Abstract
An intracranial cyst tumor with a mural nodule can be representative of some types of brain tumors, but is a rare presentation of intracranial inflammatory myofibroblastic tumor (IMT). Herein, we report the case of an intracranial IMT in a 48-year-old woman presenting with the extremely unusual radiologic findings of a cyst with a mural nodule.
A cyst with a mural nodule tumor in the central nervous system (CNS) is commonly seen in a variety of fluid-secreting tumors, such as hemangioblastoma, pilocytic astrocytoma, ganglioglioma, pleomorphic xanthoastrocytoma, tanycytic ependymoma, intraparenchymal schwannoma, desmoplastic infantile ganglioma, and cystic metastasis. Rarely, parenchymal perianeurysmal cyst, cavernous angioma, and neurocysticercosis can also appear as a cyst with a mural nodule [1].
In previous reports, inflammatory myofibroblastic tumors (IMTs) were described as a solid enhancing mass without cystic features [2]. Herein, we report one case of IMT with extremely unusual radiologic findings of a cyst with a mural nodule.
A 48-year-old woman visited our hospital with her family due to depression, paranoid personality, and memory impairment, which began several months prior. The findings of general physical examination and neurological examination were within normal limits. Magnetic resonance imaging (MRI) was performed using a 3.0-T Skyra scanner (Simens, Erlangen, Germany). T2-weighted MRI revealed an intraaxial cystic mass in the right temporal region measuring 5.3×4.2 cm with an irregular margin and internal hypodense sepatation. Peritumoral edema was not observed (Fig. 1A). On gadolinium-enhanced T1-weighted MRI, a nodular mass was seen in the anterior part of the cyst in contact with the dura. Neither dural tail sign nor broad dural basement was noted (Fig. 1B). The tumor was not restricted on diffusion-weighted MRI (Fig. 1C). Based on these radiologic findings, the preoperative diagnosis was pleomorphic xanthoastrocytoma, cystic meningioma, or another cystic glioma.
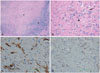
On microscopic surgical findings, the nodular lesion of the tumor was hard and had poor vascularity. There was tight adhesion between the nodular mass and the dura. The cyst contained a yellowish fluid and was well demarcated from normal brain parenchyma. Total resection was performed surgically. Histopathology of the mural nodule revealed a mixture of hyalinized hypocellular stroma and an inflammatory area containing plasma cells and lymphocytes (Fig. 2A, B). On immunohistochemical staining, the tumor showed focal staining for smooth muscle actin (Fig. 2C) and was negative for desmin (Fig. 2D). Glial fibrillary acidic protein, S-100 and anaplastic lymphoma kinase were negative. Based on these pathologic findings, the tumor was diagnosed as IMT.
During a four-year follow-up period, the patient demonstrated improvement in memory function and showed no signs of tumor recurrence (Fig. 1D).
IMT is a relatively rare disease and occurs in the lung, mesentery, omentum, retroperitoneum, genitourinary tract or upper respiratory tract [34]. IMT is diagnosed based on histopathologic findings of inflammatory cell infiltration and vari-able fibrosis. Thus, it has also been called inflammatory pseu-dotumor, plasma cell granuloma, fibrous xanthoma, xantho-matous pseudotumor, pseudosarcomatous myofibroblastic proliferation, inflammatory myofibrohistiocytic proliferation, and myofibroblastoma [5]. However, in the 2002, the World Health Organization classified it as a soft tissue tumor and named it IMT [6].
According to the review of the literature, IMT involving the CNS is a very unusual event and mostly affects children and young adults [7]. Although the radiologic findings of IMT are nonspecific, IMT generally shows hypointensity on T1- and T2-weighted MRI, as well as marked gadolinium enhancement [8]. On MR spectroscopy, lactate can be detected by hypoxia and inflammatory reaction. N-acetyl aspartate can be reduced by loss of normal neuronal elements and choline can be increased by cell membrane synthesis increase due to inflammatory cell hyperplasia on MR spectroscopy [9]. In previous cases, all intracranial IMTs were described as a solid lesion, except one case. Nawashiro et al. [2] reported the first cystic intracranial IMT with a solid mural nodule in the right frontal lobe manifesting as progressive left paresis. To the best of our knowledge, this is the second reported case of a cystic intracranial IMT with a mural nodule.
Häusler et al. [7] analyzed 57 cases of brain IMT and divided them into 5 groups: dural/meningeal lesions, intraparenchymatous lesions, mixed intraparenchymatous/meningeal lesions, intraventricular lesions, and lesions extending from intracerebral to extracerebral sites. They reported that most intracranial IMTs affected the dural/meningeal structures. In our case, the solid part of the tumor was adhered to the dura tightly and the cystic part involved the brain parenchyma, so it was classified as a mixed intraparenchymatous/meningeal lesion.
Surgical resection is considered the optimal treatment for IMT; radiotherapy with or without corticosteroid can also be used in recurrent or unresectable cases [10]. The recurrence rate is 40% within 2 years in general, and is higher in cases of incomplete resection and in females [7]. After incomplete surgical resection, patients must be followed closely.
In conclusion, intracranial IMT can rarely present as a cyst with a mural nodule and should be considered in the differential diagnosis of intracranial cyst with mural nodule lesions. Surgical resection and histopathologic examination of solid mural nodules are essential for the accurate diagnosis of IMT.
Figures and Tables
Fig. 1
Intracranial inflammatory myofibroblastic tumor presenting as a cyst with a mural nodule in a 48-year-old woman. A: T2-weighted MRI shows a large cyst with septation in the right temporal lobe. An iso-signal-intense mass compared to gray matter is also seen in the anterior portion of the cyst. B: Contrast-enhanced T1-weighted MRI shows a strongly enhanced mural nodule. C: The tumor was not restricted on diffusion-weighted MRI. D: There was no evidence of recurrence on MRI 4 years later.

Fig. 2
The findings of immunohistochemical staining for mural nodule. A: At low magnification, the tumor is composed of a hyalinized fibrotic area (★) and a dense inflammatory area (arrowhead) (hematoxylin & eosin staining, ×40). B: The hyalinized area includes plasma cells (black arrow), lymphocytes (arrowhead), and atypical spindle cells (white arrow) in a collagenous background (×200). C: The stromal area is focally stained with smooth muscle actin (×400). D: Immunostaining for desmin is negative (×400).
References
1. Raz E, Zagzag D, Saba L, et al. Cyst with a mural nodule tumor of the brain. Cancer Imaging. 2012; 12:237–244.

2. Nawashiro H, Omura T, Kobayashi H. Cystic intracranial plasma cell granuloma. J Neurosurg. 2006; 105:799. author reply 799-800.

3. Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995; 19:859–872.

4. Matsubara O, Tan-Liu NS, Kenney RM, Mark EJ. Inflammatory pseudotumors of the lung: progression from organizing pneumonia to fibrous histiocytoma or to plasma cell granuloma in 32 cases. Hum Pathol. 1988; 19:807–814.

5. Biselli R, Boldrini R, Ferlini C, Boglino C, Inserra A, Bosman C. Myofibroblastic tumours: neoplasias with divergent behaviour. Ultrastructural and flow cytometric analysis. Pathol Res Pract. 1999; 195:619–632.

6. Fletcher CDM, Unni K, Mertens F. Pathology and Genetics, Tumors of Soft Tissue and Bone. World Health Organization Classification of Tumors. Lyon: IARC press;2002. p. 91–93.
7. Häusler M, Schaade L, Ramaekers VT, Doenges M, Heimann G, Sellhaus B. Inflammatory pseudotumors of the central nervous system: report of 3 cases and a literature review. Hum Pathol. 2003; 34:253–262.

8. Park SB, Lee JH, Weon YC. Imaging findings of head and neck inflammatory pseudotumor. AJR Am J Roentgenol. 2009; 193:1180–1186.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download