INTRODUCTION
Papillary thyroid carcinoma (PTC) is known to relatively favorable neoplasm because of its slow clinical course and rare case of distant metastases [
1]. Distant metastases of PTC were reported in about 10% of cases [
2], but mestasizing to brain is extremely rare (0.4-1.2%) [
3]. Thyroid gland neoplasm can show hoarseness, swallowing difficulty, and hormonal disturbances. Most of all, thyroid gland neoplasm can easily be found because of palpable mass (such as goiter). However the mass can grows toward the mediastinum, lung apex, or retropharyngeal space, rather than the surface of neck. Malignant thyroid neoplasm very rarely present as Horner's syndrome [
4,
5]. We report extremely rare case of PTC with only symptoms of Horner's syndrome and incidental brain metastases of which could be easily be missed.
Go to :

CASE REPORT
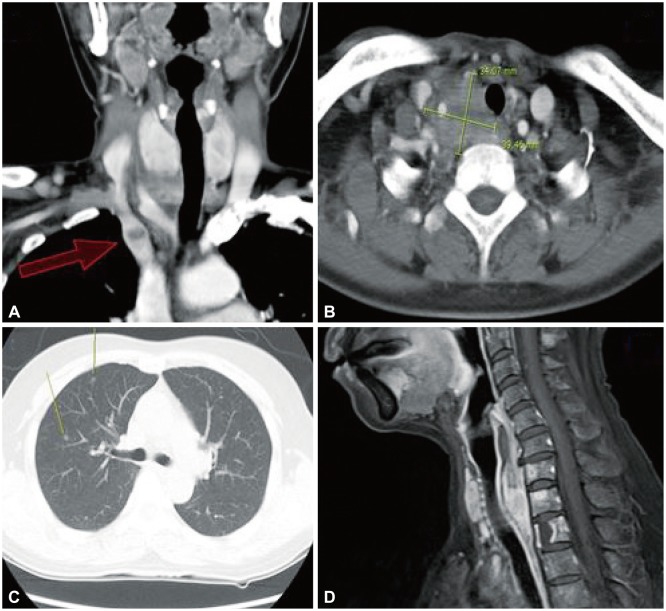
A 53-year-old woman, with past history of only hysterectomy due to uterine myoma 4 years ago previously, visited our institute for incidental brain tumor. She had been visiting a local ophthalmologic clinic for 3 months, because of right eye monocular blurred vision and foreign body sensation. At the time she was diagnosed as xerophthalmia, but showed no sign of improvement despite the 3 months management. She complained of more aggravated symptoms of blurred vision and even showed hemi-facial numbness. The ophthalmologist recommended further evaluation of cerebral lesion. She visited a neurological clinic for brain imaging [magnetic resonance imaging (MRI), magnetic resonance angiography (MRA)] to evaluate the possibilities of cerebral infarction, transient ischemic attack or brain tumor. The brain MRI and MRA revealed a left frontal lobe cystic mass 1.7×2.2×2.1 cm in size. And it showed high signal intensity (SI) of T2 and low SI of T1 lesion with peripheral irregular enhancement. Although she visited our institute for visual disturbance and incidental cerebral mass, we thought that there was no connection between the cerebral lesion and neurologic symptoms. So we thoroughly performed neurological exam again. We suggested right side Horner's syndrome and diagnosis confirmation was done by the ophthalmologic department in our institute through the pharmacological test.
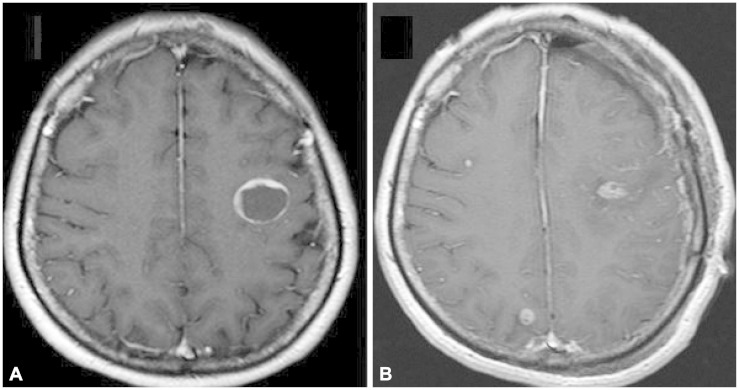
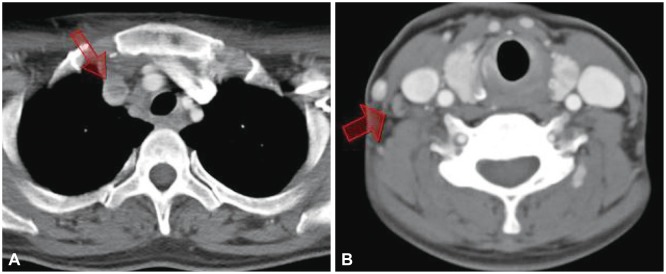
Further evaluation, positron-emitting tomography-computed tomography (PET-CT) (
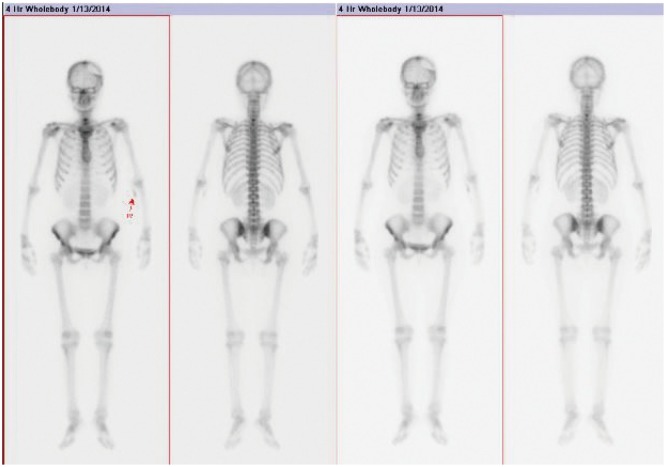
Fig. 1), chest CT, neck CT, neck MRI revealed that thyroid mass invading mediastinum, apex of lung, right common carotid artery, retropharyngeal space (
Fig. 2), and even right internal jugular vein with tumor th-rombus (
Fig. 3). There was no definite goiter in physical exam, because of tumor growth in the caudal and dorsal direction.
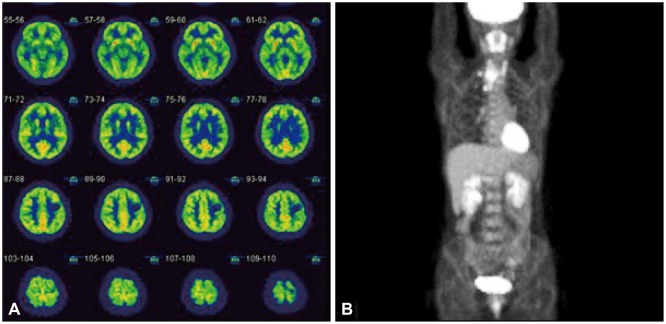 | Fig. 1Fluorodeoxyglucose-positron-emitting tomography image of (A) brain and (B) Torso. A cold spot is located on the left frontal lesion, a tumor mass uptakes glucose more than white matter, but surrounding normal gray matter more actively uptakes glucose. Papillary thyroid carcinoma is shown as hot uptake of cervical lesion in the Torso. 
|
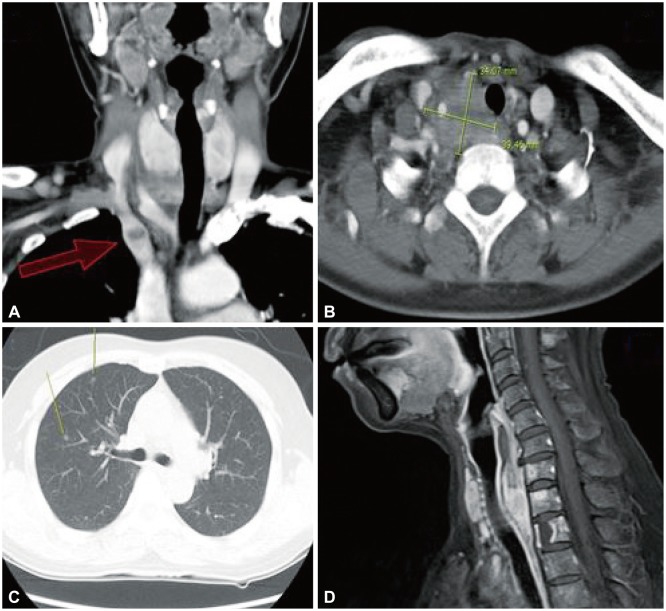 | Fig. 2The tumor growing toward mediastinum (red arrow) and retropharyngeal space and not which presenting goiter (A and D). The main mass located in deep cervical to lung apex lesion which encased major vessels and nerves, and deviated the trachea (B). Lung CT shows small nodular mass suspicious of metastasization from thyroid (C). 
|
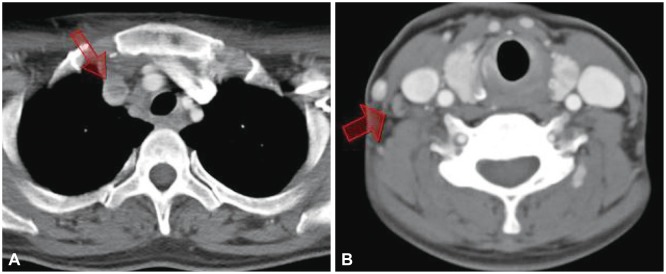 | Fig. 3Thyroid mass invaded into the vessel (arrow in A), with internal jugular venous thrombus (arrow in B) and cervical lymph node enlargement. 
|
Pre-operative thyroid function test was in normal range ex-cept for a high level of anti-thyroglobulin antibody (541.2 IU/mL, normal 0-70 IU/mL). There were no hormonal symptoms from thyroid or parathyroid gland dysfunction, and other laboratory results were also in normal range.
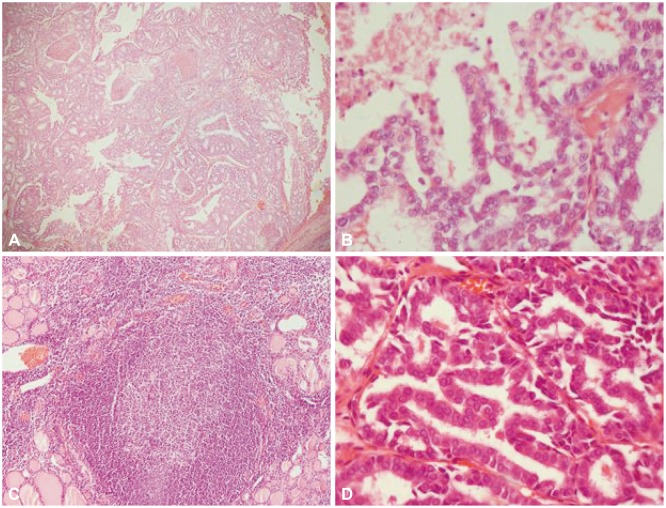
The fine needle aspiration biopsy was performed at right lobe of the thyroid gland. The pathologic diagnosis was PTC. To manage the primary lesion, total thyroidectomy with selective neck lymphatic dissection (III-IV) was performed in the otorhinolaryngologic department. Final pathologic diagnosis was PTC with tall cell variant and Hashimoto's thyroiditis (
Fig. 4). During the surgery, there were severe adhesions to surrounding tissue. To preserve major organs and structures, a small amount of tumor was remained. Her symptoms of mild ptosis, anhydrosis, and mild numbness of right hemi-facial area continued after the surgery.
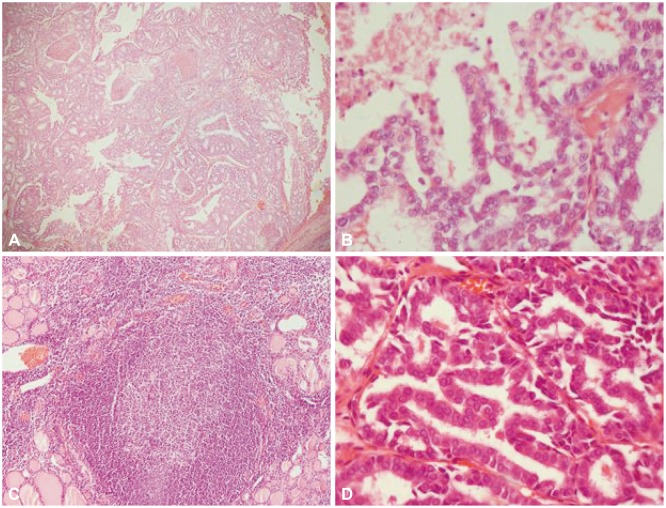 | Fig. 4Pathologic images of thyroid low magnification (A) and high magnification (B), which show irregular nuclear membrane with enlarged, grooved nucleus. Papillary thyroid carcinoma (PTC) coexisted with Hashimoto's thyroiditis (C). Metastasized cerebral tumor (D) showing same pathologic patterns as PTC. A and C: H&E, ×100. B and D: H&E, ×400. 
|
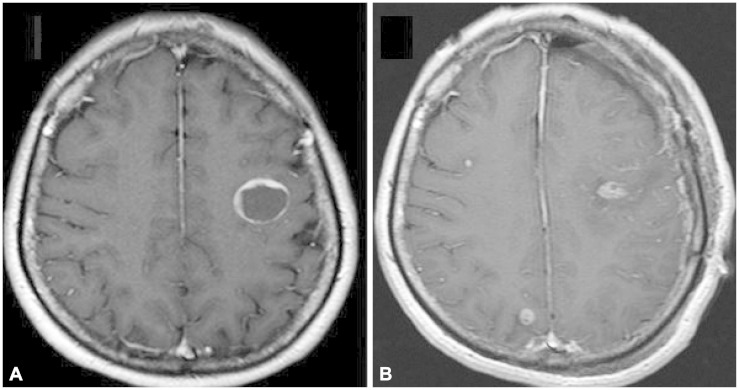
After the primary lesion controls, brain surgery was performed 3 weeks later. We planned to use of navigator system for accurate tumor evacuation of the brain. In the navigator CT image, the tumor size had increased significantly to about 3.3×3×3.1 cm, but mainly from the cystic lesion. Craniotomy and gross total tumor removal was done by using of navigator system. The metastasized brain lesion was well marginated from normal parenchyme. The frozen biopsy result of metastasized tumor was adenoma-typed malignancy, but final pathologic confirmation was same pathology of original site. Post-operative follow-up brain MRI image revealed complete removal of left frontal mass with two new small enhanced nodules on the right frontal and occipital lobe (
Fig. 5). During the post-operative period,
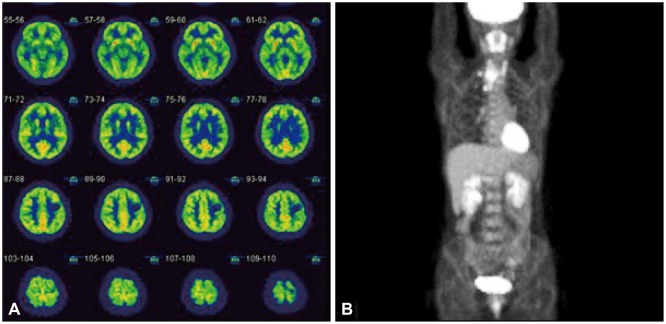
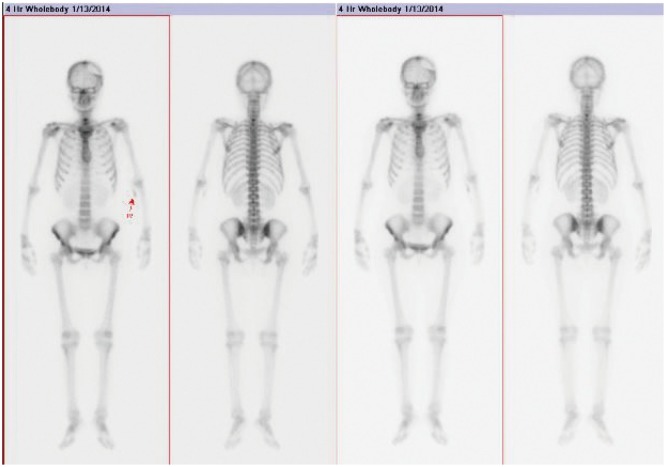
99mTc pertechnetate bone scan (
Fig. 6), and whole spine MRI were performed to evaluate distant metastases. It revealed additional metastases on 7th cervical, and 2nd thoracic vertebral body. We are planning whole brain radiotherapy with 30 Gy for remnant lesion first, then neck lesion radiotherapy and radioactive iodine ablation (
131I) for distant metastases.
 | Fig. 5Brain pre-operative enhanced MRI image (A). There is a single cystic mass in left frontal lobe. But in the post-operative enhanced MRI image (B) shows total removal of left frontal mass, but additional enhanced small mass were also found in right frontal and occipital lobe during the interval of 4 weeks. 
|
 | Fig. 6Bone scan with Tc-99m-pertechnetate shows a defect in the left parietal bone, as sequel of the recent craniotomy surgery. There is a metastatic skeletal hot uptake lesion of lower cervical spine. 
|
Go to :

DISCUSSION
Malignant thyroid neoplasm includes papillary, follicular, medullary, anaplastic pathologic types. Among them, PTC is the most common type of 65-80% [
6]. It has the most favorable prognosis, because they are a well differentiated type, usually juxta-nodal invasion and low incidence of vessel invasion or distant metastases [
3]. It has 97.8% and 94.9% of 5-year and 10-year survival rate, respectively in non-metastatic PTC [
7]. However, if it has metastasized to distant organs including lung or bone, their biological character can be aggressive. Blood-borne metastasis of PTC is very rare among the thyroid malignancies [
8]. Some reports found the mean survival rate to be about 12 months, if there is the extremely rare case of brain metastases [
1]. Our case also shows distant metastases including lung and spine, and even brain lesion.
The thyroid neoplasm is usually found because of symptoms of goiter, hoarseness, and sometimes through the regular screening test. In this case, however, there was no goiter or other symptoms. It shows only mild Horner's syndrome, including subjective visual disturbance, xerophthalmia and mild ptosis, but no awareness of anhydrosis or miosis. Classic symp-toms of Horner's syndrome are the combination of ptosis, miosis and hemifacial anhidrosis, and conjunctival injection of the eye or enophthalmos are often also present. This indicates a problem with the sympathetic nervous system related with facial lesion. Sympathetic nerve route associated with pupillary function can be divided into 3 lesions. The pre-ganglionic lesion is known as the most common origin site (21-67%) of Horner's syndrome, for example, compression or disruption by lung neoplasm. But thyroid mass lesion is an unusual cause of Horner's syndrome (0.14-1.3%) [
4,
5]. Paradoxically, the most common cause of the Horner's syndrome is due to malignancy including non-thyroidal lesion. But, in thyroidal lesion, benign thyroidal mass shows Horner's syndrome more frequently (83%) than malignancy [
9].
The thyroid mass presents Horner's syndrome by involving the second or third order neuron of sympathetic pathway. If the mass is confirmed as malignancy, we should consider the possibility of tumor invasion of major vessels including carotid artery or jugular vein. Even though there is little evidence that malignant thyroid neoplasm with Horner's syndrome always shows distant metastases, because of lack of collection, the possibilities should be considered. Generally, fluorodeoxyglucose (FDG)-PET is an excellent tool to evaluate the tumor metastases of the whole body. But when it comes to brain lesion, FDG-PET is not useful tool to detect brain metastases, because the brain metastases can often easily be obscured by the high FDG uptake of normal cortical gray matter [
10]. However enhanced MRI is considered precise. In this case, the tumor lesion shows relatively cold spot and if the size had been smaller, it would have been obscured (
Fig. 1).
The importance of physical and neurological examination is another point to emphasize. Especially, mismatched cases of brain imaging with neurologic symptoms should be re-considered. At first, there was no awareness of neck mass, and facial vague neurologic symptoms were the only clues in this case, and the brain metastatic lesion was found incidentally. If the classic evaluation of neurologic, physical examination was skipped, inappropriate and more risky study strategies would be selected or even led to misdiagnosis. For example, if there is a mass in cerebral eloquent area, attempts are usually made to get the tumor tissue through the biopsy or surgery, not taking into account the possibility of metastases. But kn-owing the primary site helped to find an easier access, diagnosis, and make the therapeutic strategy.
Although there is no definitely confirmed protocol for the treatment of brain metastases from thyroid cancer, surgery is generally considered to be the best therapeutic strategy for prolonged survival and regression of neurologic symptoms. After that, it is followed by radioiodine or external radiotherapy [
1].
We decided treatment strategy by consulting with medical-oncologist, radio-oncologist, and otorhinolaryngologist. The plan was primary and metastasized lesion tumor removal first, followed by conventional radiotherapies. Regular metastases evaluation, additional boost radiotherapy schedules or doses were also discussed. PTC with metastasized to central nervous system was reported as poor prognosis. However, there is a report about a patient who survived for more than 10 years by a combined approach of total thyroidectomy, resection of brain metastatic lesion, radioactive iodine (
131I), suppressive therapy with L-throxine, whole brain body radiotherapy with dose of 44 Gy, and gamma knife radiosurgery [
1]. This case needed a tailored treatment because it is an extremely rare case with no standard therapy.
In conclusion, PTC is the most common type of thyroid malignancy. A thyroid tumor can be easily detectable at an early stage because of a noticeable and palpable mass or early other symptoms. Moreover PTC usually has a favorable outcome because of its relatively well differentiated pathology and indolent clinical course. However, if the tumor grows toward lung apex, mediastinum or retropharyngeal space, detection can be late. We describe an extremely rare case of vague early Horner's syndrome symptoms but had cerebral metastasized PTC. In addition, we suggest that patients presenting with Horner's syndrome should have a proper investigation performed to look for any revealed mass lesions, vascular lesions, or other treatable disorders.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download