Abstract
Background
Up to 15% of all patients with brain metastases have no clearly detected primary site despite intensive evaluation, and this incidence has decreased with the use of improved imaging technology. Radiosurgery has been evaluated as one of the treatment modality for patients with limited brain metastases. In this study, we evaluated the effectiveness of radiosurgery for brain metastases from unknown primary tumors.
Methods
We retrospectively evaluated 540 patients who underwent gamma knife radiosurgery (GKRS) for brain metastases radiologically diagnosed between August 1992 and September 2007 in our institution. First, the brain metastases were grouped into metachronous, synchronous, and precocious presentations according to the timing of diagnosis of the brain metastases. Then, synchronous and precocious brain metastases were further grouped into 1) unknown primary; 2) delayed known primary; and 3) synchronous metastases according to the timing of diagnosis of the primary origin. We analyzed the survival time and time to new brain metastasis in each group.
Results
Of the 540 patients, 29 (5.4%) presented precocious or synchronous metastases (34 GKRS procedures for 174 lesions). The primary tumor was not found even after intensive and repeated systemic evaluation in 10 patients (unknown primary, 34.5%); found after 8 months in 3 patients (delayed known primary, 1.2%); and diagnosed at the same time as the brain metastases in 16 patients (synchronous metastasis, 55.2%). No statistically significant differences in survival time and time to new brain metastasis were found among the three groups.
About 40% of systemic cancer patients have one or more brain metastases [1]. Surgical resection, whole brain radiotherapy (WBRT), radiosurgery, and chemotherapy are modalities of brain metastasis treatment, and treatment decision is made based on patient age, performance status, systemic disease status, brain metastasis status, and so on. For the treatment of limited brain metastases, radiosurgery has become the standard of treatment and could defer WBRT as late as possible to avoid neurocognitive dysfunction [23456].
Up to 15% of all patients with brain metastases have no clearly detected primary site despite intensive evaluation, even though the incidence is decreasing owing to improved imaging technology. However, the outcome of patients with brain metastases of unknown primary origin is still controversial [7891011].
The aim of this study was to compare the effectiveness of gamma knife radiosurgery (GKRS) for brain metastases of unknown primary origin according to the timing of diagnosis of the primary tumor.
We performed GKRS for 540 patients with brain metastases from August 1992 to September 2007 in our institution. The study was approved by the Institutional Review Board of our institution (IRB No.: 4-2016-0734), as specified in the Declaration of Helsinki. Of the 540 patients, 29 (5.4%) presented with precocious or synchronous metastases (34 GKRS procedures for 174 lesions). The primary tumor was not found even after intensive and repeated systemic evaluation in 10 patients (unknown primary, 34.5%), was disclosed after 8 months in 3 patients (delayed known primary, 10.3%), and diagnosed up to 2 months before the diagnosis of the brain metastases in 16 patients (synchronous metastasis, 55.2%). Of the 29 patients, 17 were men and 12 were women. The mean age of the patients at the time of GKRS was 57.7 (range, 40–79) years. The median follow up duration was 16.0 (range, 1–35) months. The clinical, radiological, and radiosurgical data were retrospectively reviewed (Table 1).
GKRS was performed by using Leksell Gamma Knife Type C or Perfexion (Elekta Instrument AB, Stockholm, Sweden) under local anesthesia. Preoperative T1-weighted magnetic resonance images (MRI) with gadobutrol (Gd, Gadovist; Bayer Schering Pharma AG, Leverkusen, Germany) were used for dose planning. The images were transferred to a GammaPlan treatment system, and the treating neurosurgeon determined the target volume and identified the critical structures. Treatment plans were constructed with single or multiple shots by using several sizes of collimators in order to construct a three-dimensional plan that conformed to each target. The mean (SD) tumor margin dose was 17.6 (3.9) Gy.
The Statistical Package for the Social Sciences version 20.0.0 (IBM, Armonk, NY, USA) was used. We analyzed survival time and time to new brain metastasis, and compared each among the 3 groups. Data were analyzed by using the Kaplan-Meier survival analysis and log-rank (Mantel-Cox) test. A p value of <0.05 was considered statistically significant.
Clinical follow-up data were available for 29 patients. Initially, brain metastases were radiologically diagnosed by experienced neuroradiologists in most cases. We performed brain biopsy in 7 patients. There were 6 brain lesions in average on a MRI (Table 1).
The estimated median survival time in each group was 27.1 months in the unknown primary group, 35.3 months in the delayed known primary group, and 25.2 months in the synchronous metastasis group. The difference in survival time among the groups was not statistically significant (Fig. 1).
The median times to new lesion detection after GKRS in each group were as follows: 4.6 months in the unknown primary group, 12.1 months in the delayed known primary group, and 10.4 months in the synchronous metastasis group (p>0.05) (Fig. 2).
Of the 19 patients in the delayed known primary and synchronous metastasis group, the most common site of the primary cancer was the lung in 12 patients, followed by the breast in 2 patients. The other sites were the liver, stomach, ovary, thyroid, and heart (Table 1). Diagnosis of the primary tumor could be confirmed by using brain biopsy in 3 patients and the primary site in 11 patients. Brain biopsy was performed in 7 patients, but the diagnosis of the primary tumor was possible in only 3 patients (42.9%). Leptomeningeal seeding occurred in one patient who got brain biopsy as a complication of biopsy.
Nineteen patients died during the follow-up period. Among these patients, 15 (78.9%) died of systemic cause; 3 (15.8%), of brain metastasis progression; and 1, of intracerebral hemorrhage not related to brain metastasis.
Over the last two decades, radiosurgery has become an alternative treatment modality for brain metastases. Many authors reported the efficacy of radiosurgery in comparison with that of surgical resection alone, WBRT alone, or combination therapies. Currently, radiosurgery is the treatment of choice for limited brain metastases to defer unnecessary WBRT in terms of neurocognitive dysfunction, repeated brain metastases, and so on [123456].
Brain metastases are divided into metachronous, synchronous, and precocious presentations according to the timing of the brain metastasis. Metachronous metastasis is defined as brain metastasis occurring >2 months after the diagnosis of the primary cancer; synchronous metastasis, as brain metastasis occurring within 2 months of the diagnosis of the primary cancer; and precocious metastases, as brain metastasis diagnosed before the primary cancer is found. Synchronous and precocious brain metastases are often grouped together for evaluation. Up to 15% of all patients with brain metastases have no clearly detected primary cancer even after intensive and repeated systemic evaluations. The incidence of brain metastases of unknown primary origin is decreasing owing to the improvements of imaging technology. However, only a few studies have reported results about the outcome of patients with unknown primary brain metastases, and the results are discrepant [7891011].
Le Chevalier et al. [8] reported 120 consecutive cases of patients who presented with brain metastases as the primary sign of malignancy. In 58 patients, the primary site remained unknown. However, survival was almost identical between the patients with known and unknown primary sites. They concluded that extensive evaluations to identify primary sites do not appear to be rational in patients presenting with brain metastases. Nguyen et al. [9] also reported that the overall survival of patients whose primary tumors were known was similar to that of patients in whom the primary tumor remained unknown. D’Ambrosio and Agazzi [10] reported that if a patient presents with brain metastases, overall prognosis is not affected by previous knowledge of a primary tumor and that whether the primary tumor was eventually found did not affect survival rates. They treated metastatic brain tumors with resection followed by WBRT, GKRS with WBRT, WBRT alone, or steroid alone. In our study, we compared survival time and time to new brain metastases between the unknown primary, delayed known primary, and synchronous metastasis groups that were treated with GKRS only. Our results showed no statistically significant differences, which might be caused by the modest progression of the primary cancers.
Agazzi et al. [12] reported that the lung was the most frequent primary site with significantly higher relative frequency in patients with initially unknown primary sites than in patients with known primary sites. Our data showed similar results, and in 12 of 19 patients, the primary cancer whose diagnosis was delayed was located in the lung. This might be due to the characteristic of lung cancer in aspects of limitation of chest radiography and computed tomography. In our series, one patient was finally diagnosed as having brain metastases from a rare cardiac myxoma.
Primary cancer origin and the efficacy of GKRS are controversial. Gerosa et al. [13] reported that the results of treatment with GKRS alone were better than those with WBRT and are comparable with the results of the best-selected surgery-radiation series, even for oncotypes unresponsive to therapeutic radiation, cystic tumors, and brain stem tumors. However, Black et al. [14] suggested that primary histology affected local failure rates in case of comparing breast cancer, lung cancer, and melanoma. According to our results, the origin of brain metastases did not influence patient survival time and disease progression. In addition, GKRS alone for primary unknown brain metastases was an effective and successful treatment modality.
Multiple brain enhancing lesions do not always mean metastatic brain tumors, even in patients who have a systemic ca-ncer history. Many other possibilities include lymphomas, mu-ltifocal or multicentric high-grade gliomas, infectious diseases such as tuberculoma, demyelinating diseases, and vasculitis. Therefore, accurate diagnosis of multiple brain lesions is essential before making the treatment decision for brain lesions. When the primary cancer is not diagnosed radiologically or pathologically, we could consider biopsy for brain lesions. However, even after brain biopsy, the diagnosis of metastatic brain tumors could be made, but the estimation of primary ca-ncer is not usually easy, except for several pathologically distinct tumors such as choriocarcinoma, melanoma, renal cell carcinoma, and advanced gastric cancer. Moreover, biopsy-related complications could occur, such as hemorrhage, infection, or leptomeningeal spread [151617]. Hence, we should decide to perform brain biopsy in selective cases and diagnose by using mostly radiological and clinical examinations.
We conclude that GKRS is an effective treatment modality even for brain metastases from unknown primary tumors. Identification of a primary tumor before GKRS did not affect the patients’ outcome. If other possible differential diagnoses were completely excluded, delaying the optimal treatment of brain metastases by evaluating the primary origin may not be appropriate.
Figures and Tables
Fig. 1
Kaplan-Meier curve of survival time showing no statistically significant difference in median survival time after gamma knife radiosurgery among the groups (p>0.05). Cum survival, cumulative survival; Survival time, survival time in months; Unknown, unknown primary group; Delayed, delayed known primary group; Synch, synchronous metastasis group.
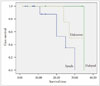
Fig. 2
Kaplan-Meier curve of the time to new brain metastases showing no statistically significant difference in median time to new brain metastases among the group (p>0.05). Cum survival, cumulative survival; Survival time, survival time in months; Unknown, unknown primary group; Delayed, delayed known primary group; Synch, synchronous metastases group.
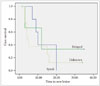
Table 1
Clinical characteristics of patients

References
2. Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004; 363:1665–1672.

3. Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 2006; 295:2483–2491.

4. Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009; 10:1037–1044.

5. Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011; 29:134–141.
6. Pirzkall A, Debus J, Lohr F, et al. Radiosurgery alone or in combination with whole-brain radiotherapy for brain metastases. J Clin Oncol. 1998; 16:3563–3569.

7. Debevec M. Management of patients with brain metastases of unknown origin. Neoplasma. 1990; 37:601–606.
8. Le Chevalier T, Smith FP, Caille P, Constans JP, Rouesse JG. Sites of primary malignancies in patients presenting with cerebral metastases. A review of 120 cases. Cancer. 1985; 56:880–882.

9. Nguyen LN, Maor MH, Oswald MJ. Brain metastases as the only manifestation of an undetected primary tumor. Cancer. 1998; 83:2181–2184.

10. D’Ambrosio AL, Agazzi S. Prognosis in patients presenting with brain metastasis from an undiagnosed primary tumor. Neurosurg Focus. 2007; 22:E7.
11. Maesawa S, Kondziolka D, Thompson TP, Flickinger JC, Dade L. Brain metastases in patients with no known primary tumor. Cancer. 2000; 89:1095–1101.

12. Agazzi S, Pampallona S, Pica A, et al. The origin of brain metastases in patients with an undiagnosed primary tumour. Acta Neurochir (Wien). 2004; 146:153–157.

13. Gerosa M, Nicolato A, Foroni R, et al. Gamma knife radiosurgery for brain metastases: a primary therapeutic option. J Neurosurg. 2002; 97:5 Suppl. 515–524.

14. Black PJ, Page BR, Lucas JT Jr, et al. Factors that determine local control with gamma knife radiosurgery: The role of primary histology. J Radiosurg SBRT. 2015; 3:281–286.
15. Bouillot-Eimer S, Loiseau H, Vital A. Subcutaneous tumoral seeding from a glioblastoma following stereotactic biopsy: case report and review of the literature. Clin Neuropathol. 2005; 24:247–251.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download