1. Kleihues P, Cavenee WK. World Health Organization classification of tumours. Pathology and genetics of tumours of the central nervous system. Lyon: IARC Press;2000.
2. Nevin S. Gliomatosis cerebri. Brain. 1938; 61:170–191.

3. Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993; 3:255–268. PMID:
8293185.

4. Crossen JR, Garwood D, Glatstein E, Neuwelt EA. Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol. 1994; 12:627–642. PMID:
8120563.

5. Imperato JP, Paleologos NA, Vick NA. Effects of treatment on long-term survivors with malignant astrocytomas. Ann Neurol. 1990; 28:818–822. PMID:
2178330.

6. Sanson M, Cartalat-Carel S, Taillibert S, et al. Initial chemotherapy in gliomatosis cerebri. Neurology. 2004; 63:270–275. PMID:
15277619.

7. Herrlinger U, Felsberg J, Küker W, et al. Gliomatosis cerebri: molecular pathology and clinical course. Ann Neurol. 2002; 52:390–399. PMID:
12325066.

8. Taillibert S, Chodkiewicz C, Laigle-Donadey F, Napolitano M, Cartalat-Carel S, Sanson M. Gliomatosis cerebri: a review of 296 cases from the ANOCEF database and the literature. J Neurooncol. 2006; 76:201–205. PMID:
16200347.

9. Chen S, Tanaka S, Giannini C, et al. Gliomatosis cerebri: clinical characteristics, management, and outcomes. J Neurooncol. 2013; 112:267–275. PMID:
23341100.

10. Seol HJ, Jung HW, Kim DG, Hwang SK, Yang HJ, Kim MK. Gliomatosis cerebri: clinical features and prognostic factors of long-term survival. J Korean Neurosurg Soc. 2002; 32:125–130.
11. Romero FJ, Ortega A, Titus F, Ibarra B, Navarro C, Rovira M. Gliomatosis cerebri with formation of a glioblastoma multiform. Study and follow-up by magnetic resonance and computed tomography. J Comput Tomogr. 1988; 12:253–257. PMID:
2848658.

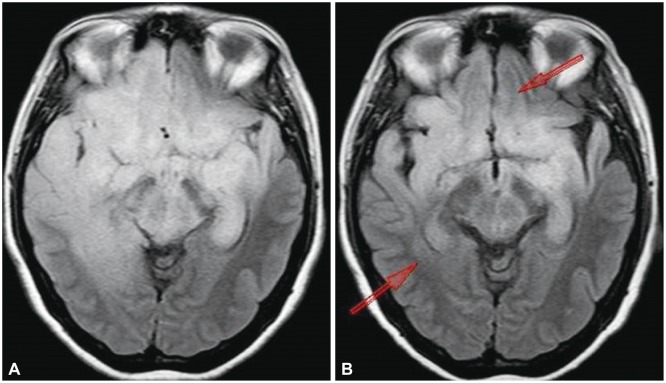
12. Shin YM, Chang KH, Han MH, et al. Gliomatosis cerebri: comparison of MR and CT features. AJR Am J Roentgenol. 1993; 161:859–862. PMID:
8372774.

13. Ponce P, Alvarez-Santullano MV, Otermin E, Santana MA, García Ludeña MV. Gliomatosis cerebri: findings with computed tomography and magnetic resonance imaging. Eur J Radiol. 1998; 28:226–229. PMID:
9881257.

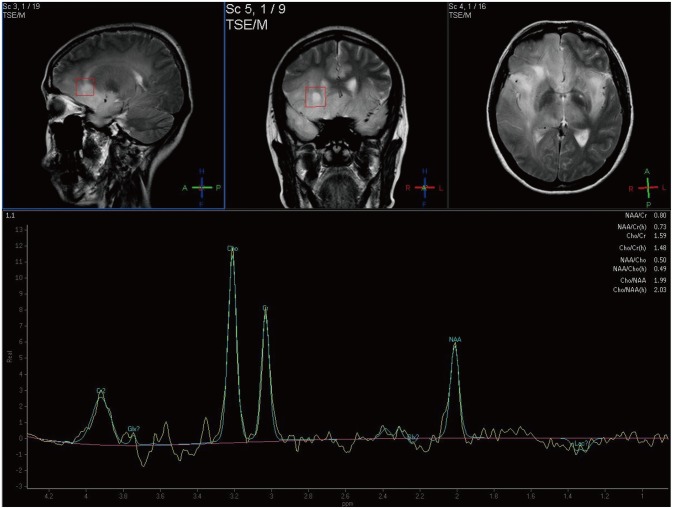
14. Bendszus M, Warmuth-Metz M, Klein R, et al. MR spectroscopy in gliomatosis cerebri. AJNR Am J Neuroradiol. 2000; 21:375–380. PMID:
10696026.
15. Osborn A, Blaser S, Salzman K. Diagnostic imaging: brain. 1st ed. Salt Lake City, UT: Amirsys Inc;2004. p. I–6. p. 26p. 29
16. Elshaikh MA, Stevens GH, Peereboom DM, et al. Gliomatosis cerebri: treatment results with radiotherapy alone. Cancer. 2002; 95:2027–2031. PMID:
12404298.
17. Levin N, Gomori JM, Siegal T. Chemotherapy as initial treatment in gliomatosis cerebri: results with temozolomide. Neurology. 2004; 63:354–356. PMID:
15277636.

18. Glas M, Rasch K, Wiewrodt D, Weller M, Herrlinger U. Procarbazine and CCNU as initial treatment in gliomatosis cerebri. Oncology. 2008; 75:182–185. PMID:
18841032.

19. Peyre M, Cartalat-Carel S, Meyronet D, et al. Prolonged response without prolonged chemotherapy: a lesson from PCV chemotherapy in low-grade gliomas. Neuro Oncol. 2010; 12:1078–1082. PMID:
20488959.

20. Glas M, Bähr O, Felsberg J, et al. NOA-05 phase 2 trial of procarbazine and lomustine therapy in gliomatosis cerebri. Ann Neurol. 2011; 70:445–453. PMID:
21710625.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download