Abstract
Objective
The aim of this study was to determine factors affecting the long-term survival of subjects with aortic aneurysm (AA).
Methods
We included 294 Korean patients aged ≥30 years who were hospitalized from 1994 through 2004. Diagnosis was confirmed in 267A subjects (75.8% with abdominal only AA (AAA) and 24.2% with thoracic AA (TAA)) by computed tomography angiography in Samsung Medical Center, Seoul, Korea. AA repair direct operation or percutaneous endovascular AA repair (Revascularized group) was performed in 60.3% of the total patients. Death data were obtained from all participants between 1994 and 2009.
Results
The mean age of AA subjects was 68.7 (±8.1) years. The proportion of males was 82%. Five- and 10-year survival rates were 89.8% and 82.6%, respectively. The 5- and 10-year survival rates were 92.3% and 84.9% in revascularized group and 86.4% and 79.5% in non-revascularized group, respectively. Adjusted hazard ratios were 1.11 {95% confidence interval (CI) 1.04-1.21} in ages and 3.07 (95% CI 1.26-7.90) in smoking for AA.
Mortality due to coronary artery disease (CAD) and cerebrovascular accident has increased worldwide over the past few decades. Atherosclerosis is the leading cause of cardiovascular disease (CVD) such as coronary and other atherosclerotic vascular disease. The increase in mortality has been attributed to an increase in the elderly population, a westernized life style, and/or increased chronic disease incidence.12 For the aforementioned reasons, more attention has recently been focused on the aortic disease.3 Although the incidence of aortic aneurysm (AA) has increased with the increase in the elderly population,4 few studies have reported the long-term survival of subjects with AA in Korea. Our objective in this study was to analyze factors affecting the long-term survival of subjects with AA.
We reviewed the records of patients diagnosed with AA at the Cardiac and Vascular Center, Samsung Medical Center, Seoul, Korea from 1994 through 2004. Subjects consisted of patients with AA (n=267, male=82%) including thoracic aortic aneurysm (TAA, n=52) and abdominal aortic aneurysm (AAA, n=215) confirmed by computed tomography (CT) angiography. TAA and AAA were defined as follows: TAA was AA affecting the thoracic aorta, regardless of abdominal aorta, while AAA was AA affecting only the abdominal aorta. Genetic aorta diseases such as Marfan syndrome and Loeys-Dietz syndrome were excluded. CAD in AA subjects was confirmed by cardiac catheterization, coronary CT, echocardiography, or positron emission tomography. AA repair direct operation or percutaneous endovascular AA repair (AA Revascularized group) (n=161) was performed. Information was obtained by reviewing electronic medical charts. This study was approved by the Samsung Medical Center institutional review board. Informed consent was waived for this retrospective study.
Subjects were defined as having hypertension (HT) if they were taking an anti-hypertension drug, had been clinically diagnosed with HT, or had either a systolic blood pressure (SBP) ≥140 mmHg or a diastolic blood pressure (DBP) ≥90 mmHg.5 Subjects who met one of the following requirements were defined as having diabetes mellitus (DM): taking an oral hyperglycemic agent, using insulin, clinical diagnosis of diabetes, or a fasting plasma glucose >125 mg/dL.5 Subjects were defined as dyslipidemia if they met one of the following requirements: diagnosis of hypercholesterolemia, medication history for hypercholesterolemia or total cholesterol (TC) >200 mg/dL or low density lipoprotein (LDL) >130 mg/dL.5 The criterion for obesity based on body mass index (BMI) was BMI ≥ 25.6 A patient who had smoked within a year prior to the study was defined as a smoker. The estimated glomerular filtration rate (eGFR), which is used as an indicator of kidney function, was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. The CKD-EPI equation is eGFR = 141 × min (serum Cr /κ, 1)α × max (serum Cr /κ, 1)-1.209 × 0.993Age × 1.018 [if female], where κ is 0.7 for females and 0.9 for males, α is -0.329 for females and -0.411 for males, min indicates the minimum of serum Cr /κ or 1, and max indicates the maximum of serum Cr /κ or 1. Multiplication factors for race and sex are incorporated into the intercept, which results in different intercepts for different age and sex combinations. The National Kidney Foundation Kidney Disease Outcome Quality Initiative defines chronic kidney disease (CKD) as an eGFR <60 mL/min/1.73m2.
General and clinical characteristics of AA subjects are reported as means±standard deviations (SD) for continuous variables and percentages for categorical variables. Kaplan-Meier analysis was used to plot survival curves for AA subjects. Kaplan-Meier method was also used to compare survival among patients with AA at different sites or in the presence of CAD using log-rank tests. Multiple cox proportional hazards analysis was carried out using the variables of age, gender, SBP, DBP, fasting plasma glucose, triglyceride, high density lipoprotein, eGFR, smoking, BMI, AA revascularized group, and AA maximum size.
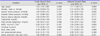
The mean age of AA subjects was 68.7 (±8.1) years. The proportion of patients older than 65 years was 70.8%. The proportion of males was 82%. The proportion of cardiovascular risk factors in the patient population was as follows: over 60% had HT, over 40% had dyslipidemia or were smokers, over 30% had CKD, and over 20% had DM or were obese. The proportion of CAD comorbidity was 19.9% (Table 1).
Five- and 10-year survival rates for all subjects were 89.8% and 82.6%, respectively. The 5- and 10-year survival rates were 90.2% and 83.3% for AAA patients and 86.4% and 76.8% for TAA patients, respectively (p=0.250). The 5- and 10-year survival rates were 88.7% and 81.9% in non-CAD subjects versus 92.6% and 86.6% in CAD subjects, respectively (p=0.490). And for AA revascularized group versus non-revascularized group, the 5- and 10-year survival rates were 92.3% and 84.9 % in AA revascularized group versus 86.4% and 79.5% in non-revascularized group, respectively (p=0.173) (Fig. 1).
Adjusted hazard ratios (HRs) of age was 1.11 {95% confidence interval [CI] 1.04-1.21} and adjusted HRs of smoking was 3.07 (95% CI 1.26-7.90) in smoking for AA subjects (Table 2). However, adjusted HRs of gender, SBP, DBP, fasting plasma glucose, triglyceride, high density lipoprotein, eGFR, BMI, AA revascularized group, and AA maximum size was not significant association.
The old age group and the current smoking group showed higher risk for death in AA patients. These findings are consistent with those of previous studies that smoking is a predictor for AA patients.78910 AA development was contributed endotherial cells.11 Endotherial cells respond to a number of stimulating factors such as smoking.12 Therefore, aggressive non-smoking education program should be applied in smoking AA patients. However, a study in an England cohort from 1997 through 2010 showed that smoking was not associated with cardiac death.13 Mechanism of underlying the association between older age and development of AA might be related to aortic wall changes. With aging, the vascular wall will gradually lose its elasticity, resulting in aortic dilatation from which mechanical forces will be conveyed to collagen within the aortic wall. Subsequent changes in collagen due to remodeling will lead to a stiffer and less compliant vessel.14 These findings differ from those for HT,89 DM,15 and BMI-defined obesity.9 Dyslipidemia16 and CKD may be involved in the pathophysiologic mechanism of development due to AA. In previous studies, calcium-channel blockers were an independent risk factor for the presence of an AAA and were associated with increased arterial aortic wall stiffness.17 Angiotensin-converting-enzyme inhibitors were associated with decreased stiffness and greater collagen turnover.17 And, beta-blockers may be used to slow the growth rate of an AA.18
The 5- and 10-year survival rates for Korean AA patients were over 80%. AA with CAD, AA without CAD, and AAA subjects also showed over 80% survival rate over 5 and 10 years. Patients with TAA had the lowest 10-year survival rate of 76.8%. Furthermore, the 5- and 10-year survival rates were 92.3% and 84.9% in AA revascularized group and 86.4% and 79.5% in non-revascularized group, respectively. In Korea, 21,301 echocardiography devices were available at 62,853 medical institutions registered with the National Health Insurance Service in 2013.19 This easy accessibility to clinics or hospitals and earlier health examination may have contributed to the higher AA survival rates in Korea. Also, it is important to educate patients and to follow AHA/ACC guidelines for secondary prevention, especially in those patients with coronary and other atherosclerotic vascular diseases in 2006.20
Our study showed the proportion of male patients was higher than that of female patients. This result is consistent with United States AAA study.21 Their study showed that the ratio of male vs female was 4:1. In addition, they revealed that female are protected from AAA formation not only in human22 but also in animal model.2324
This study had several limitations. First, the study was conducted retrospectively at a single center, which may have caused selection bias. We were also unable to eliminate the possibility of information bias when collecting medical records from the medical charts of the subjects and laboratory results. Second, we did not consider other CAD risk factors such as CRP,25 homocysteine,26 lipoprotein(a),27 fibrinogen,28 physical activity, nutrition, socioeconomic position, or health behavior variables in this study. Furthermore, we were unable to analyze smoking details because we grouped the patients only into current smoking and ex-smoker or none. Therefore, risk factors of atherosclerosis for prediction of CVD should be confirmed in further prospective cohort studies. We also suggest active non-smoking education program should be applied in smoking AA patients. Third, we could not separately analyze cox proportional hazard model for AAA and TAA due to their small sample size.
We found that age and smoking were associated with increased risk of death in AA patients in Korea. The proportion of male and older age was over two thirds, and the 10-year survival rate for AA patients in Korea was over 80%. Especially, the 10-year survival rates of AA revascularized group were over 85%.
Figures and Tables
 | Fig. 1Kaplan-Meier curves of (A) cumulative survival rates of all AA patients, (B) cumulative survival rates of AA patients with and without CAD (p=NS), (C) cumulative survival rates of TAA and AAA patients (p=NS), and (D) cumulative survival rates of AA patients with and without revascularization (p=NS). CAD; coronary artery disease. |
Table 1
General and clinical characteristics of subjects with aortic aneurysm (n=267)

Table 2
Associations between clinical variables and overall hazard ratios
References
2. Booth GL, Kapral MK, Fung K, Tu JV. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: a population-based retrospective cohort study. Lancet. 2006; 368:29–36.

3. Park YJ, Kim N, Kim YW. Investigation of Current Trend of AAA Treatment in Korea. J Korean Surg Soc. 2011; 80:125–130.

4. Grundy SM, Pasternak R, Greenland P, Smith S Jr, Fuster V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation. 1999; 100:1481–1492.

5. Jang SY, Ju EY, Cho SI, Lee SW, Kim DK. Comparison of cardiovascular risk factors for peripheral artery disease and coronary artery disease in the Korean population. Korean Circ J. 2013; 43:316–328.

6. Weisell RC. Body mass index as an indicator of obesity. Asia Pac J Clin Nutr. 2002; 11:Suppl 8. S681–S684.

7. Lee AJ, Fowkes FG, Carson MN, Leng GC, Allan PL. Smoking, atherosclerosis and risk of abdominal aortic aneurysm. Eur Heart J. 1997; 18:671–676.

8. Wong DR, Willett WC, Rimm EB. Smoking, hypertension, alcohol consumption, and risk of abdominal aortic aneurysm in men. Am J Epidemiol. 2007; 165:838–845.

9. Jahangir E, Lipworth L, Edwards TL, Kabagambe EK, Mumma MT, Mensah GA, et al. Smoking, sex, risk factors and abdominal aortic aneurysms: a prospective study of 18 782 persons aged above 65 years in the Southern Community Cohort Study. J Epidemiol Community Health. 2015; 69:481–488.

10. Wilmink TB, Quick CR, Day NE. The association between cigarette smoking and abdominal aortic aneurysms. J Vasc Surg. 1999; 30:1099–1105.

11. Guzik B, Sagan A, Ludew D, Mrowiecki W, Chwała M, Bujak-Gizycka B, et al. Mechanisms of oxidative stress in human aortic aneurysms--association with clinical risk factors for atherosclerosis and disease severity. Int J Cardiol. 2013; 168:2389–2396.

12. Siasos G, Mourouzis K, Oikonomou E, Tsalamandris S, Tsigkou V, Vlasis K, et al. The role of endothelial dysfunction in aortic aneurysms. Curr Pharm Des. 2015; 21:4016–4034.

13. Pujades-Rodriguez M, George J, Shah AD, Rapsomaniki E, Denaxas S, West R, et al. Heterogeneous associations between smoking and a wide range of initial presentations of cardiovascular disease in 1937360 people in England: lifetime risks and implications for risk prediction. Int J Epidemiol. 2015; 44:129–141.

14. Collins JA, Munoz JV, Patel TR, Loukas M, Tubbs RS. The anatomy of the aging aorta. Clin Anat. 2014; 27:463–466.

15. De Rango P, Farchioni L, Fiorucci B, Lenti M. Diabetes and abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2014; 47:243–261.

16. Celik T, Iyisoy A, Celik M, Tan Y. Dyslipidemia and abdominal aortic aneurysm: another piece of the puzzle? Int J Cardiol. 2010; 139:202–203.

17. Wilmink AB, Vardulaki KA, Hubbard CS, Day NE, Ashton HA, Scott AP, et al. Are antihypertensive drugs associated with abdominal aortic aneurysms? J Vasc Surg. 2002; 36:751–757.

18. Chun AS, Elefteriades JA, Mukherjee SK. Do betablockers really work for prevention of aortic aneurysms?: time for reassessment. Aorta (Stamford). 2013; 1:45–51.
19. Korean Statistical Information Service. Specific equipments by type of medical care institutions [Internet]. Daejeon: Statistics Korea;2014. accessed on 1 March 2017. Available from: http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE$parentId=D.
20. Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006; 113:2363–2372.

21. Hannawa KK, Eliason JL, Upchurch GR Jr. Gender differences in abdominal aortic aneurysms. Vascular. 2009; 17:Suppl 1. S30–S39.

22. Ailawadi G, Eliason JL, Roelofs KJ, Sinha I, Hannawa KK, Kaldjian EP, et al. Gender differences in experimental aortic aneurysm formation. Arterioscler Thromb Vasc Biol. 2004; 24:2116–2122.

23. Lee JK, Borhani M, Ennis TL, Upchurch GR Jr, Thompson RW. Experimental abdominal aortic aneurysms in mice lacking expression of inducible nitric oxide synthase. Arterioscler Thromb Vasc Biol. 2001; 21:1393–1401.

24. Manning MW, Cassi LA, Huang J, Szilvassy SJ, Daugherty A. Abdominal aortic aneurysms: fresh insights from a novel animal model of the disease. Vasc Med. 2002; 7:45–54.

25. Fortmann SP, Ford E, Criqui MH, Folsom AR, Harris TB, Hong Y, et al. CDC/AHA workshop on markers of inflammation and cardiovascular disease: application to clinical and public health practice: report from the population science discussion group. Circulation. 2004; 110:e554–e559.

26. Fakhrzadeh H, Ghotbi S, Pourebrahim R, Nouri M, Heshmat R, Bandarian F, et al. Total plasma homocysteine, folate, and vitamin B12 status in healthy Iranian adults: the Tehran homocysteine survey (2003–2004)/a cross-sectional population based study. BMC Public Health. 2006; 6:29.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download