Abstract
Extra ventricular neurocytoma (EVN) is a rare brain tumor with histologic features similar with a central neurocytoma, but located outside of the ventricular system. In this study, we present an unusual case of hypothalamic EVN in a 14-year-old patient. The patient underwent subtotal removal and had tumor relapse. The patient was then treated using intensity modulated radiation therapy, and the tumor remained stable for 24 months. This case report may be important in that this is the first pediatric case of EVN located in the hypothalamic region. EVN has similar radiologic features with pilocytic astrocytomas and therefore a hypothalamic EVN may be misdiagnosed as a hypothalamic glioma. Also, the pathologic-radiologic-clinical correlation of EVN located in the hypothalamic area may be different from that of EVNs originating from other usual sites.
Central neurocytoma (CN) is an uncommon benign neuronal tumor of the central nervous system (CNS) that is located in the ventricular system. Nishio et al. [1] reported three cases of unusual neuronal tumors in the cerebral hemisphere and named the tumors "cerebral neurocytoma". Since the initial report, there have been several case reports of tumors with similar histological features of CNs, but the tumors were located outside of the ventricles. These so-called extraventricular neurocytomas (EVNs) were classified as a different entity in the 2007 World Health Organization classification of CNS tumors. EVNs have demonstrated more malignant biological behavior, with higher rates of atypia, and higher recurrence rates than CNs [23]. In this study, we present an unusual case of hypothalamic EVN in a pediatric patient that mimicked a hypothalamic glioma.
A 14-year-old boy presented with bitemporal hemianopsia and decreased visual acuity at a local hospital (Fig. 1). His visual acuity was decreased to 0.02/0.2 (oculus dexter/oculus sinister). The patient had no specific past medical history. The initial magnetic resonance (MR) image showed a 6.1×5.7×6.0 cm homogeneously enhanced lobulating mass in the sella and suprasellar areas (Fig. 2). The radiological diagnosis was a hypothalamic glioma. To confirm the pathologic diagnosis a stereotactic biopsy was done. Unexpectedly, the pathologic result was consistent with a neurocytoma. In order to relieve the visual defect and control the disease, the neurosurgeon at the local hospital decided to remove the tumor.
The surgery was performed by a right fronto-temporal craniotomy and subfrontal approach. In the operative field, a flattened right optic nerve was noted. During the dissection, the tumor origin was not evident, but there was no connection between the tumor and the third ventricle, indicating that this tumor did not originate from the ventricular system. The mass was hyper-vascular, and there were severe adhesions with surrounding structures including the hypothalamus, internal carotid artery, optic nerve, and optic chiasm. Due to these findings, aggressive dissection and removal of tumor was limited and subtotal removal was performed. Approximately, 60% of tumor was removed. There was remnant tumor mass in the hypothalamus and optic nerve at the midline and left side, respectively (Fig. 2).
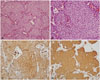
The histological findings of the tumor were identical to those of a CN (Fig. 3). The tumor was composed of homogeneous cells with clear and round cytoplasm, honeycomb appearance, and mild nuclear pleomorphism. The immunohistochemistry results were positive for synaptophysin and chromogranin. Ki-67 labeling index was less than 1%. There was no evidence of connections between the tumor and ventricles according to the radiological and surgical findings. Therefore, the pathologic diagnosis was an EVN.
The patient's visual acuity of left eye somewhat recovered to 0.7 from 0.2. The visual field defect of the right eye was not improved, and the visual acuity of the right side actually decreased to hand motion perception (Fig. 1). However, MR imaging taken at one-year follow-up after surgery revealed a 6.0×4.4 cm enhancing mass. This mass was a re-growing tumor from the sub-totally resected tumor (Fig. 2). The visual acuity was aggravated to no light perception on the right side and 0.5 on the left side. The neurosurgeon decided to perform radiotherapy with low dose radiation. He treated the patient with intensity modulated radiation therapy (IMRT) giving 200 cGy over 10 fractions to the relapsed tumor. The patient was then referred to our institution. We made a decision to continue the radiotherapy as a salvage therapy for three weeks with IMRT. The patient was treated with 30 Gy delivered in 15 fractions to the tumor. A follow-up MR was taken 24 months after the IMRT, and the results showed that the tumor was stable. The visual field has also remained unchanged according to the serial Goldmann perimetry exam (Fig. 1).
The incidence of pediatric EVN is so low that the incidence has been estimated only from a number of case reports and series. A review of pediatric EVNs in the PubMed database provided about 50 cases [345]. However, to our knowledge, there has been no case report of a pediatric EVN located in the hypothalamic region. The present case provides the first detailed radiological and clinical features of a pediatric hypothalamic EVN.
However, the importance of this case is not restricted to its rare location, but rather related to the risk of misdiagnosis, when facing a hypothalamic mass in pediatric patients. In incidence-wise aspect, primary brain tumors in the hypothalamic area comprise approximately 10% of all primary brain tumors in the pediatric population [6]. Gliomas of the optic pathway and the hypothalamus account for approximately 5% of all pediatric brain tumors, and up to 85% involve the hypothalamus [7]. In radiological terms, EVNs are often well-demarcated, partly or mainly cystic, and variably enhancing masses, with or without peritumoral edema [8]. Gliomas of the optic pathway and the hypothalamus also show similar radiologic findings [9]. In other words, EVNs may resemble pilocytic astrocytomas, gangliogliomas, or oligodendrogliomas [8]. Pediatric EVNs have been located mostly in the cerebral hemisphere, especially the frontal lobe. Unusual intracranial locations of EVNs include the thalamus, cerebellum, and spine [4]. There has been no case report of a pediatric EVN located in the hypothalamus. Thus, a pediatric neurosurgeon could misdiagnose a hypothalamic EVN as a hypothalamic glioma. Because the treatment of hypothalamic gliomas is somewhat different from that of hypothalamic EVNs, pediatric neurosurgeons should be well aware of the fact that there could be a hypothalamic EVN in pediatric patients.
Atypical EVN is defined as an EVN with atypical histologic features including increased proliferative index, microvascular proliferation, or necrosis. An atypical EVN is regarded as a more aggressive variant, so that it is helpful to predict whether the lesion is atypical or not before surgery [10]. According to a recent report, atypical histologic features seems to correlate with radiologically aggressive findings, e.g., vascular proliferative patterns and infiltrative margins [11]. This report reviewed an atypical pediatric EVN, among which there have been no hypothalamic EVNs. On contrast-enhanced MRI, the EVN of our case shows a well-demarcated homogeneously enhanced mass (Fig. 2), which did not indicate atypical pathology. In the pathologic examination, the tumor showed benign features, including Ki-67 index <1%. However, the findings during operation showed hyper-vascularity and severe adhesion with surrounding structures. Also, despite the benign pathologic and radiologic features, the tumor in our case grew somewhat rapidly after subtotal resection. Therefore, radiologic and pathologic features of EVN in the hypothalamic area may not correlate well with the clinical features, which can give important information for neurosurgeons developing a treatment plan for a pediatric hypothalamic EVN.
In conclusion, EVNs has similar radiologic features with pilocytic astrocytomas, such that hypothalamic EVNs may be misdiagnosed as a hypothalamic glioma. Also, the pathologic-radiologic-clinical correlation of EVNs located in the hypothalamic area may be different from that of EVNs originating from other usual sites.
Figures and Tables
Fig. 1
The results of the Humphrey visual field exam (A) revealed "bitemporal hemianopsia", preoperatively. The same exam (B) was performed when regrowth of the tumor was confirmed, and showed the same pattern with almost complete right eye blindness. After radiotherapy, there was no aggravation of the visual field according to the Goldmann perimetry exam (C). However, the right eye was unable to perceive light.

Fig. 2
T1-gadolinium-enhanced axial, sagittal, and coronal MR images showing the well-demarcated and homogeneously enhanced mass located in the sella-suprasella-hypothalamic area. A: Preoperative images. B: Immediate postoperative images. C: Postoperative images taken 1 year after the surgery showing regrowth of the tumor. D: The last follow up taken 24 months after intensity modulated radiation therapy.

Fig. 3
Histopathology of the lesion resected during the craniotomy. A and B: Hematoxylin and eosin staining indicates a tumor of moderate cellularity with vascular proliferation. Immunohistochemistry demonstrates neoplastic cells exhibiting strong, diffuse immunoreactivity for (C) chromogranin and (D) synaptophysin.
References
1. Nishio S, Takeshita I, Kaneko Y, Fukui M. Cerebral neurocytoma. A new subset of benign neuronal tumors of the cerebrum. Cancer. 1992; 70:529–537.

2. Sweiss FB, Lee M, Sherman JH. Extraventricular neurocytomas. Neurosurg Clin N Am. 2015; 26:99–104.

3. Xiong Z, Zhang J, Li Z, et al. A comparative study of intraventricular central neurocytomas and extraventricular neurocytomas. J Neurooncol. 2015; 121:521–529.

4. Han L, Niu H, Wang J, et al. Extraventricular neurocytoma in pediatric populations: a case report and review of the literature. Oncol Lett. 2013; 6:1397–1405.

5. Patil AS, Menon G, Easwer HV, Nair S. Extraventricular neurocytoma, a comprehensive review. Acta Neurochir (Wien). 2014; 156:349–354.

6. Schroeder JW, Vezina LG. Pediatric sellar and suprasellar lesions. Pediatr Radiol. 2011; 41:287–298. quiz 404-5.

7. Alshail E, Rutka JT, Becker LE, Hoffman HJ. Optic chiasmatic-hypothalamic glioma. Brain Pathol. 1997; 7:799–806.

8. Yang GF, Wu SY, Zhang LJ, Lu GM, Tian W, Shah K. Imaging findings of extraventricular neurocytoma: report of 3 cases and review of the literature. AJNR Am J Neuroradiol. 2009; 30:581–585.

9. Koeller KK, Rushing EJ. From the archives of the AFIP: pilocytic astrocytoma: radiologic-pathologic correlation. Radiographics. 2004; 24:1693–1708.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download