Abstract
We report a rare case of bilateral renal infarction resulting in acute renal failure in a previously healthy 26-year-old soldier. The patient presented with an abdominal pain and bilateral costovertebral angle tenderness. Laboratory studies showed elevated serum creatinine, mild leukocytosis, and increased lactate dehydrogenase. Contrast-enhanced computed tomography showed multiple perfusion defects in both kidneys with wedge-shaped infarction in right kidney. Kidney biopsy performed in the left kidney revealed microinfarction. Comprehensive work-up did not reveal any specific causes or risk factors except smoking, and the infarction was considered to be idiopathic. He emphasized that he received extremely strenuous military training several days before he came to the hospital. He was treated with low molecular weight heparin with significant improvement in renal function. Further studies are needed for the characterization of idiopathic renal infarction in previously healthy individuals and evaluating the mechanisms including strenuous physical activity on the renal blood flow.
Infarction of the kidney is a rather uncommon condition that can result from obstruction or decrease of the renal arterial flow. In the majority of cases, the etiology is a thromboembolic phenomenon, and the risk factors of thromboembolic event are atrial fibrillation, valvular heart disease, heart failure, or aortic aneurysm.1 Actually, cardiac conditions such as atrial fibrillation and ischemic or valvular heart disease are known to be the most common causes of renal infarction (RI), and other frequent etiologies include atherosclerosis, renal artery fibrodysplasia, and renal artery dissection.123
Rarely, idiopathic RI may occur in patients without apparent risk factors for thromboembolism or vascular disease, and a few cases have been reported.456
We report a 26-year-old man who developed bilateral RI associated with acute renal failure (ARF) of unknown cause.
A 26-year-old male presented to the emergency department (ED) with a chief complaint of epigastric pain persisting more than 24hr. He denied fever, diarrhea, or trauma. He had no specific medical history, and worked as a professional soldier. He visited the ED the day before with a chief complaint of general weakness and abdominal discomfort, and discharged after little relief after intravenous (IV) hydration. Physical examination showed vital signs as follows: body temperature of 37.1℃, blood pressure of 140/90 mmHg, and heart rate of 100 beats per minute. The patient's abdomen was soft and depressible, with slight tenderness in bilateral costovertebral angles (CVA). Results of laboratory tests revealed the following measurements : white blood cell (WBC) count, 12,600 cells/mm3; hemoglobin, 15.0 g/dL; hematocrit, 44.0%; platelet count, 157×103/mm3; CRP 4.67 mg/dL; blood urea nitrogen (BUN), 12.9 mg/dL; and creatinine, 2.0 mg/dL. A serum analysis done one day previously showed that his creatinine level was 1.0 mg/dL. The serum electrolytes, liver function profiles, and Amylase/Lipase levels were normal. Urinalysis was weakly positive for protein, and microscopically showed 20-29 red blood cells per high-power field (HPF), 0-2 WBCs per HPF, and negative for bacteria. Helical unenhanced computed tomography (CT) failed to show nephrolithiasis or other abnormalities.
He was admitted to the hospital for diagnostic evaluation and pain control. Initial treatment included IV hydration and antibiotics, with incomplete pain relief. Plasma BUN and creatinine increased to 23.7 mg/dL and 4.0 mg/dL, respectively, on the following day. Serum lactate dehydrogenase (LDH) was examined and increased to 564 IU/L (reference range 263~450 IU/L). Due to the persistent abdominal pain and creatinine elevation, we performed an abdominal contrast-enhanced helical CT on day 3 in order to rule out other intra-abdominal disease including RI. CT demonstrated mild enlargement, multiple perfusion defects and delayed contrast excretion in bilateral kidneys with small wedge-shaped infarction in right kidney with no lithiasis or dilatation of urinary tract (Fig. 1). CT revealed normal abdominal aorta and renal arteries. Since CT findings showing focal infarction could not explain the cause of ARF sufficiently, we performed a renal biopsy at the left kidney in order to get further information on ARF of unknown origin. Biopsy revealed renal microinfarct, showing severe necrosis of podocytes which are entirely detached from the glomerular basement membrane, loss of nuclei and ballooning degeneration of tubular epithelial cells, and severe interstitial hemorrhage in the medulla (Fig. 2). Together with the CT findings, biopsy, elevated LDH, and the clinical features of the patient, this was suggestive of bilateral RI with ARF, although most areas showed hypoperfusion rather than typical wedge-shaped infarction in CT imaging.
Although CT revealed no thrombus in vasculature, we performed a transthoracic echocardiogram, transesophageal echocardiography, and 48 hour Holter monitoring in order to find out the cause of RI, and no structural or arrhythmic heart disease could be detected. A blood analysis showed near normal prothrombin time 14.3 sec (reference range 11.9-13.9) and normal activated partial thromboplastin time of 37.2 sec, with a d-dimer concentration of 567.6 ng/dL. Hypercoagulable workup, including factor V, protein C, protein S, anticardiolipin antibody, and antiphospholipid antibody, was negative. The parameters for complements and autoimmune disease were negative. Serum creatinine peaked at 5.6 mg/dL. The serum liver function and lipid profile remained normal. Since the patient lacked associated co-morbid conditions, and comprehensive work-up failed to reveal the etiology of his RI except smoking, he was diagnosed as idiopathic RI. He told that he received extremely strenuous military training several days before he came to the hospital.
Besides continuous intravenous hydration, anticoagulation with enoxaparin was initiated immediately after contrast-enhanced CT was done. His abdominal pain and nausea improved 4-5 days after admission. Systolic blood pressure improved from 140s to 120s mmHg spontaneously. Serum creatinine decreased to 3.2 mg/dL after 6 days after admission. At day 10 after admission, serum creatinine was 1.2 mg/dL and there was no proteinuria or hematuria. Low dose aspirin was prescribed at discharge.
We presented a case of bilateral RI, a rare cause of acute kidney injury, in a previously healthy young male from unknown cause. The patient described above presented with abdominal pain, bilateral CVA tenderness, and slightly elevated blood pressure. Laboratory examination revealed ARF, elevated LDH, normal liver function, mild leukocytosis, and microscopic hematuria which are consistent with RI. Contrast enhanced CT showed a wedge-shaped unequivocal infarction at right kidney with multiple perfusion defects in bilateral kidneys. Kidney biopsy of left kidney revealed microinfarction. In the present case, substantial portion of the ischemic damage seems to be reversible, given the near normal serum creatinine at discharge.
The diagnosis of acute RI is often missed or delayed due both to the rarity of the disease and its non-specific clinical presentation. Diagnosing RI could be overlooked, particularly, in young individuals who may lack traditional risk factors for RI, and in whom conditions that present similarly to RI are relatively common such as lumbago of musculoskeletal origin, nephrolithiasis, or acute abdominal disease. Recognizing and diagnosing RI is important, however, due to both the severity of potential underlying causes and the associated risk of chronic kidney disease and mortality.
The mechanisms of RI are various, mainly thrombotic and embolic. Several reports investigating the clinical features of RI have suggested that most patients have risk factors for thromboembolism from cardiac origin and atheromatous disease.7 Other etiologies include renal trauma (renal artery dissection), renal vascular disease (such as fibromuscular dysplasia and vasculitis), and hypercoagulability (thrombophilia, sickle cell disease).1238 Bilateral infarction, in particular, is rare, and was reported to be found in dissecting aneurysms of the aorta, septic emboli from endocarditis, lupus, hypercoagulable state, or with fibromuscular dysplasia of the renal arteries.910111213
Recently, idiopathic RI without any underlying disease was reported. In the present case, also, comprehensive work-up did not reveal any specific causes or risk factors except smoking, and the infarction was considered to be idiopathic. Bolderman et al reported 16 case series of idiopathic RI.14 These patients were younger (median age 48 years) compared to those with cardiogenic RI and, except for smoking, had fewer traditional cardiovascular risk factors.
Actually, in 4 recent case series published between 2002 and 2013, 10.0~30.8% of cases of RI were classified as idiopathic.12315 Co-morbidities were often present in idiopathic RI cases, such as preexisting hypertension, hyperlipidemia, and smoking. It is not known, however, so far why RI occurs in those patients. Although little is known on the correlation of smoking and RI, smoking appears to be a risk factor of idiopathic RI. Bolderman et al reported that 75% of patients with idiopathic RI were smokers, and the patient in the present case was also a smoker. It could be assumed that strenuous physical activity might have triggered the development of RI in the patient with risk factors such as smoking in the present case. It is likely that acute RI has been underreported so far, and the increased use of CT nowadays lead to the shift in the epidemiologic spectrum toward the idiopathic form. More study is needed to better characterize idiopathic RI which occur in individuals who lack associated co-morbid conditions and to evaluate the mechanisms including various situations such as extreme strenuous physical activity on the renal blood flow and the effect on ischemic damage.
RI can occur in otherwise healthy individuals, and the possibility of acute RI should be suspected in persistent abdominal pain and AKI, after more common causes such as nephrolithiasis have been excluded, even in patients without apparent risk factors for infarction.
Figures and Tables
Fig. 1
Contrast-enhanced abdominal computed tomography (CT). (A) Arterial phase, (B) Delayed phase, CT demonstrated mild enlargement, multiple perfusion defects and delayed contrast excretion in bilateral kidneys with unequivocal wedge-shaped infarction in right kidney.
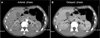
Fig. 2
Renal biopsy findings. (A) Light microscopy (×10). In the renal cortex, patch microinfarction is shown with loss of nuclei and ballooning degeneration of tubular epithelial cells (not shown). In the medulla, severe interstitial hemorrhage is also shown, (B) Transmission electron microscopy (TEM) (×5000). Ultrastructurely, glomerular cells, particularly podocytes, exhibit severe necrosis, entirely detached from the glomerular basement membrane.

References
1. Korzets Z, Plotkin E, Bernheim J, Zissin R. The clinical spectrum of acute renal infarction. Isr Med Assoc J. 2002; 4:781–784.
2. Antopolsky M, Simanovsky N, Stalnikowicz R, Salameh S, Hiller N. Renal infarction in the ED: 10-year experience and review of the literature. Am J Emerg Med. 2012; 30:1055–1060.

3. Bourgault M, Grimbert P, Verret C, Pourrat J, Herody M, Halimi JM, et al. Acute renal infarction: a case series. Clin J Am Soc Nephrol. 2013; 8:392–398.

4. Racusin JS, Pollack ML. Idiopathic renal infarction in a young woman. Am J Emerg Med. 2005; 23:397–398.

5. Joulin V, Sallusto F, Deruelle C, Taccoen X, Valeri A, Fournier G. Idiopathic acute partial renal infarction. Prog Urol. 2005; 15:75–77.
6. Eickhoff C, Mei JM, Martinez J, Little D. Idiopathic renal infarction in a previously healthy active duty soldier. Mil Med. 2014; 179:e259–e262.

7. Tsai SH, Chu SJ, Chen SJ, Fan YM, Chang WC, Wu CP, et al. Acute renal infarction: a 10-year experience. Int J Clin Pract. 2007; 61:62–67.

8. Paris B, Bobrie G, Rossignol P, Le Coz S, Chedid A, Plouin PF. Blood pressure and renal outcomes in patients with kidney infarction and hypertension. J Hypertens. 2006; 24:1649–1654.

9. Manfredini R, La Cecilia O, Ughi G, Kuwornu H, Bressan S, Regoli F, et al. Renal infarction: an uncommon mimic presenting with flank pain. Am J Emerg Med. 2000; 18:325–327.

10. Yen TH, Chang CT, Ng KK, Wu MS. Bilateral renal infarction in chronic myelomonocytic leukemia on blast crisis. Ren Fail. 2003; 25:1029–1035.

11. Bouassida K, Hmida W, Zairi A, Hidoussi A, Jaidane M, Slama A, et al. Bilateral renal infarction following atrial fibrillation and thromboembolism and presenting as acute abdominal pain: a case report. J Med Case Rep. 2012; 6:153.

12. Padilla-Fernández B, García-Casado D, Martín-Izquierdo M, Manzano-Rodríguez C, García-García J, Lorenzo-Gómez MF. Bilateral renal infarction in a lupus patient: an unusual pathology. Clin Med Insights Case Rep. 2013; 6:87–91.

13. González-Moreno J, Campins MA, Buades JM. Fibromuscular dysplasia presenting with asymptomatic bilateral renal infarctions. Int Urol Nephrol. 2014; 46:243–246.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download