Abstract
Primary sarcomas of the central nervous system are rare. These tumors is rapid growth often produces mass effect on the brain. Diagnosis is rendered pathologically after resection. Surgical resection is the mainstay treatment and need the adjuvant therapy. We report a 44-year-old female with a meningeal sarcoma of frontal meninges. She complained headache for 2 months and palpable forehead mass for 3 weeks. Brain MRI demonstrated a soft tissue mass sized as 5.3×3.7×3.1 cm with well-defined osteolysis on the midline of the frontal bone. The mass attached to anterior falx without infiltration into the brain parenchyme. The tumor had extracranial and extraaxial extension with bone destruction. The tumor was totally removed with craniectomy and she had an adjuvant radiotherapy. However, an isolated subcutaneous metastasis developed at the both preauricular area of the scalp, originating from the scar which was remained the first surgery. After complete removal of this metastasis, she had an adjuvant radiotherapy in other hospital. However, she expired after six months after first surgery. We believe that the occurrence of tumor seeding at the site of incision in the scalp is related to using the fluid for irrigation after tumor resection and the same surgical instruments for the removal of the brain tumor.
Primary sarcomas of the central nervous system (CNS) are rare. An overall estimate in the range of 1.2% of intracranial tumor is reasonable [12]. These lesions are believed to originate from mesenchymal precursors of mesodermal and ectodermal origin, and rapid growth often produces mass effect on the brain. Diagnosis is rendered pathologically following resection, but MRI can reveal initial findings suggestive of meningeal sarcomas [3]. The infiltrative nature of these tumors and the dense adhesions to neighboring structures such as major vessels make surgical excision a difficult task. However, Surgical resection is the mainstay treatment and must be preceded by radiographical determination of the extent of the primary lesion and possible metastatic deposits. The role of adjuvant therapy is not well established given the rarity of the diagnosis.
In our report, a 44-year-old female has been presented with an unusual seeding of the cranial meningeal sarcoma in her scar on the scalp which was remained the first surgery, 8 weeks after the removal of the tumor. The patient underwent second operations for resection of masses on the scalp.
We speculate that the main cause of tumor recurrence is the use of the fluid for irrigation and the same surgical instruments already used during the primary tumor resection.
This 44-year-old female was admitted to our department, due to growing mass at the midline of frontal head.
No neurological deficits were identified during the physical examination. CT and MRI revealed a contrast-enhanced tumor at the midline of frontal bone, which was spreading toward the scalp and the brain cortex with bone destruction (Fig. 1, 2).
First, tumor infiltrated bone was removed with a tumor free margin. The intracranial portion of the lesion was then resected with a narrow safety margin. The tumor was cut in frontal area with en bloc resection.
After the cranioplasty with medpore, the scalp was closed. Standard neurosurgical precautions for dealing with tumors, such as drapping, irrigation and suction, were carefully applied.
The patient’s recovery from surgery had natural course, with no event and no sign of neurological deficit. Five weeks after the tumor removal, adjuvant radiotherapy was started with the regimen of 50 Gy in 25 fractions over 5 weeks. Eight weeks after the tumor removal, an isolated subcutaneous masses developed at the both preauricular area of the scalp, originating along the scar left by the previous surgery, in an area unrelated to the resection margin (Fig. 3, 4).
In general, primary meningeal sarcomas are a rare group of intracranial malignant mesenchymal neoplasms without strong evidence-based treatment guidelines [23]. Among these few primary brain sarcomas, 70% arise in the pediatric population and there have been limited cases reported in adults [1]. Believed to arise from pleuripotential mesenchymal cells in the dura mater and leptomeninges, these tumors are known for rapid proliferative potential and a dismal prognosis despite aggressive surgical excision and chemoradiotherapy [4]. Inherently, these tumors are not radiosensitive and the role of chemotherapy is not yet well established, though is usually attempted. Therefore, an aggressive surgical excision remains the mainstay of therapy [3]. The biological behavior of these lesions is largely unknown and recurrence and metastatic formation is a known phenomena [4].
Different kinds of metastatic formation have been documented for diverse types of intracranial tumor with malignant potential. Those include spreading through blood, lymph, Cerebrospinal fluid (CSF), and surgical treatment. Iatrogenic seeding of neoplasms may occur during various types of surgical interventions [5]. Surgical seeding of various types of CNS tumors has been reported.
As a retrospective review of patients treated for scalp metastases of meningiomas, spreading of meningioma cells during surgery is a possible mechanism for scalp metastasis. Factors associated with scalp metastases of meningiomas include reoperations, radiation therapy, immunosuppression, CSF fistula, and torpid course of the surgical wound [6].
A case report of recurrence of tumor in the lateral part of the left thigh over the previous incision of fascia lata graft to reconstruct the dura mater following removal of the brain tumor. Highly suspected reason for implantation of the tumor on the other areas, is using the same surgical instruments, surgical gowns and surgical gloves, and whatever used in the tumor sites [5].
Another case report and review of the literature revealed 28 cases of CNS tumors demonstrating evidence of extraneural spread associated with ventriculo-peritoneal shunt in children. Ventriculo-peritoneal shunt should be considered as potential causes for increasing abdominal distention and ascites in patients with histories of intracranial malignancies [7].
In some cases of high grade glioma or glioblastoma, remote cutaneous metastasis, or metastatic seeding through the stereotactic biopsy tract have been reported. The case of stereotactic needle biopsy for glioblastoma, tumor cells were spilled and implanted during removal of the needle [8].
In our case, we believe that some fluid for irrigation and surgical instruments used for resection of the brain tumor were responsible for seeding of the tumor along a surgical trajectory on the scalp.
In conclusion, based on the present case, we concluded that a reason for implantation of the tumor on the other areas, is the irrigation fluid that is running through the tumor site and using the same surgical instruments which were already used in the tumor site. And this case demonstrates that meningeal sarcoma carry a risk of dissemination during surgery, even when precautions are taken seriously.
We suggest that surgical instruments, surgical gowns, surgical gloves, and whatever used in the tumor site be substituted with the new ones when the resection of the tumor is finished, entirely. And the fluid for irrigation of surgical site are used sufficiently.
Figures and Tables
Fig. 1
Axial CT scan (soft-tissue window) of the head, demonstrating extraaxial and extracranial tumor masses. Axial CT scan (bone window) demonstrating irregular destruction of the skull.

Fig. 2
Axial and sagittal MRI demonstrating an irregular contrast-enhancing mass lesion with compression anterior falx and midline of frontal lobe.

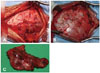
Fig. 3
Gross appearance of the patient’s head with the enlarged, painful palpable mass on the both preauricular area of the scalp along the scar left by the surgery.

Fig. 4
Axial contrast-enhanced MRI of the head demonstrating the heterogeneous contrast-enhancing scalp lesions on the bilateral temporal areas.

References
1. Palta M, Riedel RF, Vredenburgh JJ, et al. Primary meningeal rhabdomyosarcoma. Sarcoma. 2011; 2011:312802.

2. Sugita Y, Shigemori M, Harada H, et al. Primary meningeal sarcomas with leiomyoblastic differentiation: a proposal for a new subtype of primary meningeal sarcomas. Am J Surg Pathol. 2000; 24:1273–1278.
3. Cummings M, Chowdhry V, Shah H, Back J, Kennedy GA. Recurrent meningeal sarcoma successfully treated with stereotactic radiosurgery. J Neurosurg Pediatr. 2012; 10:434–438.

4. Singla N, Kapoor A, Chatterjee D. Undifferentiated meningeal sarcoma of childhood presenting as hard mass adhered to major intracranial vessels. Childs Nerv Syst. 2016; 32:771–773.

5. Maddah G, Shabahang H, Zehi V, Sharifi Sistani N, Mashhadi Nejad H. Iatrogenic seeding of tumor cells in thigh soft tissue upon surgical removal of intracranial meningioma. Basic Clin Neurosci. 2016; 7:159–164.

6. Avecillas-Chasin JM, Saceda-Gutierrez J, Alonso-Lera P, et al. Scalp Metastases of Recurrent Meningiomas: Aggressive Behavior or Surgical Seeding? World Neurosurg. 2015; 84:121–131.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download