NF1, also known as von Recklinghausen disease, is characterized by multiple skin lesions (café-au-lait spots, axillary and/or inguinal freckling), Lisch nodules, and various tumors including optic glioma, brain tumors, soft-tissue sarcomas, carcinomas (breast, lungs, gastrointestinal tract, thyroid, pharynx, ovaries), malignant melanoma, pheochromocytomas [
5,
6,
7]. The majority of intracranial tumors with NF1 are pilocytic astrocytomas and optic gliomas which are thought to be pathologically low grade. Up to the year 2010, 12 patients with NF1 associated with glioblastoma had been reported [
4]. Among them four occurred in adults. One patient was clinically represented with progressive multiple sclerosis and neurofibromatosis but glioblastoma remained silent during the patient's life. The pathology of glioblastoma was revealed by autopsy [
8].
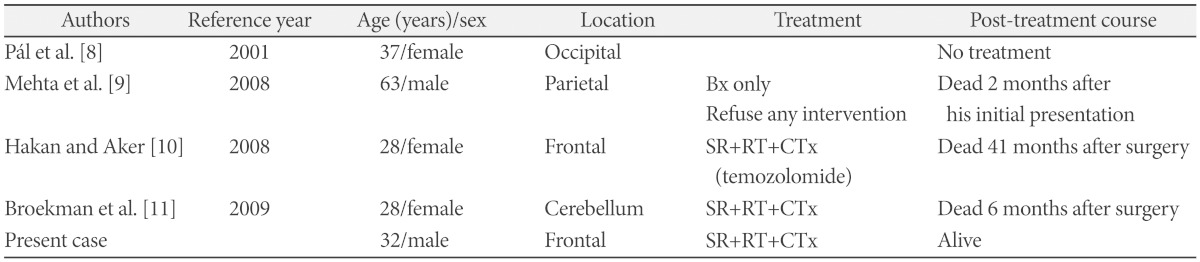
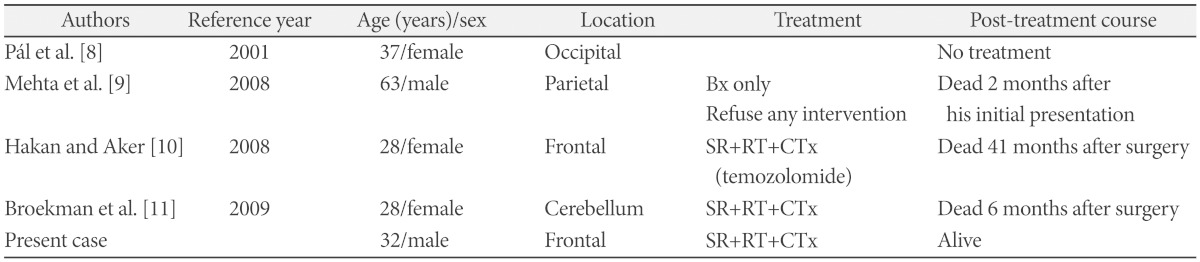
Table 1 shows the characteristics of the glioblastomas with NF1 in adults [
8,
9,
10,
11]. Huttner et al. [
4] reviewed five glioblastoma patients in children with NF1 and reported their clinicopathologic features. This study suggested that pathological features such as increased
p53 expression, increased
EGFR amplification, and increased proliferative indices might have predicted a worse overall outcome. They also provided that the survival of glioblastoma patient with NF1 was better than those without NF1. The median overall survival of patients with and without NF1 was 9.25 and 1.08 years respectively. However, because of the limited number of patients, further investigation is needed. In adults, glioblastoma is the most common and aggressive primary brain tumor. The methylation status of the
MGMT gene promoter is currently a promising molecular prognostic marker. There is a significant association between
MGMT promoter methylation and the outcome of glioblastoma patients treated with temozolomide. Molecular analysis of glioblastomas arising in NF1 patients showed the presence of genetic alterations such as
p16INK4A/ARF deletion and
p53 mutations [
12]. Some studies have reported the cooperation of mutations in NF1 and
p53 in the development astrocytomas in transgenic mice [
13,
14]. In our case, the promoter methylation of
MGMT gene was not observed. Immunohistochemical findings were positive for GFAP, and negative for
EGFR. Preliminary studies reported that the prognosis of glioblastoma with NF1 in children may differ from patient without NF1 [
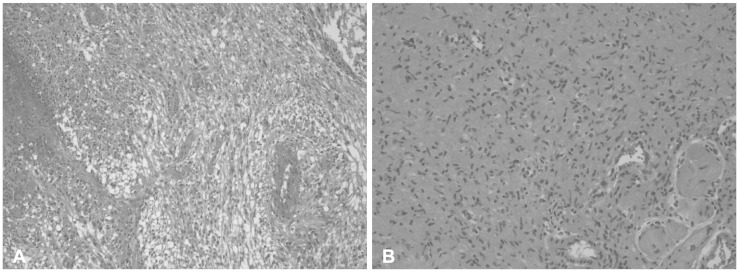
4]. In adults, there is limited information about glioblastoma with NF1 cases. In this present case, the patient was treated using surgical excision and chemoradiotherapy with temozolomide. Further investigation for the glioblastoma patients with NF1 in adults would be necessary.
Table 1
The characteristics of previous cases of Glioblastoma with NF1 in adults





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download