lee HK, Khang SK, et al. Neuronal tumors of the central nervous system: radiologic findings and pathologic correlation. Radiographics. 2002; 22:1177–1189.

19. Goergen SK, Gonzales MF, McLean CA. Interventricular neurocytoma: radiologic features and review of the literature. Radiology. 1992; 182:787–792.

20. Schmidt MH, Gottfried ON, von Koch CS, Chang SM, McDermott MW. Central neurocytoma: a review. J Neurooncol. 2004; 66:377–384.

22. Park HK, Steven DC. Stereotactic radiosurgery for central neurocytoma: a quantitative systematic review. J Neurooncol. 2012; 108:115–121.

24. Paek SH, Kim DG, Kim IH, et al. O-22-327-Central neurocytoma: the role of radiation therapy and long-term outcome. Clin Neurol Neurosurg. 1997; 99:Supplement 1. S192.
25. Bertalanffy A, Roessler K, Koperek O, Gelpi E, Prayer D, Knosp E. Recurrent central neurocytomas. Cancer. 2005; 104:135–142.

26. Kim DG, Paek SH, Kim IH, et al. Central neurocytoma: the role of radiation therapy and long term outcome. Cancer. 1997; 79:1995–2002.
27. Anderson RC, Elder JB, Parsa AT, Issacson SR, Sisti MB. Radiosurgery for the treatment of recurrent central neurocytomas. Neurosurgery. 2001; 48:1231–1237. discussion 1237-8.

28. Leenstra JL, Rodriguez FJ, Frechette CM, et al. Central neurocytoma: management recommendations based on a 35-year experience. Int J Radiat Oncol Biol Phys. 2007; 67:1145–1154.

29. Kim JW, Kim DG, Chung HT, et al. Radiosurgery for central neurocytoma: long-term outcome and failure pattern. J Neurooncol. 2013; 115:505–511.

30. Chen YD, Li WB, Feng J, Qiu XG. Long-term outcomes of adjuvant radiotherapy after surgical resection of central neurocytoma. Radiat Oncol. 2014; 9:242.

31. Chen MC, Pan DH, Chung WY, et al. Gamma knife radiosurgery for central neurocytoma: retrospective analysis of fourteen cases with a median follow-up period of sixty-five months. Stereotact Funct Neurosurg. 2011; 89:185–193.

32. Maiuri F, Spaziante R, De Caro ML, Cappabianca P, Giamundo A, Iaconetta G. Central neurocytoma: clinico-pathological study of 5 cases and review of the literature. Clin Neurol Neurosurg. 1995; 97:219–228.

33. Paek SH, Han JH, Kim JW, et al. Long-term outcome of conventional radiation therapy for central neurocytoma. J Neurooncol. 2008; 90:25–30.

34. Bertalanffy A, Roessler K, Dietrich W, et al. Gamma knife radiosurgery of recurrent central neurocytomas: a preliminary report. J Neurol Neurosurg Psychiatry. 2001; 70:489–493.

35. Cobery ST, Noren G, Friehs GM, et al. Gamma knife surgery for treatment of central neurocytomas. Report of four cases. J Neurosurg. 2001; 94:327–330.
36. Pollock BE, Stafford SL. Stereotactic radiosurgery for recurrent central neurocytoma: case report. Neurosurgery. 2001; 48:441–443.

37. Tyler-Kabara E, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for residual neurocytoma. Report of four cases. J Neurosurg. 2001; 95:879–882.
38. Hara M, Aoyagi M, Yamamoto M, et al. Rapid shrinkage of remnant central neurocytoma after gamma knife radiosurgery: a case report. J Neurooncol. 2003; 62:269–273.
39. Javedan SP, Manwaring K, Smith KA. Treatment of posterior third ventricular central neurocytoma with endoscopic biopsy, endoscopic third ventriculostomy and stereotactic radiosurgery. Minim Invasive Neurosurg. 2003; 46:165–168.

40. Kim CY, Paek SH, Kim DG. Linear accelerator radiosurgery for central neurocytoma: a case report. J Neurooncol. 2003; 61:249–254.
41. Martín JM, Katati M, López E, et al. Linear accelerator radiosurgery in treatment of central neurocytomas. Acta Neurochir (Wien). 2003; 145:749–754. discussion 754.

42. Suh JH, Barnett GH. Stereotactic radiosurgery for brain tumors in pediatric patients. Technol Cancer Res Treat. 2003; 2:141–146.

43. Knisely JP, Linskey ME. Less common indications for stereotactic radiosurgery or fractionated radiotherapy for patients with benign brain tumors. Neurosurg Clin N Am. 2006; 17:149–167. vii

44. Rades D, Schild SE. Value of postoperative stereotactic radiosurgery and conventional radiotherapy for incompletely resected typical neurocytomas. Cancer. 2006; 106:1140–1143.

45. Kim CY, Paek SH, Jeong SS, et al. Gamma knife radiosurgery for central neurocytoma: primary and secondary treatment. Cancer. 2007; 110:2276–2284.
46. Yen CP, Sheehan J, Patterson G, Steiner L. Gamma knife surgery for neurocytoma. J Neurosurg. 2007; 107:7–12.

47. González SV, Rozos AP, Farpón RC, Barceló AR, Fardoun HF, Sánchez MVV. Recidivant central neurocytoma treated with radiosurgery: a case report. J Radiother Pract. 2012; 11:120–126.

48. Barnett GH, Linskey ME, Adler JR, et al. Stereotactic radiosurgery--an organized neurosurgery-sanctioned definition. J Neurosurg. 2007; 106:1–5.

49. Patel DM, Schmidt RF, Liu JK. Update on the diagnosis, pathogenesis, and treatment strategies for central neurocytoma. J Clin Neurosci. 2013; 20:1193–1199.

50. Karlsson B, Guo WY, Kejia T, et al. Gamma knife surgery for central neurocytomas. J Neurosurg. 2012; 117 Suppl:96–101.

51. Kim JW, Kim WC, Cho JH, et al. A multimodal approach including craniospinal irradiation improves the treatment outcome of high-risk intracranial nongerminomatous germ cell tumors. Int J Radiat Oncol Biol Phys. 2012; 84:625–631.

52. Monaco EA 3rd, Niranjan A, Lunsford LD. The management of central neurocytoma: radiosurgery. Neurosurg Clin N Am. 2015; 26:37–44.
53. Yamanaka K, Iwai Y, Shuto T, et al. Treatment results of gamma knife radiosurgery for central neurocytoma: report of a Japanese multi-institutional cooperative study. World Neurosurg. 2016; 90:300–305.

54. Campbell I. Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat Med. 2007; 26:3661–3675.

55. Richardson JT. The analysis of 2×2 contingency tables--yet again. Stat Med. 2011; 30:890. author reply 891-2.
56. Genc A, Bozkurt SU, Karabagli P, et al. Gamma knife radiosurgery for cranial neurocytomas. J Neurooncol. 2011; 105:647–657.

57. Sharma MC, Rathore A, Karak AK, Sarkar C. A study of proliferative markers in central neurocytoma. Pathology. 1998; 30:355–359.

58. Söylemezoglu F, Scheithauer BW, Esteve J, Kleihues P. Atypical central neurocytoma. J Neuropathol Exp Neurol. 1997; 56:551–556.

59. Mackenzie IR. Central neurocytoma: histologic atypia, proliferation potential, and clinical outcome. Cancer. 1999; 85:1606–1610.
60. Chen CL, Shen CC, Wang J, Lu CH, Lee HT. Central neurocytoma: a clinical, radiological and pathological study of nine cases. Clin Neurol Neurosurg. 2008; 110:129–136.

61. Vajrala G, Jain PK, Surana S, Madigubba S, Immaneni SR, Panigrahi MK. Atypical neurocytoma: dilemma in diagnosis and management. Surg Neurol Int. 2014; 5:183.

62. Cook DJ, Christie SD, Macaulay RJ, Rheaume DE, Holness RO. Fourth ventricular neurocytoma: case report and review of the literature. Can J Neurol Sci. 2004; 31:558–564.

63. Eng DY, DeMonte F, Ginsberg L, Fuller GN, Jaeckle K. Craniospinal dissemination of central neurocytoma. Report of two cases. J Neurosurg. 1997; 86:547–552.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download