Abstract
Multiple myelomas (MM) are characterized by monoclonal proliferation of immunoglobulin (Ig)-secreting plasma cells. Central nervous system involvement is a rare complication of MM, and it can present as either an intraparenchymal or a leptomeningeal lesion. A 77-year-old woman was transferred from the dementia clinic in July 2012. She had a large heterogeneous signal mass with central necrosis and with pial involvement in the left frontal lobe with destruction of the frontal bone that was observed on computed tomography and magnetic resonance imaging. Multiple punched out radiolucent lesions were also noted on the skull X-ray. Serum protein electrophoresis revealed an IgA-kappa monoclonal gammopathy. External lumbar drainage was helpful for treating the fluid collection underneath the scalp after an orbitozygomatic craniotomy with duroplasty.
Multiple myelomas (MM) are characterized by monoclonal proliferation of immunoglobulin (Ig)-secreting plasma cells. Neurological complications in MMs most frequently occur due to spinal cord compression by bone lesions, paraprotein-related neuropathy, hypercalcemia, hyperviscosity, or amyloidosis [1]. In particular, intracranial MM is an uncommon condition in middle-aged or elderly individuals who are diagnosed with MM [2]. The immunoglobulin types most frequently reported in association with MM are IgG and IgA, with an IgG κ isotype. The mechanism for the spread of plasma cells to the leptomeninges remains unclear. Plasma cells may, in a similar fashion to leukemic cells, extend to the central nervous system (CNS) through microscopic veins in the arachnoid membrane. Myeloma cells may also migrate into perivascular spaces and direct extension from bony lesions, or preexisting CNS plasmacytomas may occur. We would like to introduce a case showing an extensive meningeal and cerebral involvement with MM.
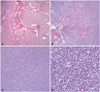
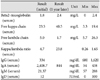
A 77-year-old woman from a neuropsychiatric dementia clinic with an abnormal magnetic resonance imaging (MRI) presented with headaches and memory disturbance, with a swollen periorbital area on the left side of several months duration. MRI and computed tomography (CT) showed a large heterogeneous signal mass with central necrosis and pial involvement in the left frontal lobe, and adjacent bony destruction and parenchymal edema. There were also multiple other smaller well-enhancing nodular or lobulating contoured nodules in both the frontal and parietal bones. The skull X-ray showed identical multiple punched-out-like radiolucent lesions in both the frontal and parietal bones (Fig. 1). Laboratory results revealed the following: serum protein electrophoresis revealed IgA-kappa monoclonal gammopathy, beta-2 microglobulin was in the normal range (1.8 mg/L), kappa free light chain levels were elevated to 23.5 mg/L, and IgA levels were increased to 2,408.7 mg/dL (Table 1, Fig. 2). Also, the albumin level was low continuously (<3 g/dL), otherwise there were no other abnormal laboratory findings in the serum and urine samples. Therefore, the multiple myeloma staging of the patient was Stage II according to the International Staging System, and Stage III-A in Durie-Salmon staging system. The frozen biopsy demonstrated plasma cell neoplasm in the tumor, bone, and muscle during the orbitozygomatic craniotomy (Fig. 3). Final biopsy reported that bone, tumor tissues revealed portions of undifferentiated neoplasm composed of numerous plasmacytic small cells with eccentric nuclei of cartwheel pattern, the cytoplasm is eosinophilic with perinuclear clearing and some immature cells or multinucleated cells are present with multiple plasma cell. However, the positron emission tomography (PET)-CT and bone scan did not show any other systemic lesions except in the brain. External lumbar drainage during the 5 days of admission relieved the fluid collection underneath the scalp. She was treated with eight cycles of Melphalan and prednisolone, and about 1 year later after surgery, the follow-up laboratory results were as follows: beta-2 microglobulin was in the normal range (2.4 mg/L), kappa free light chain levels were elevated to 40.5 mg/L, and IgA levels were increased to 844 mg/dL (Table 1).
Multiple myeloma is a hematological malignancy characterized by a monoclonal proliferation of plasma cells. Patients may present with spinal cord or root compression as a result of vertebral collapse or extradural lesions [3]. Occasionally, patients present with polyneuropathy secondary to amyloidosis or as part of the POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes) [4]. Meningeal involvement by a myeloma is an uncommon event, occurring in approximately 1% of cases of MM [5]. It may manifest as either a solitary cerebral lesion, intraparenchymal infiltration, or a diffuse leptomeningeal disease such as CNS myelomatosis. The mechanism of spread to the leptomeninges in a myeloma is unknown, although it is thought to be comparable to that of leukemic meningitis. Post-mortem examination of children with acute lymphoblastic leukemia has shown that leukemic involvement of the CNS first becomes apparent in the walls of superficial arachnoid veins and surrounding adventitia. With more advanced stages of leukemic infiltration, the arachnoid trabeculae are destroyed and leukemic cells are able to spill over into the cerebrospinal fluid (CSF), and are thus detectable on cytological examination. The mechanism of leptomeningeal spread in myeloma is likely to take place by a related mechanism [6].
Presenting signs and symptoms are often generalized and may include lethargy, nausea, vomiting, headaches, confusion, paresthesias, and seizures as well as visual, gait, and speech disturbances [7]. Patients with myelomatous meningeal involvement usually present with diffuse leptomeningeal infiltration, and the presence of plasma cells in the cerebrospinal fluid [8]. An analysis of CSF can often distinguish a disease of the dura mater from leptomeningeal involvement. In patients with diffuse leptomeningeal infiltration, plasma cells are usually evident in the CSF, whereas in dural myeloma without parenchymal or leptomeningeal disease, plasma cells are not usually detected in the CSF.
Previous studies have reported 54 cases of MM with myelomatous meningeal involvement, and a male/female ratio of 1 : 2. The advanced stage of MM, with circulating plasma cells in the peripheral blood, suggested a hematogenous spread of tumor cells to the meninges. Unfortunately, imaging studies are often nonspecific, and the differential diagnosis includes metastasis, lymphoma, meningioma, dural granulocytic sarcoma, plasmacytoma, infectious meningitis, and leptomeningeal carcinomatosis [9]. A diagnosis of dural myeloma requires a histologic examination of tissue, although this may not be indicated if the patient already has a history of MM or a poor prognosis [7]. The prognosis associated with leptomeningeal infiltration by plasma cells is extremely poor, with a median survival of 1.5 to 3 months despite various treatments, including intrathecal and/or systemic chemotherapy and cranial radiotherapy. More rarely, a direct accumulation of plasma cells in the dura mater may present as an isolated mass without any leptomeningeal or cerebrospinal fluid diffusion. This solitary monoclonal plasma cell tumor arising from the dura mater has been identified as solitary dural plasmacytoma [10]. In our patient, there was no presence of any plasma cells in the five consecutive studies of CSF by postoperative external lumbar drainage for 5 days.
Because of its infrequency, no guidelines have been established for the treatment of patients with CNS MM. The treatment is similar to that of leukemias and aggressive lymphomas invading the CNS, and includes intrathecal chemotherapy or combination systemic chemotherapies that cross the blood-brain barrier, with or without cranial irradiation. Case reports using autologous and allogeneic stem cell transplantation in CNS myeloma reported disease remission of up to 12 months [5]. Systemic chemotherapy agents used with mostly transient responses include a combination of doxorubicin, cyclophosphamide, melphalan, cisplatin, and etoposide, bortezomib, and the immunomodulators thalidomide and lenalidomide. Except for cisplatin and etoposide, most of the other chemotherapeutic regimens used to treat CNS myelomatosis, including bortezomib and the immunomodulators thalidomide and lenalidomide, are not known to cross the blood-brain barrier, or there is insufficient information on their CNS penetration. Cranial irradiation appears to be transiently effective [2]. Our patient underwent surgery for the extensive intracranial involvement of MM, which did not show active lesions on the PET and bone scans. However, it is still necessary to evaluate the patient systemically with bone marrow biopsy for a better prognosis and differential diagnosis of the solitary dural plasmacytoma.
In conclusion, MM requires an accurate diagnosis and a CNS evaluation with MRI and other imaging as early as possible in order to define the meningeal or cerebral involvement. This would also aid in the use of optimized chemotherapeutic agents and radiation.
Figures and Tables
Fig. 1
Image study of the patient. A: Skull X-ray. Multiple punch out lesion was noted. B: T2 weighted magnetic resonance image (axial). Large heterogeneous signal mass with central necrosis and pial involvement is noted in left frontal lobe. Adjacent bony destruction and parenchymal edema are also noted. After contrast media injection, the mass shows strong enhancement. And multiple other smaller well-enhancing nodular or lobulating contoured nodules in both frontal and parietal bones are noted. C: Pre-operation brain computed tomography (CT). Relatively wall marginated bone destruction is noted in left frontal and parietal bones. D: Post-operation brain CT (bone setting image). Post-operative state, left frontal tumor removal and cranioplasty state with orbitozygomatic approach.
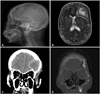
Fig. 2
Electrophoresis and Immunofixations. A: Serum electrophoresis. B: Urine electrophoresis. C: Serum Immunofixation. D: Urine Immunofixation, Serum and urine protein electrophoresis revealed monoclonal gammopathy, IgA kappa type, free kappa light chains.

References
1. Kyle RA. Multiple myeloma: review of 869 cases. Mayo Clin Proc. 1975; 50:29–40.
2. Turhal N, Henehan MD, Kaplan KL. Multiple myeloma: a patient with unusual features including intracranial and meningeal involvement, testicular involvement, organomegaly, and plasma cell leukemia. Am J Hematol. 1998; 57:51–56.

3. Somers LJ, Shaw B, Lyn BE, McMillan AM, Mahendra P. Meningeal myeloma in the absence of systemic disease, and as the initial feature of disease progression. Clin Lab Haematol. 1998; 20:189–190.

4. Peest D. [Multiple myeloma]. Ther Umsch. 1996; 53:147–151.
5. Fassas AB, Muwalla F, Berryman T, et al. Myeloma of the central nervous system: association with high-risk chromosomal abnormalities, plasmablastic morphology and extramedullary manifestations. Br J Haematol. 2002; 117:103–108.

6. Roddie P, Collie D, Johnson P. Myelomatous involvement of the dura mater: a rare complication of multiple myeloma. J Clin Pathol. 2000; 53:398–399.

7. Méndez CE, Hwang BJ, Destian S, Mazumder A, Jagannath S, Vesole DH. Intracranial multifocal dural involvement in multiple myeloma: case report and review of the literature. Clin Lymphoma Myeloma Leuk. 2010; 10:220–223.

8. Paul RH, Piatt AL, Whelihan WM, Malloy PF. Neuropsychological and magnetic resonance imaging abnormalities associated with a plasmacytoma of the frontal dura: a case report. Neuropsychiatry Neuropsychol Behav Neurol. 2000; 13:143–147.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download